In the transition from adolescence to adulthood, university students face numerous challenges. These include adapting to a new social context, living away from home and dealing with social and academic pressure, which could increase the risk of sleep difficulties and sleep disorders (Li et al., 2018).
Poor quality of sleep is associated with negative consequences, including fatigue, difficulties in concentration, changes in mood, and cognitive impairment, having a negative impact on health, academic performance and professional success. Poor sleep is also linked to various pathologies, such as migraines, lower back pain, cardiovascular problems, cancer and psychiatric disorders (Li et al., 2018). The prevalence of insomnia varies geographically (ranging from 3% to 74.2%; Li et al., 2018) with the timeframe assessed, the method of measurement, and operational diagnostic criteria (ranging from 6% to 33%; Ohayon, 2002).
Thus, the concept of sleep difficulties differs from the DSM-5’s insomnia diagnosis (American Psychiatric Association [APA], 2013), which is defined as dissatisfaction with sleep associated with difficulty in initiating sleep, or maintaining sleep, or early-morning awakening at least 3 times a week for at least 3 months. Additionally, it is crucial to evaluate other parameters, such as sleep opportunity, and clinically significant impairment in important areas of functioning, the comorbidity with other medical and psychiatric disorders, and drug abuse, among others. The dissatisfaction with sleep is generally associated with difficulties in initiating sleep (DIS), maintaining sleep (DMS) and early morning awakening (EMA) which could contribute to the curtailment of the total amount of sleep (sleep quantity), non-restorative sleep (NRS), and poor sleep quality (poor vs. good sleep quality; American Psychiatric Association APA, 2013; Li et al., 2018; Ohayon et al., 2010; Ohayon & Paiva, 2005). The prevalence of sleep disturbances is higher than that of insomnia. In the general population, the prevalence of complaints related to DIS, DMS, EMA or NRS, evaluated with yes/no answer questions, ranges from 1.6% to 76.3%. Among university students worldwide, the prevalence of sleep disturbances ranges from 3.0% to 74.2% (Li et al., 2018).
Predisposition (e.g., personality traits/dispositions), precipitating factors (e.g., stressful life events), and maintenance factors (e.g., emotion regulation strategies) have, therefore, been implicated in generation and perpetuation of insomnia and sleep difficulties (Harvey, 2002; Perlis et al., 2017).
Optimism and pessimism are considered as two personality dispositions that reflect, respectively, a positive/negative expectation towards the future and the achievement of favourable/unfavourable outcomes in life (Lau et al., 2015). One key aspect distinguishing optimists from pessimists is the way they face adversity and solve problems, which may also have consequences for sleep quantity and quality (Lau et al., 2015).
Emotion regulation is defined as the intrinsic and extrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions, as well as influencing their intensity and duration (Thompson, 1994). Emotion is regulated via three main mechanisms: physiologically (tachycardia/palpitations, tachypnea/increased respiratory rate and sudoresis/sweating), through unconscious cognitive processes (selective attention processes, memory distortions, denial, or projection), and through conscious processes to cope with stressful life events, such as cognitive emotion regulation (CER; Garnefski et al., 2001, 2002). These CER could be either adaptive (or positive) and non-adaptive (or negative), considering the strategies used to deal with emotions triggered by stressful events and the positive or negative outcomes. Thus, adopting non-adaptive CER (such as rumination, self-blame, suppression), in comparison to adaptive strategies (such as reappraisal, refocusing and problem solving), is strongly associated with PD/psychopathology, such as depression, anxiety, negative affect, sleep difficulties and insomnia (Aldao & Nolen-Hoeksema, 2010; Amaral et al., 2018, 2021).
Optimism has been associated with physical/psychological well-being, along with adaptive coping strategies, such as proactively facing stressful events to overcome them (e.g., problem-focused coping and approach coping strategies; Uchino et al., 2017), as well as with CER processes, including positive reappraisal, positive refocusing, and putting into perspective (Subramanian & Nithyanandan., 2007). It has also been linked to better sleep quality and sleep sufficiency (Lau et al., 2015). Optimism has shown negative associations with anxiety, depression, negative affect, insomnia, and poor sleep quality, short (<6 h) and long (>9 h) sleep duration, and stress (Lau et al., 2015, 2017; Uchino et al., 2017; Weitzer et al., 2020). Additionally, it has been associated with less adaptive CER strategies, such as self-blame, catastrophizing, and rumination (Subramanian & Nithyanandan, 2007).
Regarding sleep, an optimistic perspective might reduce worries and rumination and improve sleep directly, through adaptive sleep habits; and indirectly, through adaptive problem-solving strategies (Lau et al., 2015), and low levels of psychological distress (Lau et al., 2015, 2017; Uchino et al., 2017). In contrast, pessimism is directly associated with negative affect, PD, and less adaptive coping strategies, such as self-blame, avoidance, and withdrawal (Carver et al., 2010). High levels of pessimism and low levels of optimism are associated with increased risk of depression, suicidal behaviours, and postpartum depressive symptoms (Lau et al., 2015). In addition to depressive mood, studies have shown that too little optimism and too much pessimism are associated with more anxiety and stress, which could negatively impact sleep (Harvey, 2002; Lau et al., 2017).
It is, therefore, possible that there is a potential effect of optimism/pessimism on susceptibility to sleep difficulties, and that this might also be indirectly through CER strategies and PD mediation. In fact, the rationale for the mediation analysis is that if one or more variables has been associated with both the independent variable (X; in this case optimism/ pessimism), and the dependent variable (Y; in this case sleep difficulties), it is plausible that they are strong candidates to mediate their association.
