Introduction
In recent decades, the use of active, “student-centred” learning methods has become a strong trend across higher education institutions worldwide. Problem-Based Learning (PBL) was first introduced in the late 1960s and has been adopted as an educational strategy, particularly in the health sciences, and more specifically in nursing education since the 1980s (Wosinski et al., 2018). In nursing education, a paradigm shift has occurred from “teacher-centred” to “student-centred” learning, where the students are encouraged to actively seek knowledge (Zhang & Wilkinson, 2014).
According to Rodrigues et al. (2024), active methodologies such as PBL foster the development of professionals who are active, critical, reflexive, and ethical, with greater responsibility and commitment to achieving learning outcomes.
PBL is an active methodology that places the students at the centre of the educational process, promoting the development of essential competences for nursing practice (Jamshidi et al., 2021). By working through real and/or simulated problem situations, students could apply critical thinking, problem-solving, and evidence-based decisions, which are shown to be indispensable non-instrumental skills for the challenges of healthcare providing (Pires et al., 2017).
In this context, PBL encourages a holistic approach to care, enabling future nurses to understand the individual as a whole and to proactively identify real and potential health risks (Rodrigues et al., 2024; Sardo & Dal Sasso, 2008). Furthermore, it promotes teamwork, communication skills, and learning autonomy (Li et al., 2019).
Thus, through the implementation of this methodology, students become better prepared to handle complex clinical scenarios, fostering a safe, humanized, and evidence-based practice. Moreover, the adoption of PBL shifts the educational focus from “what to teach” to “what to learn” (Sardo & Dal Sasso, 2008).
1. Theoretical framework
PBL is an active educational method focused on the comprehension or resolution of a problem proposed by students or educators, under the guidance of a tutor (Jamshidi et al., 2021). This approach is “student-centred” and typically implemented in small groups, where real-world scenarios serve as stimuli for a deeper understanding of theoretical and practical concepts (Allert et al., 2022).
Beyond acquiring new knowledge related to the problem, PBL is one of the teaching methods used to develop essential professional skills in nursing, such as self-directed and collaborative learning (Wosinski et al., 2018).
In this model, students study independently and take responsibility for their own learning, including planning, implementation, and evaluation of their academic work (Putri & Sumartini, 2021). Self-directed learning includes identifying: 1) self-learning needs; 2) what is important to learn; and 3) appropriate learning resources.
Thus, PBL is a “student-centred” pedagogical method in which students and teachers act as co-responsible partners in the teaching-learning process, with teaching as a resource to facilitate learning (Ku & Ha, 2016). According to Jamshidi et al. (2021), the goal of this method in health education is to acquire basic clinical knowledge, enhance personal learning skills, effectively manage care-related challenges, and finally increase learning motivation and engagement (Üstün, 2006). Therefore, PBL is recognised as an approach that strengthens nursing education by teaching students to apply theory to clinical practice and developing their problem-solving skills, which can be used to overcome environmental constraints in clinical settings (Shin & Kim, 2013).
Group learning provides students with the opportunity to exchange ideas, develop effective communication and interpersonal skills, engage in teamwork, and cultivate group management and collaboration abilities (Zhang & Wilkinson, 2014). It creates a space to share, compare, and debate the information that they have found and learned, promoting the development of their clinical judgement skills. The development of positive interpersonal relationships and effective partnerships promotes the acquisition of leadership skills essential for addressing healthcare challenges in a controlled and safe environment (Allert et al., 2022).
Furthermore, by working in small groups, students develop collaborative learning skills, facilitating social and cultural interaction among individuals of diverse age groups, ethnic backgrounds, and socioeconomic statuses (Ku & Ha, 2016). They also learn to listen and to respect their peers' perspectives, record conclusions drawn from group discussions, critically appraise specialised literature, learn independently, use learning resources effectively, and develop oral presentation and public speaking skills (Putri & Sumartini, 2021). Allert et al. (2022) further emphasise that this methodology significantly enhances the moral development of nursing students compared to traditional education methods. Overall, these skills and attitudes are vital assets for lifelong learning (Putri & Sumartini, 2021).
According to Ku and Ha (2016), when confronted with a nursing problem, students use their theoretical knowledge to analyse the data presented and make informed judgments about the situation, which may result in nurse diagnoses, care plans, outcomes, and more. Moreover, the process encourages students to evaluate others' perspectives, preparing them to become responsible and engaged citizens, an aspect that will improve the nurse-patient relationship.
PBL offers a more holistic perspective on problems, contextualized within the healthcare environment and, more specifically, structured around the core concepts of the nursing metaparadigm (person, environment, health, and nurse) (Zhang & Wilkinson, 2014). In this regard, PBL addresses each problem with a focus on the individual, the specific environment that affects their health, the health-related issues involved, and the nursing approaches implemented to promote the individual’s health.
According to Ku and Ha (2016), based on Schmidt’s Model, students should follow seven sequential steps when applying PBL: (1) Clarify and agree on the definitions of unclear terms and concepts; (2) Define the problem(s); (3) Analyse the problem through group discussion strategies; (4) Formulate hypotheses by agreeing on possible explanations for the problem and analysing the information presented; (5) Generate and prioritise learning objectives; (6) Research to meet the learning objectives (self-directed study); and (7) Synthesise and apply the newly acquired data to the problem.
Critical thinking is a fundamental skill required for nurses, in addition to integrating theoretical knowledge and clinical interventions. In this sense, through the application of critical thinking, specific nursing knowledge, and the execution of techniques and interventions, students progressively develop interpersonal, instrumental, and systemic competences, as defined by the “Regulamento do Perfil de Competências do Enfermeiro de Cuidados Gerais” (Registered Nurse Competence Profile Regulation) (Ordem dos Enfermeiros, 2012). PBL has proven to be a pedagogical strategy that effectively promotes the development of critical thinking skills among nursing students (Wei et al., 2024).
According to “Ordem dos Enfermeiros” (2012, p. 7), the certification of Registered Nurse competences “ensures that the nurse holds a set of knowledge, skills, and abilities applied in clinical practice, which enables them to assess the health needs of the target population and act across all life contexts and levels of prevention.” The core competence domains of the Registered Nurse include professional, ethical, and legal responsibility, care provision and management, and professional development.
In nursing, the learning process (along with the socialisation necessary to develop a professional identity) involves the adoption of the standards and norms of the professional group. Nursing students are therefore socialised into professionalism throughout their training, and are expected to integrate the attributes of professionalism into their daily practice (Rudberg et al., 2022). In the context of nursing education in Portugal, students are encouraged to develop the Registered Nurse competences through a variety of learning strategies over the course of their academic training.
In this sense, according to Allert et al. (2022), PBL may serve as a methodological resource that facilitates a more effective and gradual transition from the educational phase to clinical practice, helping to overcome the challenges commonly faced by students during this transition.
With the potential contributions of PBL to the development of competences related to the provision and management of care by future Registered Nurses in mind, the present study aims to analyse the perceptions of undergraduate nursing students regarding the role of PBL in developing the competencies encompassed in the “Care Provision and Management” domain (B) of the Registered Nurse competence profile, as defined by “Ordem dos Enfermeiros”.
2. Methods
This was a prospective, quantitative, descriptive, and cross-sectional study conducted at a Higher Education Institution located in the Central Region of Portugal. Data collection was carried out at the end of the first semester of the 2023-2024 academic year.
By implementing the PBL strategy, we adopted the guidelines proposed by McMaster University (McMaster University, 2025), in Canada, and Maastricht University (Maastricht University, 2025), in the Netherlands.
This approach enabled the construction of an educational practice centred on the student (regarded as an active subject responsible for their own learning process) supported by the teacher/tutor (who plays a mediating and facilitating role in the teaching-learning process), that allows the transition from “What to teach” to “What to learn” (Sardo & Dal Sasso, 2008).