Insomnia and PD (depression, anxiety, and stress) are described as comorbidities, linked by several underlining mechanisms, including biological factors, dispositional traits like optimism and pessimism, and CER strategies (Lau et al., 2017; Staner, 2010).
The mediation role of PD has already been explored by, for example, Lau et al. (2015), who have observed that depressive mood mediates the bidirectional relationship between optimism and sleep difficulties as follows: Optimism prospectively and indirectly reduces sleep difficulties through its positive effects in reducing depressed mood. On the other hand, sleep difficulties are associated with low optimism, both directly and indirectly, through its impact on an increase in depressed mood. Moreover, the depressed mood might partially explain how sleep difficulties prospectively cause pessimism.
As for the role of CER strategies in relation to both optimism/pessimism (Carver et al., 2010; Subramanian & Nithyanandan, 2007; Uchino et al., 2017) and sleep difficulties/insomnia (Amaral et al., 2018, 2021; Lau et al., 2015, 2017; Uchino et al., 2017; Weitzer et al., 2020), they might, therefore, mediate the relationship between these variables. As far as we know, however, this is yet to be explored by any study.
Studying the factors contributing to the genesis and maintenance of sleep difficulties might have consequences for the promotion of university students’ academic performance, adjustment to academic life, physical and mental health, and quality of life. Here, this study aimed to analyse: (1) The extent to which optimism/pessimism, CER strategies, and PD were associated with sleep difficulties; (2) the role of negative CER strategies and PD as mediators in the relationship between pessimism and sleep difficulties, controlling for the effect of positive CER strategies; and (3) the role of positive CER strategies and PD as mediators of the relationship between optimism and sleep difficulties, controlling for the effect of negative CER strategies.
One of our study hypotheses (related to the first aim) was that pessimism (Lau et al., 2015, 2017), non-adaptive CER strategies, and PD (Amaral et al., 2018, 2021; Lau et al., 2015, 2017) are positively associated with sleep difficulties, whereas optimism (Lau et al., 2015, 2017; Uchino, et al., 2017), and adaptive CER (Amaral et al., 2021) are inversely associated with sleep difficulties.
Given that prior studies’ results also indicated that adaptive coping and CER strategies and low levels of PD are related to optimism (e.g., Carver et al., 2010; Lau et al., 2015, 2017; Subramanian & Nithyanandan., 2007; Uchino et al., 2017; Weitzer et al., 2020), as well as better sleep, less sleep difficulties and less insomnia symptoms (e.g., Amaral et al., 2021; Lau et al., 2015, 2017; Weitzer et al., 2020), it might be possible that these variables mediate the relationship between optimism and sleep difficulties. Therefore, another study hypothesis (related to the second aim) posits that optimism is associated with fewer sleep difficulties, and that adaptive CER strategies and low levels of PD mediates this relationship, while controlling for the effect of non-adaptive CER strategies.
In turn, there is also evidence from the literature that non-adaptive coping and CER strategies, as well as high levels of PD are associated with both pessimism/low optimism (Carver et al., 2010; Lau et al., 2015, 2017; Weitzer et al., 2020), and more sleep difficulties/insomnia symptoms (Amaral et al., 2018, 2021; Lau et al., 2015, 2017; Weitzer et al., 2020). It is thus conceivable that these variables might mediate the relationship between pessimism and sleep difficulties. We therefore also hypothesized (related to the third aim) that pessimism is associated with more sleep difficulties, and non-adaptive CER strategies and high PD mediates this relationship, controlling for the effect of adaptive CER strategies.
Considering the role of the covariates in these mediation models, it is also predictable that adaptive or non-adaptive CER strategies might influence the variability of both PD and sleep difficulties, exerting an effect on decreasing/increasing their levels (e.g., Aldao & Nolen-Hoeksema, 2010; Amaral et al., 2018, 2021; Lau et al., 2015, 2017; Uchino et al., 2017; Weitzer et al., 2020).
Method
Participants and procedure
The present cross-sectional study was approved by the Ethics Committee of the Faculty of Medicine of the University of Coimbra (Ref. 098-CE-2014). The participants were from the Medicine and Dentistry courses at the University of Coimbra and from several Health Technology courses at the Polytechnic Institute of Coimbra. The participants were invited by their teachers or investigators to join the study. The assessment was conducted in person, during classes and took place from 10th December 2014 to 15th June 2015. Informed consent was obtained from participants prior to their participation in the study.
The non-probabilistic convenience sample consisted of 253 higher education students (77.9% females), mean aged 20.53 years (SD = 1.64; range: 18-25 years), predominantly of Portuguese nationality (95.7%) or of dual nationality. They attended between the 1st and the 4th year (with 22.6% in the 1st year; 69.9% in the 3rd / 4th year) and were mostly from medicine / dentistry courses (87%).
Instruments
The participants completed a booklet of questionnaires with sociodemographic questions and a set of questionnaires, validated for the Portuguese population, which included:
The Depression, Anxiety, and Stress Scale-21, DASS-21 (Lovibond & Lovibond, 1995, Pais-Ribeiro et al., 2004) that assessed Anxiety (A), Depression (D) and Stress (S) dimensions, and global PD (DASS-T; total score). It consisted of 21 items, with 5 Likert-type answer options, rated from 0 (Nothing applied to me) to 4 (It applied to me most of the time). The dimensions of the scale had good internal consistency (Almeida & Freire, 2017; Soares & Santos, 2021) in the Portuguese population (Cronbach's alpha (α): D = .85; A = .74; S = .81; Pais-Ribeiro et al., 2004). In the sample of the present study, the internal consistency of the scale was high (α DASS-T = 0.96).