Accordingly, the guidelines for group work and the steps of the tutorial process included: (1) Identifying unclear terms and concepts within the case description; (2) Exploring the situation by establishing priorities and identifying relevant knowledge domains: biological, psychological, sociocultural, and spiritual, with a focus on the learning objectives; (3) Analysing and clarifying the problems based on the mobilisation of prior knowledge, both individually and collectively; (4) Systematising the analysis and developing explanatory hypotheses based on the data presented in the scenario; (5) Formulating learning questions based on individual and/or group needs; (6) Acquiring new knowledge by identifying and using appropriate learning resources; (7) Sharing new knowledge with the group regarding the problems, supported by solid scientific evidence, and synthesising the knowledge constructed; (8) Assessment (self-assessment, peer assessment, tutor assessment, and group work assessment) (Jamshidi et al., 2021).
2.1 Sample
The study sample was obtained through convenience sampling and consisted of 96 undergraduate nursing students from a Portuguese higher education institution. These students conducted a critical and reflexive analysis of a problem-based scenario of adult and elderly care for medical respiratory conditions (2nd year students) or post-operative care for orthopaedic surgical interventions (3rd year students).
Inclusion criteria were defined as: students who had attended both Medical-Surgical Nursing course units and had chosen the discrete assessment method (which included a group-based critical and reflective analysis of a problem-based situation). Students who opted for a final exam-based assessment were excluded from the study.
2.2 Data Collection Procedures
Data were collected through an online digital platform (FormsUA) composed by two sections: the first section gathered sociodemographic information (sex, age, course year, and attendance regime), while the second section asked students to rate competence criteria related to Competences B1, B2, B3, and B5 of the "Care Provision and Management" domain from the Registered Nurse Competence Profile (Ordem dos Enfermeiros, 2012) (see Figure 1). Ratings were provided using a scale from 0 to 2, according to the perceived contribution of PBL to the development of each competence criterion (0 indicating no contribution, and 2 indicating good/excellent contribution).
It is important to refer that, although the Registered Nurse Competence Profile (Ordem dos Enfermeiros, 2012) includes other domains, the domains “Professional, Ethical and Legal Responsibility” (A) and “Professional Development” (C) were not assessed in this study, as the competences within those domains are more typically developed in clinical practice contexts. Similarly, the competence criteria corresponding to Competences B4, B6, and B7 within the “Care Provision and Management” domain were also not evaluated, as their development is more closely linked to nursing clinical practice settings.
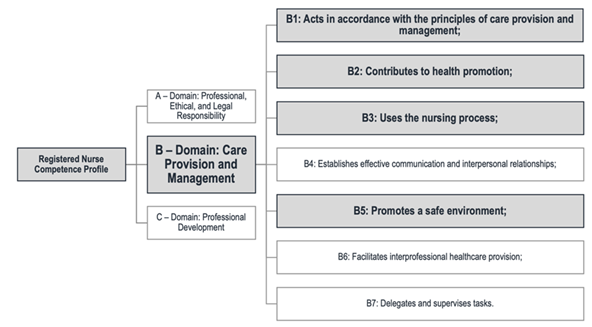
Figure 1 Domain of the provision and management of care in the Registerd Nurse Competence Profile (based on Ordem dos Enfermeiros, 2012).
Data collection was conducted online, where the competence criteria from the Registerd Nurse Competence Profile (Ordem dos Enfermeiros, 2012) were presented along with a Likert-type scale ranging from 0 to 2. Students were asked to “rate” the development of each competence criterion following the implementation of the PBL methodology.
Institutional authorisation was obtained to carry out the project, which was framed within pedagogical innovation strategies and outcomes monitoring. Prior to data collection, informed, voluntary, and explicit consent was obtained from all participants. Agreement to participate was formally indicated by a required selection on an introductory page of the online form, where students had to confirm their consent before proceeding to the questionnaire section. Anonymity and confidentiality of the collected data were fully ensured using numerical coding for organising the completed forms.
This pedagogical experience was integrated into an educational innovation initiative promoted by the University of Aveiro, titled the “Teaching and Pedagogical Training Program” (Universidade de Aveiro, 2024). This program encourages faculty members to implement active teaching-learning methodologies within their courses and curricular units, and to share the outcomes of best practices and excellent educational experiences with the academic and scientific communities. It is also worth noting that all activities conducted under this project actively promote voluntary student involvement in the process of diagnosing pedagogical change, defining strategies, and supporting implementation.