The Optimism-Pessimism-2 Scale (OP-2 Scale). Pessimism and optimism were assessed with 2 items (Kemper et al., 2011), which are rated from 1 (Not at all optimistic/ pessimistic) to 7 (Very optimistic/pessimistic). The OP-2 Scale revealed good psychometric characteristics in German, Spanish and Italian samples (Kemper et al., 2017). Silva et al. (2014) observed that both items have concurrent validity with the optimism and pessimism dimensions of the Life Orientation Test - Revised (LOT-R; Scheier et al., 1994; Laranjeira, 2008). The correlations between their scores were of large/medium magnitude (Cohen, 1988; Pallant, 2010): r, LOT-R optimism/ OP-2 optimism = .602, r, LOR-R pessimism/OP-2 pessimism = .444, both p < .01) in a sample of Portuguese community participants, including university students. Both OP-2 items also revealed divergent validity with LOT-R, neuroticism and extroversion dimensions of the Eysenck Personality Inventory EPI-12, with correlation coefficients of large/medium magnitude (Cohen, 1988; Pallant, 2010). The correlation of OP-2 optimism with LOT-R pessimism and the neuroticism dimension of the Eysenck Personality Inventory (EPI-12) were of -.492 and -.539, respectively, and the correlation of OP-2 pessimism with LOT-R optimism and EPI-12 extroversion were of -.573 and -.371 (all p<.01; Silva et al., 2014).
The Cognitive Emotion Regulation Questionnaire (CERQ; Garnefski et al., 2001) consists of 36 items, which assessed nine strategies of CER used in response to stressful or threatening events. The CERQ items were answered on a five-point Likert scale, ranging from 1 (Never) to 5 (Always). Higher scores indicated higher levels of the respective dimension. The version validated for the Portuguese population (Castro et al., 2013) had a structure of eight factors, with good/respectable/very good internal consistency, four of which were considered adaptive and four non-adaptive. The adaptive CER strategies (CERQ-positive; CERQ-P) were: Putting into perspective (thoughts about the gravity of the event, emphasizing its relativity and comparing it with other events; α = .80); positive refocusing (pleasant thoughts instead of thinking about the current event; α = .85); positive reappraisal and refocus on planning (thoughts of creating a positive meaning for what happened, in terms of personal growth and thoughts about what can be done to control the negative event; α = .89); and acceptance (acceptance of what has been experienced, conformity with what happened; α = .70; Castro et al., 2013).
The non-adaptive CER strategies (CERQ-negative; CERQ-N) were self-blame (thoughts of self-blame for the lived experience; α = .76); blaming-others (placing blame for the experience lived on the environment or on another person; α = .79); rumination (thoughts about the feelings / cognitions associated with the negative event; α = .78); and catastrophizing (thoughts that emphasize the terror experienced; α = .74; Castro et al., 2013).
The scores for each of the CERQ dimensions resulted from the sum of the respective item scores. The variables CERQ-P and CERQ-N resulted from the sum of the item scores of the adaptive and non-adaptive CERQ dimensions, respectively.
Sleep difficulties during the last month, namely DIS, DMS and EMA were assessed with three questions, rated 1-5 (1, Never; 2, Rarely; 3, Sometimes; 4, 3 to 4 nights a week; 5, Almost every night; Azevedo & Bos, 2005). The sleep difficulties index (SDI) resulted from the sum of the scores of these three items and presented adequate internal consistency in the present study sample (α = .71).
Statistical Analysis
For data analysis, we used SPSS program (v. 23) and the PROCESS Macro for SPSS (v. 2.5; Hayes, 2013). We performed the descriptive statistics analysis. The normality of the distribution of continuous variables was explored, based on their skewness and kurtosis values. When the distribution of continuous variables was close to normality, we applied inferential parametric tests, otherwise we used non-parametric ones.
We applied Pearson's product-moment and Spearman's rho correlation coefficients to explore the association between variables and sleep difficulties and optimism/pessimism. Biserial correlations were applied to analyse the associations between gender and other variables. Cohen's (1988) criteria were used to analyse their magnitude: Small, r = .10 to .29; medium, r = .30 to .49; large, r = .50 to 1.0 (Pallant, 2010).
To analyse whether and how CER strategies (mediator 1, M1) and PD (mediator 2, M2) mediate, respectively, the relationship between pessimism and optimism (X) and sleep difficulties (Y), serial multiple mediators mediation analysis (model 6) was computed. When the variable X was pessimism, M1 was considered negative CER strategies, M2 was DASS-T and the covariate was positive CER (Figure 1, Model 1). When the variable X was optimism, M1 was considered positive CER strategies, M2 is DASS-T and the controlled covariate was negative CER (Figure 1, Model 2). The confidence intervals (CIs) of the bootstrap analysis for the indirect effects were calculated repeatedly in 1000 bootstrap samples, estimating the model in each of these samples, calculating the indirect effects and deriving the final CIs. The confidence level for all CIs was 95%. An indirect effect was different from zero with a 95% CI, if the zero value was not included in the CI. If the 95% CI contained this value, the indirect effect was not statistically different from zero.
Results
Prevalence of sleep difficulties
Regarding the prevalence of self-reported sleep difficulties, students who described DIS, DMS and EMA frequently (3 or 4 nights a week/Almost every night) were 10.2%, 9.0%, and 6%, respectively. Those who described occasionally having DIS, DMS and EMA, were 31.2%, 25.5% and 24.5%, respectively. The students who scored a standard deviation or more above the average in the SDI were 10.3%.
Correlations
Gender and age were not significantly associated with sleep difficulties, but pessimism correlated negatively with age (Table 1).
Optimism was inversely correlated, and pessimism was positively correlated at a small to medium level with PD (depression, anxiety, stress, DASS-T) and negative CER strategies. Additionally, optimism was positively correlated, and pessimism was negatively correlated at a small to medium level with positive CER strategies (Table 1).