2.3 Statistical Analysis
This study was based on a descriptive statistical analysis performed by using the software Statistical Package for the Social Sciences (SPSS), version 28. Given the study’s objective and its descriptive nature, categorical variables were analysed using absolute and relative frequencies, which are presented in tabular format.
3. Results
The sample in this study was predominantly composed of female students (85.4%), with 20 years or younger (67.7%), and a mean age of 21.2 years (Table 1). The third-year students were the most representative group (61.5%), and the majority were enrolled in the course on a full-time basis (89.6%).
Table 1 Socio-demographic characterisation of study participants (n=96)
| Socio-demographic variable | N | % |
|---|---|---|
| Sex | ||
| Male | 14 | 14,6 |
| Female | 82 | 85,4 |
| Age (years) | ||
| ≤20 | 65 | 67,7 |
| ≥ 21 | 31 | 32,3 |
| Year of Nursing Degree Course | ||
| 2nd year | 37 | 38,5 |
| 3rd year | 59 | 61,5 |
| Attendance regime | ||
| Ordinary | 86 | 89,6 |
| Working Student | 9 | 9,4 |
| Student Athlete | 1 | 1 |
Regarding Competence B1: "Acts in accordance with the principles of care provision and management", students reported that PBL contributed most significantly to the good/excellent development of the following competence criteria: "Applies critical thinking and problem-solving techniques" (93.8%), "Makes well-founded judgments and decisions in any care context" (85.4%), and "Provides justification for the nursing care provided" (86.5%) (Table 2).
Conversely, the competence criteria, which in the students’ opinion, were least developed through the PBL strategy include: "Demonstrates an understanding of emergency plans for catastrophe situations" (36.5%), "Initiates and participates in discussions about innovation and change in nursing and healthcare" (11.5%), and "Acts as a resource for individuals, families, and communities facing health, disability, or end-of-life challenges" (10.4%) (Table 2).
Table 2 Results of the scores awarded by students for Competence B1: Acts in accordance with the principles of care provision and management (n=96)
| Competence Criteria | N (%) | ||
|---|---|---|---|
| Does not develop | Satisfactory development | Good/excellent development | |
| (20) - Applies the most appropriate knowledge and techniques in nursing practice. | 1 (1,0) | 18 (18,8) | 77 (80,2) |
| (21) - Incorporates valid and relevant research findings and other evidence into practice. | 2 (2,1) | 27 (28,1) | 67 (69,8) |
| (22) - Initiates and participates in discussions about innovation and change in nursing and healthcare. | 11 (11,5) | 33 (34,4) | 52 (54,2) |
| (23) - Applies critical thinking and problem-solving techniques. | 0 (0,0) | 6 (6,3) | 90 (93,8) |
| (24) - Makes well-founded judgments and decisions in any care context. | 2 (2,1) | 12 (12,5) | 82 (85,4) |
| (25) - Provides justification for the nursing care provided. | 0 (0,0) | 13 (13,5) | 83 (86,5) |
| (26) - Organises their work, managing time effectively. | 9 (9,4) | 32 (33,3) | 55 (57,3) |
| (27) - Demonstrates an understanding of the legal processes associated with healthcare. | 6 (6,3) | 36 (37,5) | 54 (56,3) |
| (28) - Acts as a resource for individuals, families, and communities facing health, disability, or end-of-life challenges. | 10 (10,4) | 39 (40,6) | 47 (49,0) |
| (29) - Presents information clearly and succinctly. | 2 (2,1) | 21 (21,9) | 73 (76,0) |
| (30) - Interprets objective and subjective data and their meanings appropriately, with a view to providing safe care. | 0 (0,0) | 22 (22,9) | 74 (77,1) |
| (31) - Demonstrates an understanding of emergency plans for catastrophe situations. | 35 (36,5) | 40 (41,7) | 21 (21,9) |
Caption: Competence indicators and most relevant values in bold.
Regarding Competence B2: "Contributes to health promotion", 91.7% of students rated PBL as a good/excellent contribution to the development of the competence criteria "Views the individual, family, and community from a holistic perspective that considers the multiple determinants of health" and "Recognises the potential of health education in nursing interventions" (Table 3).