Optimism, inversely, and pessimism, along with PD (stress, anxiety, depression, and overall distress), negative CER strategies, and its rumination dimension, in a positive way, were significantly associated with various sleep difficulties, ranging from small to medium in magnitude. The most robust associations, although with a medium magnitude, were found between SDI, DIS, and the total score of DASS-21 (Table 1).
Self-blame also showed a positive and significant small correlation with DIS and SDI, and catastrophizing was correlated with SDI. The positive CER strategies were significantly, and negatively associated at a small level with SDI. Its dimension, positive reappraisal and refocus on planning revealed a significant negative association with SDI, DIS and DMS and a trend towards significant association with the EMA (p = .055; Table 1).
Table 1 Correlation coefficients and central tendency values of the variables.
| Optim r | Pess r | SDI r | DIS r | DMS r | EMA r | M (SD); Range | |
|---|---|---|---|---|---|---|---|
| Gender | -.116 | .100 | .112 | .096 | .061 | .101 | --- |
| Age (years) | .094 | -.137* | .023 | -.057 | .117 | .041 | 20.53 (1.64); 18-25 |
| CERQ1 | .397** | -.375** | -.193** | -.126* | -.153* | -.121 | 14.25 (3.26); 4-20 |
| CERQ2 | .377** | -.346** | -.102 | -.116 | -.052 | -.079 | 8,24 (2.96); 3-15 |
| CERQ3 | -.291** | .343** | .250** | .215** | .174** | .208** | 5.64 (1.94); 2-10 |
| CERQ4 | -.140* | .147* | .001 | -.020 | .017 | .019 | 5.45 (1.94); 3-15 |
| CERQ5 | .182** | -.144* | -.054 | -.029 | -.084 | -.052 | 6.91 (2.04); 2-10 |
| CERQ6 | -.289** | .308** | .172** | .255** | .074 | .077 | 6.45 (2.39); 3-15 |
| CERQ7 | .195** | -.151* | -.050 | -.022 | -.048 | -.005 | 9.36 (2.70); 3-15 |
| CERQ8 | -.313** | .397** | .129* | .083 | .121 | .127 | 3.54 (1.64); 2-10 |
| CERQ-N | -.380** | .439** | .198** | .218** | .129* | .146* | 38.75 (8.57); 12-60 |
| CERQ-P | .385** | -.344** | -.136* | -.102 | -.111 | -.087 | 21.08 (5.72); 10-40 |
| DASS-D | -.406** | .402** | .346** | .350** | .223** | .209** | 3.32 (4.02); 0-20 |
| DASS-A | -.286** | .324** | .233** | .238** | .128* | .139* | 3.10 (3.66); 0-18 |
| DASS-S | -.351** | .387** | .315** | .398** | .220** | .219** | 6.08 (4.67); 0-21 |
| DASS-T | -.384** | .416** | .325** | .354** | .190** | .180** | 12.51 (11.43); 0-52 |
| Otim | -- | -.816** | -.204** | -.171** | -.162** | -.164** | 4.66 (1.25); 1-7 |
| Pess | -- | -- | .225** | .166** | .178** | .200** | 3.40 (1.42); 1-7 |
| M ± SD Range | -- | -- | 6.72±2.34 3-15 | 2.34±1.03 1-5 | 2.30±.98 1-5 | 2.00±.94 1-5 |
Note: *p < .05; **p < .01; Correlation coefficients values in bold indicated statistically significant correlations; Optim.: Optimism; Pess.: Pessimism; CERQ1: Positive Reappraisal and Refocus on Planning; CERQ2: Positive Refocusing; CERQ3: Rumination; CERQ4: Blaming others; CERQ5: Putting into perspective; CERQ6: Self-blame; CERQ7: Acceptance; CERQ8: Catastrophizing; CERQ-P/N: CERQ positive/negative; DASS-D/A/S: (Depression, Anxiety. Stress); r = Correlation Coefficients
Serial multiple mediator mediation analysis
Link between pessimism and sleep difficulties. The serial multiple mediator mediation analysis was performed to explore the relationship between pessimism (X) and sleep difficulties (Y). CERQ-N (M1) and DASS-T (M2) were considered mediators and positive reappraisal, and refocus on planning (CERQ1) as the covariable (cov.), which was the only dimension of CERQ-P that showed a significant relationship/trend towards significance with sleep difficulties. The regression coefficients, model statistics and direct, indirect and total effects of pessimism in SDI, DIS, DMS and EMA were described in Table 2 and 3. Considering the direct effects of the variables on mediators, which were common to all models linking pessimism to sleep difficulties, it should be noted that the variables explained about 20% of the variance of CERQ-N (M1), but only pessimism had a significant association with it (a1; Table 2). In turn, PD (DASS-T, M2) had an explained variance of 32.27% and pessimism (a2), CERQ-N (d21) and CERQ1 (cov.) significantly contributed to it (Table 2). Regarding the direct effects of the variables on the independent variables (Y), they explained 15.01%, 15.62%, 6.96% and 7.78% of the variability of the SDI, DIS, DMS and EMA, respectively and, in all models, DASS-T (b2) was the only significant predictor of these sleep difficulties. The remaining variables did not have a significant direct effect on sleep difficulties, including pessimism (c') and negative CER (b1 and cov.; Table 2). The total effect (c) was statistically significant in all mediation models, with the total indirect effect (c-c') being significant only for the models on which SDI and DIS were dependent variables (Y; Table 3). However, there were two indirect processes underlying the relationship of pessimism to SDI, DIS, DMS and EMA, which were statistically significant. In one, pessimism had an impact on increasing CERQ-N, which increased DASS-T, which, in turn, had an impact on increasing SDI, DIS, DMS and EMA (Pessimism→CERQ-N→DASS-T→ SDI/DIS/DMS/EMA). In the other, pessimism had an effect on DASS-T increasing, which, in turn, increased sleep difficulties (Pessimism→DASS-T→SDI/DIS/DMS/EMA). The covariate positive reappraisal and refocus on planning (CERQ1) had a significant negative effect on DASS-T (cov.; Tables 2-3). Figure 1 (Model 1) represented the serial mediation model of the relationship between pessimism and sleep difficulties (SDI, DIS, DMS and EMA), indicating the two significant indirect processes that linked these variables.