In contrast, within this same competence, students reported limited development in the following criteria: "Demonstrates an understanding of health and social policies" (22.9%), "Demonstrates an understanding of traditional health belief systems and practices of individuals, families, or communities" (12.5%), and "Works in collaboration with other professionals and communities" (11.5%) (Table 3).
Table 3 Results of the scores awarded by students for Competence B2: Contributes to health promotion (n=96)
| Competence Criteria | N (%) | ||
|---|---|---|---|
| Does not develop | Satisfactory development | Good/excellent development | |
| (32) - Demonstrates an understanding of health and social policies. | 22 (22,9) | 45 (46,9) | 29 (30,2) |
| (33) - Works in collaboration with other professionals and communities. | 11 (11,5) | 30 (31,3) | 55 (57,3) |
| (34) - Views the individual, the family and the community from a holistic perspective that considers the multiple determinants of health. | 2 (2,1) | 6 (6,3) | 88 (91,7) |
| (35) - Participates in health promotion and disease prevention initiatives, contributing to their evaluation. | 4 (4,2) | 24 (25,0) | 68 (70,8) |
| (36) - Applies knowledge of existing resources for health promotion and education. | 2 (2,1) | 18 (18,8) | 76 (79,2) |
| (37) - Acts to empower the individual, the family and the community to adopt healthy lifestyles. | 5 (5,2) | 17 (17,7) | 74 (77,1) |
| (38) - Provides relevant health information to help individuals, families and communities achieve optimum levels of health and rehabilitation. | 3 (3,1) | 19 (19,8) | 73 (76,0) |
| (39) - Demonstrates an understanding of traditional health belief systems and practices of individuals, families, or communities. | 12 (12,5) | 37 (38,5) | 47 (49,0) |
| (40) - Provides support/education in the development and/or maintenance of independent living skills. | 2 (2,1) | 25 (26,0) | 69 (71,9) |
| (41) - Recognises the potential of health education in nursing interventions. | 0 (0,0) | 8 (8,3) | 88 (91,7) |
| (42) - Applies knowledge of teaching and learning strategies in interactions with individuals, families and communities. | 3 (3,1) | 26 (27,1) | 67 (69,8) |
| (43) - Evaluates learning and understanding about health practices. | 2 (2,1) | 21 (21,9) | 73 (76,0) |
Caption: Competence indicators and most relevant values in bold.
For Competence B3: "Uses the Nursing Process", 86.5% of participants reported that PBL contributed in a good/excellent manner to the development of the criterion "Documents the implementation of interventions", and 85.4% indicated the same level of contribution for "Documents the care process" (Table 4).
On the other hand, it is noteworthy that 30.2% of students stated that PBL did not contribute to the development of the following competence criteria: "Responds effectively in emergency or catastrophe situations" (30.2%), "Consults relevant members of the health and social care team" (11.5%), and "Responds effectively in unexpected or rapidly changing situations" (11.5%).
Table 4 Results of the scores awarded by students for Competence B3: uses the nursing process (n=96)
| Competence Criteria | N (%) | ||
|---|---|---|---|
| Does not develop | Satisfactory development | Good/excellent development | |
| (44) - Systematically assesses the data relevant to the design of nursing care. | 0 (0,0) | 25 (26,0) | 71 (74,0) |
| (45) - Analyses, interprets and documents data accurately. | 4 (4,2) | 20 (30,2) | 63 (65,6) |
| (46) - Formulates a care plan, whenever possible, in collaboration with clients and/or caregivers. | 4 (4,2) | 16 (16,7) | 76 (79,2) |
| (47) - Consults relevant members of the health and social care team. | 11 (11,5) | 31 (32,3) | 54 (56,3) |
| (48) - Ensures that the client and/or caregivers receive and understand the information on which they base their consent to care. | 6 (6,3) | 22 (22,9) | 68 (70,8) |
| (49) - Establishes priorities for care, whenever possible, in collaboration with clients and/or caregivers. | 3 (3,1) | 20 (20,8) | 73 (76,0) |
| (50) - Identifies expected results and the timeframe for achieving and/or reviewing them, in collaboration with clients and/or caregivers. | 7 (7,3) | 40 (41,7) | 49 (51,0) |
| (51) - Reviews and reformulates the care plan regularly, whenever possible, in collaboration with the clients and/or caregivers. | 2 (2,1) | 32 (33,3) | 62 (64,6) |
| (52) - Documents the care process. | 1 (1,0) | 12 (12,5) | 82 (85,4) |
| (53) - Implements planned nursing care to achieve expected results. | 3 (3,1) | 14 (14,6) | 79 (82,3) |
| (54) - Practises nursing in a way that respects the limits of a professional relationship with the client. | 6 (6,3) | 9 (9,4) | 81 (84,4) |
| (55) - Documents the implementation of interventions. | 2 (2,1) | 11 (11,5) | 83 (86,5) |
| (56) - Responds effectively in unexpected or rapidly changing situations. | 11 (11,5) | 41 (42,7) | 44 (45,8) |
| (57) - Responds effectively in emergency or catastrophe situations. | 29 (30,2) | 43 (44,8) | 24 (25,0) |
| (58) - Evaluates and documents progress towards the expected results. | 3 (3,1) | 16 (16,7) | 72 (75,0) |
| (59) - Collaborates with clients and/or caregivers in reviewing progress towards the expected results. | 9 (9,4) | 32 (33,3) | 55 (57,3) |
| (60) - Using assessment data to alter care planning. | 4 (4,2) | 17 (17,7) | 74 (77,1) |
Caption: Competence indicators and most relevant values in bold.
For Competence B5: "Promotes a safe environment", 78.1% of students rated PBL as having made a good/excellent contribution to the development of the criterion "Uses appropriate assessment tools to identify actual and potential risks" (Table 5).
From another perspective, regarding this competence, 27.1% of students stated that PBL did not contribute to the development of the criterion "Records and reports safety concerns to the appropriate authority", and 10.4% reported that PBL did not contribute to the development of the criterion "Ensures the safe administration of therapeutic substances."
Tabela 5 Results of the scores awarded by students for Competence B5: Promotes a safe environment (n=96)
| Competence Criteria | N (%) | ||
|---|---|---|---|
| Does not develop | Satisfactory development | Good/excellent development | |
| (68) - Creates and maintains a safe care environment using quality assurance and risk management strategies. | 5 (5,2) | 22 (22,9) | 69 (71,9) |
| (69) - Uses appropriate assessment tools to identify actual and potential risks | 6 (6,3) | 15 (15,6) | 75 (78,1) |
| (70) - Ensures the safe administration of therapeutic substances. | 10 (10,4) | 23 (24,0) | 63 (65,6) |
| (71) - Implements infection control procedures. | 9 (9,4) | 24 (25,0) | 63 (65,6) |
| (72) - Records and reports safety concerns to the competent authority. | 26 (27,1) | 25 (26,0) | 45 (46,9) |
Caption: Competence indicators and most relevant values in bold.
4. Discussion
This study analysed the contributions of PBL, from the nursing students´ perspective of to the development of competences related to care provision and management within the scope of the Registered Nurse profile, in accordance with Regulation n.º 190/2015 of Ordem dos Enfermeiros. Overall, the results were very positive, with most students acknowledging that PBL contributed in a good/excellent way to the development of competences within this domain.
These findings are consistent with those reported by Silva et al. (2019) on the implementation of PBL with nursing students in emergency and urgent care settings. The authors concluded that this strategy promoted a more active role among students, allowing them to move beyond being mere recipients of information and to become active participants in the search for relevant knowledge based on real problems and defined learning objectives, thus promoting more reflexive learning. Furthermore, the authors note that incorporating easily applicable active methodologies (such as PBL) enables students to take ownership of their learning process within a dialogical, integrative, and questioning educational framework.
In this regard, Santos et al. (2019) state that PBL enhances critical thinking, autonomy, motivation to learn, active learning attitudes, teamwork capabilities, and problem-solving skills. Similarly, Kong et al. (2014), in a systematic review with meta-analysis, concluded that PBL can help nursing students to improve their critical thinking. Similar findings were also observed in the field of trauma care by Zheng et al. (2021). Additionally, Rodrigues et al. (2024) highlight that as far as interpersonal relationships are concerned, learning in small groups (as occurs in PBL) goes far beyond a pedagogical activity or dynamic. It constitutes a genuine learning community and a democratic space for expression, listening, inclusion, and dialogue.