Link between optimism and sleep difficulties. Next, the serial mediation analysis was performed to explore the relationship between optimism (X) and sleep difficulties (Y), considering positive reappraisal and refocus on planning (CERQ1; M1) and DASS-T (M2) as mediators (M) and CERQ-N as covariable (cov.). The regression coefficients, standard errors, model statistics and direct, indirect and total effects of optimism on SDI, DIS, DMS, EMA were described in Tables 2 and 3. Considering the direct effects of the variables on the mediators, which were common aspects to all models linking optimism to sleep difficulties, it should be noted that the variables explained 16.28% of the variance of CERQ1 (M1), which is significantly and positively determined by optimism (a1). In turn, the explained variance of PD (DASS-T; M2) corresponded to 32.65%. This variable was significantly and negatively determined by optimism (a2) and CERQ1 (d21) and, positively, by CERQ-N (cov.; Table 2). The direct effects of the independent variables (I.V.) in each type of sleep difficulty explained about 14.79%, 15.62%, 6.75% and 7.17% of the variability of the SDI, DIS, DMS and EMA, respectively and in all models the DASS-T (b2) was the only significant predictor of these sleep difficulties. None of the other variables had a significant direct effect on sleep difficulties, including optimism (c '; Table 2). The total effect (c) was only significant when the SDI was the dependent variable (Y), but the total indirect effect (c-c') was statistically significant in all models. There were two indirect statistically significant processes, underlying the relationship of optimism with SDI, DIS, DMS and EMA. In one, optimism had an impact on increasing CERQ1, which, in turn, decreased DASS-T, which then had an impact on increasing SDI, DIS, DMS and EMA (Optimism→CERQ1→DASS-T→SDI/DIS/DMS/EMA). In the other process, optimism had an effect in decreasing DASS, which, however, caused an increase in sleep difficulties (Optimism→DASS-T→SDI/DIS/DMS/EMA). The CERQ-N covariate had a significant effect only in the increase of DASS-T (cov.; Table 3 and Figure 1, Model 2).
Table 2 Serial multiple mediators mediation models that linked pessimism (X1) or optimism (X2) to sleep difficulties (DIS. DMS. EMA and SDI), with the mediator 1 CERQ-N/ CERQ-1 and the mediator 2 DASS-T - Regression coefficients and model statistics.
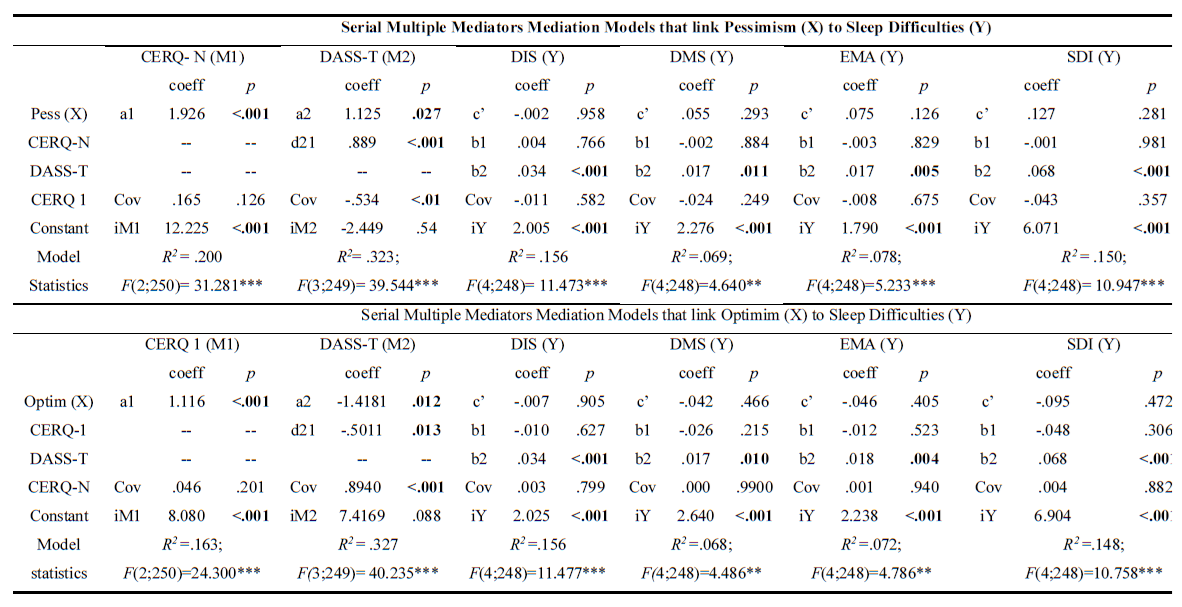
Note: ***p < .001; **p < .01; *p < .05; DIS: Difficulty initiating sleep; DMS Difficulty maintaining sleep; EMA: Early morning awakening; SDI: Sleep difficulties index; Optim: Optimism; CERQ: Cognitive Emotion Regulation Questionnaire; CERQ-N: CERQ negative dimension; CERQ 1: Positive Reappraisal and Refocus on Planning; M1: Mediator 1; M2: Mediator 2; Cov: Covariate
Table 3 Total, direct, and indirect effects of pessimism/optimism on sleep difficulties.