As far as “acts in accordance with the principles of care provision and management” (Competence B1), students emphasised that PBL contributed significantly to the application of critical thinking and problem-solving techniques, to evidence-based decision-making, and to providing justification for nursing care. In this context, Zhang and Wilkinson (2014) developed a study that aimed to evaluate the effectiveness of PBL in developing knowledge related to the care of individuals with diabetes and renal failure, and concluded that students who engage in PBL tend to consult learning resources more frequently and adopt a more intentional learning style. According to the authors, PBL reshapes students’ learning approaches and fosters patterns that promote proactive lifelong learning as students progress from “novices” to “experts”. From this perspective, the development of professional nursing competences is seen as a gradual and evolutionary process (Rudberg et al., 2022).
By the end of the first cycle of studies, students are expected to have developed an initial set of competences enabling them to provide care. However, this should only be viewed as the starting point, with continuous academic and clinical improvement required throughout their professional practice. In this regard, a solid foundation of knowledge enables students to reflect on their own roles and on nursing roles in clinical settings. Thus, PBL can promote reflection and metacognition, which are key to self-directed learning, helping students to monitor and to improve their learning processes and outcomes (Rodrigues et al., 2024).
These interactions can encourage students to reflect on their own perspectives, opinions, and arguments and enhance their meta-cognitive skills in self-assessment and self-regulation. In a study involving health sciences students who engaged in PBL within a simulation context, participants considered the experience highly valuable for their training. They strongly agreed that it supported and influenced their learning process, allowing them to acquire, to consolidate, and to deepen their knowledge (Carramate et al., 2020).
Similarly, studies developed by Amakali (2012) and Sharma et al. (2023) concluded that PBL has proven to be an effective learning strategy in nursing, offering a coherent and integrated approach that yields greater advantages over traditional teaching methods. As a “student-centred” approach, PBL enables learners to be more analytical, responsible, self-aware, and motivated toward lifelong learning.
Still in relation to Competence B1, students conversely reported that this active learning strategy did not help them to understand emergency plans for catastrophe situations. This is likely since the problem-based scenario used in the activity did not focus on this specific topic, nor did it include information that would prompt the need to research such plans.
Regarding the contribution to health promotion (Competence B2), students emphasised that PBL fosters a holistic view of the individual, family, and community. It considers the multiple determinants of health and helps them to recognise the potential of health education within nursing interventions.
In this context, Rodrigues et al. (2024) point out that PBL fosters the development of clinical reasoning, an essential tool in nurses’ decision-making processes, and contributes to a holistic understanding of the person receiving care. Similarly, Mendes et al. (2012), in their study on the contributions of PBL to student performance in clinical teaching, noted that students recognise the importance of PBL in fostering awareness of holistic care, and consequently, in promoting excellence in nursing practice. By supporting the development of reasoning, reflection, and problem-solving skills, PBL leads students to think comprehensively, from all angles, and in greater depth.
Regarding the contributions of PBL to the use of the Nursing Process (Competence B3), most participants reported that this strategy helped them improve the documentation of the implementation of interventions and the overall nursing care process. These results may be related to the methodology recommended to analyse the problem-based scenario, which requires students to develop a nursing care plan. That care plan should include the initial nursing assessment, identification of actual or potential problems through diagnostic activity, formulation of nursing diagnoses, and prescription of nursing interventions appropriate to the information provided.
According to Wosinski et al. (2018), through PBL, students enhance their critical thinking abilities and analytical judgment by evaluating data from the scenario, engaging in a progressive reasoning process, and making decisions grounded in critical thinking and evidence derived from bibliographic research. In the study developed by Lira & Lopes (2011), which aimed to evaluate the effectiveness of a PBL-based teaching strategy on nursing diagnoses, the authors concluded that this educational approach appeared to improve students’ clinical reasoning and diagnostic judgment.
Similar results were found by Sardo & Dal Sasso (2008), where a PBL practice in Basic Life Support (BLS) encouraged nursing students to take a more active role in their learning process. It also helped them build a solid knowledge base in BLS, enabling them to act in accordance with international protocols and motivating them to engage with more complex topics in the field of emergency and urgent care. Still within this competency, students once again reported that PBL did not support their ability to respond effectively in emergency or catastrophe situations.
Finally, in relation to promoting a safe environment (Competence B5), students evaluated PBL as a strategy that supports the use of appropriate assessment tools to identify actual and potential risks.
In this regard, a study by Jamshidi et al. (2021) on the influence of PBL on nursing students' knowledge, attitudes, and perceptions concerning patient safety revealed that PBL had a significant impact on all three variables compared to conventional teaching methods. Considering the positive outcomes of that study (including improvements in continuous, student-centred learning and greater focus on concept comprehension and innovation), the authors recommend that nursing educators adopt this method to enhance students’ clinical and cognitive abilities and to ensure the safety of patients under their care.
Similarly, in the study developed by Hilda et al. (2023), which aimed to develop a conceptual model of PBL specifically for Patient Safety (Problem-Based Learning Patient Safety), the authors emphasised that patient safety must be incorporated into integrated nursing curricula and addressed through diverse learning modalities, including simulations, coursework, readings, and clinical experiences. They recommend the teaching of patient safety through simulation activities for nursing students, with PBL as a resource to be integrated into these approaches.
However, students indicated that PBL did not help them develop the ability to record and report safety concerns to the appropriate authority. This finding may be considered a limitation of the study, as the problem-based scenario used did not explicitly provide an opportunity to explore this particular area of competency.
It was also observed that, despite specific guidelines being in place to guide the pedagogical process, student groups were supervised by different teachers/tutors, who may have influenced the consistency in the strategy implementation. Additionally, the group guidance and meetings were conducted remotely due to restrictions imposed by the COVID-19 pandemic, which may have limited interaction and control over some student participation variables.
Moreover, the problem scenarios used in the 2nd and 3rd years were focused on different themes (medical and surgical areas, respectively), which may have influenced the participants’ responses, as each scenario could foster the development of different competences. This variation may also have affected students’ performance, satisfaction, and competence development, since 2nd and 3rd-year students are at different stages of academic and clinical development.
Conclusion
In the students' opinion, PBL contributed most significantly to the development of skills related to the application of critical thinking and problem-solving techniques, the ability to view individuals, families, and communities from a holistic perspective, the recognition of the potential of health education, the documentation of intervention implementation, and the use of appropriate assessment tools to identify actual and potential risks.
This learning strategy fosters the development of critical thinking, problem-solving, the transfer of theoretical knowledge into practice, and the integration of knowledge from various disciplines. It is a strategy that allows the integration of knowledge from the various scientific areas present in the Nursing Degree Curriculum, facilitating the aggregation of knowledge to support clinical decision-making in nursing.
PBL also facilitates students' adaptation and integration into clinical practice contexts by promoting a holistic view of the person, rather than a compartmentalised one. In similar situations (like the COVID-19 pandemic, and/or in other comparable challenges), this strategy may prove to be a highly valuable tool for developing nursing competencies through remote, tutor-guided learning.
Moreover, it contributes to the formation of Registered Nurses who are more reflexive and better equipped to apply reflexive analysis in their future professional practice.
Acknowledgements
We would like to express our acknowledgements to the School of Health Sciences of the University of Aveiro for the support provided, and to the students who voluntarily participated in this study.
Authors' contribution
Conceptualization, J.S., A.R. and P.S.; data curation, J.S.; formal analysis, J.S., A.R. and P.S.; investigation, J.S., A.R. and P.S.; methodology, J.S., A.R. and P.S.; project administration, J.S.; resources, J.S., A.R. and P.S.; software, J.S., A.R. and P.S.; supervision, J.S.; validation, J.S., A.R. and P.S.; visualization, J.S., A.R. and P.S.; writing-original draft, J.S., A.R. and P.S.; writing-review and editing, J.S., A.R. and P.S.