| Pessimism association with Difficulties in Initiating Sleep | |||
|---|---|---|---|
| Total effect of X on Y | c = .0999; t = 2.0557 p = .0408; CI 95% = .0042 to .1956 | ||
| Direct effect of X on Y | c’= -.0027; t = -.0532; p = .9577; CI 95% = -.1037 to .0983 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | .1026 | .0435 | .1754 |
| X→M1→M2 →Y | .0574 | .0314 | .0987 |
| X→M2 →Y | .0379 | .0023 | .0872 |
| Pessimism association with Difficulties in Maintaining Sleep | |||
| Total effect of X on Y | c = .0977; t = 2.1001 p = .0367; CI 95% = .0061 to .1892 | ||
| Direct effect of X on Y | c’ = .0545; t = 1.0542; p = .2928; CI 95% = -.0473 to .1564 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | .0431 | .0087 | .1069 |
| X→M1→M2 →Y | .0282 | .0048 | .0627 |
| X→M2 →Y | 0186 | .0011 | .0567 |
| Pessimism association with Early Morning Awakening | |||
| Total effect of X on Y | c = .1192; t = 2.6997 p = .0074; CI 95% = .0322 to .2062 | ||
| Direct effect of X on Y | c’ = .0752; t = 1.5358; p = .1259; CI 95% = -.0212 to.1716 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | .0440 | -.0380 | .0977 |
| X→M1→M2 →Y | 0296 | .0065 | .0628 |
| X→M2 →Y | .0196 | 0015 | .0530 |
| Pessimism association with Sleep Difficulties Index | |||
| Total effect of X on Y | c = .3168; t = 2.8934; p = .0041; CI 95% = .1012 to .5324 | ||
| Direct effect of X on Y | c’= .1270; t = 1.0799; p = .2812; CI 95% = -.1046 to .3586 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | .1898 | .0429 | .3379 |
| X→M1→M2 →Y | .1152 | .0477 | .2045 |
| X→M2 →Y | .0760 | .0066 | .1897 |
| Optimism association with Difficulties in Initiating Sleep | |||
| Total effect of X on Y | c = -.0841; t = -1.5379; p = .1253; CI 95% = -.1917 to .0236 | ||
| Direct effect of X on Y | c’ = -.0068; t = -.1195; p = .9050; CI 95% = -.1196 to .1059 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | -.0772 | -.1561 | -.0241 |
| X→M1→M2 →Y | -.0187 | -.0457 | -.0038 |
| X→M2 →Y | -.0475 | -.1061 | -.0083 |
| Optimism association with Difficulties in Maintaining Sleep | |||
| Total effect of X on Y | c = -.1038; t = -1.9514; p = .0521; CI 95% = -.2086 to .0010 | ||
| Direct effect of X on Y | c’ = -.0422; t = -.7307; p = .4656; CI 95% = -.1561 to .0716 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | -.0616 | -.1225 | -.0123 |
| X→M1→M2 →Y | -.0094 | -.0316 | -.0013 |
| X→M2 →Y | -.0237 | -.0658 | -.0028 |
| Optimism association with Early Morning Awakening | |||
| Total effect of X on Y | c = -.0949; t = -1.8798; p = .0613; CI 95% = -.1944 to .0045 | ||
| Direct effect of X on Y | c’ = -.0457; t = -.8332; p = .4055; CI 95% = -.1537 to .0623 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | -.0492 | -.1091 | -.0010 |
| X→M1→M2 →Y | -.0100 | -.0283 | -.0011 |
| X→M2 →Y | -.0254 | -.0710 | -.0026 |
| Optimism association with Sleep Difficulties Index | |||
| Total effect of X on Y | c = -.2828; t = -2.2715; p = .0240; CI 95% = -.5280 a -.0376 | ||
| Direct effect of X on Y | c’= -.0948; t = -.7210; p = .4716; CI 95% = -.3537 a .1641 | ||
| Indirect effects of X on Y | Effect | 95% CI Lower | 95% CI Upper |
| Total ( c-c’) | -.1880 | -.3553 | -.0618 |
| X→M1→M2 →Y | -.0381 | -.0958 | -.0097 |
| X→M2 →Y | -.0966 | -.2292 | -.0228 |
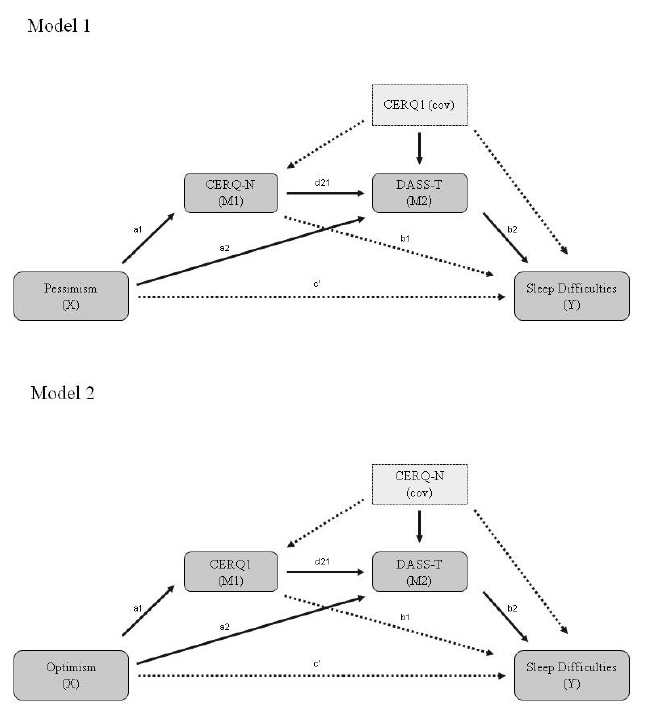
Figure 1 Diagrams of the data of Tables 2 and 3, on the serial multiple mediator model of the association between pessimism (model 1) / optimism (model 2) and sleep difficulties. Note: M1, Mediator 1; M2, Mediator 2; cov, Covariate; CERQ, Cognitive Emotion Regulation Questionnaire; DASS, CERQ-N, Negative Cognitive Emotion Regulation Strategies; CERQ1- Positive Reappraisal and Refocus on Planning; DASS-T Depression, Anxiety and Stress Scale - total score; solid bold arrows, statistically significant links; dotted arrows, statistically non-significant.
Discussion
The main aim of the present study is to explore the relationship between the optimism/pessimism traits and sleep difficulties, in terms of the role of CER strategies and PD.
Insomnia and sleep difficulties are ubiquitous in our society, and their deleterious effects on mental and physical health are well recognized and documented (Li et al., 2018). The prevalence of sleep difficulties found in the present study are in the range reported in the university student population (Li et al., 2018) and slightly overlap those observed in other studies carried out with samples of Portuguese university students. Difficulties in initiating sleep (DIS), maintaining sleep (DMS) and undesired early morning awakening (EMA; 3 or 4 nights a week/Almost every night), in the present study sample, are 10.2%, 9.0%, 6%, respectively and 10.3% of students score one standard deviation or more above the average in the SDI. The prevalence (mean of the three assessments) of difficulties in initiating sleep and in maintaining sleep Often, Very often and/or Always in two studies with Portuguese university students were 18.03%; 5.8% (Azevedo et al., 2010) and 17.93%; 5.8% (Bos et al., 2013), respectively. Considering these sleep difficulties together, the prevalence of difficulties in initiating and/or maintaining sleep were 23.8% (Azevedo et al., 2010) and 19.5% (Bos et al., 2013), respectively. The slight differences in DIS and DMS rates may be due to differences in the criteria used for their assessment, which were their presence on 3 or 4 nights a week/Almost every night and their presence Often, Very often and/or Always.
Our study shows that gender and age are not associated with sleep difficulties, confirming the results of a meta-analysis on sleep patterns in Chinese university students (Li et al., 2018) and the findings of a systematic review (Jiang et al., 2015). However, other studies indicate female gender and older age were related to insomnia and sleep difficulties (Amaral et al., 2021; Zhang & Wing, 2006). The fact that age is not related to sleep difficulties may be due to the homogeneity of this variable in the present sample of young adults, aged between 18-25 years.
In the present study, sleep difficulties are associated with PD (depression, anxiety, stress, global distress), with low levels of positive CER strategies (positive reappraisal and refocus on planning) and high levels of negative CER strategies, particularly rumination, but also self-blame and catastrophizing. These findings are in accordance with that already present in the literature (Aldao & Nolen-Hoeksema, 2010; Amaral et al., 2018, 2021). The correlation analysis also shows that optimism is associated with fewer sleep difficulties, as well as with less PD, lower levels of negative CER strategies and higher levels of positive CER strategies. Conversely, pessimism is associated with more sleep difficulties, with higher PD and higher levels of negative CER strategies and lower levels of positive CER strategies.
Our results show that optimists sleep better than pessimists, which is in line with findings from previous studies (Lau et al., 2015). The association between optimism, pessimism and low/high levels of sleep difficulties (Lau, et al., 2015; Uchino, et al., 2017), low/high levels of PD (Lau et al., 2017; Weitzer et al., 2020), and adaptive/non-adaptive CER strategies (Carver et al., 2010; Subramanian & Nithyanandan., 2007; Uchino et al., 2017) confirms the findings of previous studies. Coping strategies were another factor that influences the relationship between optimism and sleep, with adaptive coping having an effect in reducing sleep difficulties (Lau et al., 2015).
One of the strengths of our study is that it contributes to the literature by exploring the role played not only by optimism but also by pessimism in the relationship with sleep difficulties, using a mediation model with multiple mediators rather than a single one. To our knowledge, no study to date has analyzed the mediation role of both adaptive and non-adaptive CER strategies and PP in the relationship between optimism and pessimism and sleep difficulties.
A major contribution of our study to the knowledge in the field of sleep is, therefore, that its findings clarify how both the CER strategies and PD (factors that can contribute to the onset and maintenance of sleep difficulties) mediate the relationship between previous vulnerability factors - optimism/pessimism - and sleep difficulties. Although the simple correlations indicate an association between optimism/pessimism and sleep difficulties, through mediation analysis, we find that this relationship is not direct, with CER strategies and PD playing an important role in the occurrence of this connection.
For each of the traits (optimism and pessimism), there are two indirect statistically significant processes underlying their relationship with sleep difficulties (SDI, DIS, DMS and EMA). PD is a central mediator here, because it is included in all the pathways. These two processes reveal that pessimism / optimism are linked to sleep difficulties as they have an impact, respectively, on PD generation/reduction, which, in turn, determines the increase/decrease of sleep difficulties. Additionally, CER strategies have an important indirect impact on sleep difficulties. In the third process, pessimism determines an increase in the use of negative CER strategies (CERQ-N), which, in turn, has an impact on PD (DASS-T) increase, leading to sleep difficulties. On the other hand, in a fourth process, optimism determines an increase in the use of positive reappraisal and refocusing on planning (CERQ1), and this has an impact on PD (DASS-T) reduction, which, nevertheless, increases sleep difficulties. Thus, the results of the mediation analysis suggest that pessimistic people may have more sleep difficulties, either because they are more vulnerable to PD or because they use negative CER strategies, which also have an impact on the increase of PD. In contrast, optimists preferentially use positive CER (positive reappraisal and refocus on planning) and are less vulnerable to PD, which determines sleep difficulties. Despite this, optimists may also experience sleep difficulties when they present PD.
The role of psychological distress in the indirect association between optimism and sleep difficulties confirms the findings of other studies, revealing that depressive mood (Lau et al., 2015, Uchino et al., 2017), stress, and anxiety (Lau et al., 2017) are important mediation factors in the relationship between optimism and sleep quality. Such an association between optimism/pessimism and sleep difficulties does not exclude the possibility that the inverse relationship may also occur. The bidirectional relationship between optimism and sleep difficulties has also been reported (Lau et al., 2015, 2017). Indeed, studies in this area suggested that poor sleep leads to pessimism and low optimism, and that depressive symptoms play an important mediation role in their association (Lau et al., 2015, 2017).
The relationship between PD and sleep difficulties, confirmed by the present study’s results, has great clinical repercussions. Clinical studies have shown that three-quarters of patients with depression have insomnia and sleep difficulties (Staner, 2010) and that insomnia patients are twice as likely to develop depression (Baglioni et al., 2010). In addition, high levels of anxiety and stress are predictors of sleep difficulties (Lau et al., 2017). As the use of positive and negative coping strategies are differently related to PD, but are interrelated and coexist (Aldao & Nolen-Hoeksema, 2010), one of our study’s strengths is that it controlled the effect of both positive and negative CER strategies in the same serial mediation model. In pessimists, the use of positive CER strategies (positive reappraisal and refocus on planning) can have a protective effect against PD, a variable with an impact on the increase of sleep difficulties. Nevertheless, negative CER strategies are an important covariate to be aware of, as they can increase the risk of optimists having PD, which plays a central role in determining sleep difficulties in individuals with this trait. These results may have clinical implications for the therapeutic approach to sleep difficulties, which should also target CER strategies.
The present study’s findings align with both the vulnerability-stress model of the development of psychopathology/insomnia and the insomnia cognitive model (Perlis et al., 2017; Harvey, 2002). Pessimists, when confronted with stressful situations, may be more vulnerable to developing PD, sleep difficulties and insomnia than optimists (Carver, et al., 2010; Lau, et al., 2017; Scheier & Carver, 1992). They often rely on maladaptive cognitive styles (e.g., negative expectations about the future, about the attainability of achievements and desired goals, and a propensity for negative repetitive thoughts, to worrying and rumination) and maladaptive coping strategies, such as avoidance, withdrawal, self-blame (Carver, et al., 2010; Lau, et al., 2015), blaming others, rumination, and catastrophizing. Pessimists negatively toned cognitive activity and the use of maladaptive coping strategies to solve problems and regulate emotions may perpetuate stress, as well as generate, intensify and maintain stress-related psychophysiological hyperarousal and PD, increasing the risk of the onset of sleep difficulties/insomnia or its maintenance or chronicity.
A limitation of the present study is its cross-sectional design, as only longitudinal studies allow determining causal relationships and risk factors. Future longitudinal studies would be important, using stricter definitions of sleep difficulties and insomnia in healthy and psychiatric disorder populations, together with objective sleep measures.
Another additional limitation is the fact that it does not control the occurrence of psychiatric disorders and the use of psychotropic drugs by the sample students. Depression, as previously described, can change sleep habits as well as influence/bias the answers of self-report questionnaires about the dispositional traits of optimism/pessimism and sleep. The use of anxiolytics/hypnotics, antidepressants and antipsychotics, among others, can mask sleep difficulties, biasing the results (Staner, 2005). Greater knowledge in this area may help find preventive and therapeutic procedures to deal with personality characteristics and associated CER strategies, contributing to better sleep habits and the resulting well-being and health benefits.
In conclusion, pessimism is a vulnerability factor for sleep difficulties due to the negative CER processes and the PD to which it is associated. At the other extreme, optimism can be protective against sleep difficulties, namely through positive reappraisal and refocus on planning and less vulnerability to PD. The latter is the only mediator directly associated with sleep difficulties and a factor present in all processes that link pessimism/optimism to sleep, assuming a central role.
These results show the importance of personality traits, cognition, CER and PD (depression, anxiety and stress) when looking for the factors that contribute to the genesis and maintenance of sleep difficulties. Future research could consider longitudinal data; more complex mediation models with multiple mediators; the bidirectional relationship between optimism and pessimism and sleep difficulties; the control of psychiatric disorder diagnosis and use of psychotropic medication; the use of stricter definitions of sleep difficulties and insomnia; as well as of objective sleep measures (such as actigraphy), which could provide converging evidence for the associations. New doors are also opening for prevention and intervention in PD and its associated comorbidities. Cognitive behaviour therapy and other therapies focussing on intervention in positive or negative expectations about the future and emotion regulation strategies, including strengthened positive CER, could well be very promising solutions to these problems.
Credit authorship contribution statement
Boaventura R. C. R. O. Afonso: Conceptualization; Formal analysis; Investigation; Methodology; Validation; Visualization; Writing - Original Draft; Writing - Review & Editing. Maria João Soares: Conceptualization; Formal analysis; Investigation; Methodology; Resources; Supervision; Validation; Writing - Review & Editing. António Macedo: Project administration; Resources; Supervision; Validation; Writing - Review & Editing.















