Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Psicologia, Saúde & Doenças
versão impressa ISSN 1645-0086
Psic., Saúde & Doenças v.11 n.2 Lisboa 2010
Psychosocial adjustment in infertility: a comparison study of infertile couples, couples undergoing assisted reproductive technologies and presumed fertile couples
Mariana Moura-Ramos1,5, Sofia Gameiro1,2, Isabel Soares3, Teresa Almeida Santos4 & Maria Cristina Canavarro1
1Faculdade de Psicologia e Ciências da Educação da Universidade de Coimbra, Coimbra, Portugal.
2Fertility Studies Research Group, School of Psychology, Cardiff University, U.K.
3Escola de Psicologia, Universidade do Minho, Portugal.
4Faculdade de Medicina da Universidade de Coimbra, Coimbra, Portugal.
5Universidade Lusíada do Porto, Porto, Portugal.
Contactar para Email: marianamr@fpce.uc.pt
Abstract
The aim of the present study was to investigate psychosocial adjustment and infertility related stress of infertile couples and couples undergoing Assisted Reproductive Technologies (ART). In a cross sectional study, 148 couples were recruited: 79 couples undergoing ART, 25 infertile couples in their first medical appointment in an infertility centre and no previous ART treatments and 44 childless couples in reproductive age without infertility history. Measures assessed emotional adjustment, quality of life, marital relationship and infertility stress. Couples were the focus of the analysis. Results indicated that couples undergoing ART presented more adjustment difficulties, especially women. No significant differences were found in marital adjustment, although ART couples idealized their marital relationship to a higher degree. Results are discussed in terms of clinical implications and future research directions.
Keywords: Assisted Reproductive Technologies; emotional adjustment; infertility; In Vitro fertilization; marital relationship, quality of life.
Ajustamento psicossocial na infertilidade: um estudo comparativo de casais inférteis, casais a realizar tratamentos de reprodução medicamente assistida e casais presumidamente férteis
Resumo
O objectivo deste estudo foi investigar o ajustamento psicossocial e o stress associado à infertilidade em casais inférteis e casais que recorreram à Reprodução Medicamente Assistida (RMA). Neste estudo transversal, a amostra foi constituída por 148 casais: 79 casais a realizar tratamento de RMA, 25 casais inférteis, sem tratamentos de RMA anteriores, na sua primeira visita a um serviço de infertilidade e 44 casais em idade reprodutiva, sem filhos e sem história de infertilidade. Foi avaliado o ajustamento emocional, a qualidade de vida, a relação conjugal e o stress associado à infertilidade. Os resultados indicaram que os casais, principalmente as mulheres, que estão a realizar um tratamento de RMA apresentam maiores dificuldades de ajustamento. No que se refere ao relacionamento conjugal, de um modo geral não foram encontradas diferenças, apesar de os casais que recorreram à RMA tenderem a idealizar mais o seu relacionamento conjugal. As implicações clínicas e futuras áreas de investigação são discutidas.
Palavras-chave: Ajustamento emocional e relacional, infertilidade, fertilização In Vitro, qualidade de vida, reprodução medicamente assistida.
Infertility is clinically defined as the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse (Zegers-Hochschild et al., 2009). It is estimated that infertility affects 9% to 10 % of the population worldwide (Boivin, Bunting, Collins, & Nygren, 2007) and a similar prevalence was found in Portugal (Silva-Carvalho & Santos, 2009). At least one-third of couples experiencing infertility will recur to Assisted Reproductive Technology (ART) to achieve parenthood. Undergoing ART can be an emotional and physical burden, affecting emotional adjustment, quality of life (QoL) and marital quality in infertile couples (Eugster & Vingerhoets, 1999). Assessing psychosocial adjustment to ART is important due to its impact in treatment dropout rates (Brandes et al., 2009; Rajkhowa, McConnell, & Thomas, 2006) and to the hypothesized impact of emotional status on treatment outcome. Indeed, some research has shown that psychological distress during treatment affects treatment outcome (Demyttenaere, Nijs, Evers-Kiebooms, & Koninckx, 1992; Smeenk, Verhaak, Stolwijk, Kremer, & Braat, 2004). In order to investigate how couples adjust to infertility and ART treatments, we compared emotional adjustment (emotional reactivity and psychological distress), quality of life, relational adjustment (marital quality and intimacy) and infertility stress between three different groups: a group of couples undergoing ART, a group of infertile couples in their first appointment in an infertility clinic and a group of presumed fertile couples.
The psychosocial impact of infertility
Infertility has been considered a major life crisis in couples, representing the inability to fulfil an important goal in couples’ life: the wish to bear a child. It has been reported that infertile couples can experience emotional and relational difficulties due to infertility diagnosis and its treatment, namely high emotional reactivity and psychological distress, impairment in quality of life, marital problems, and infertility stress and concerns (Cousineau & Domar, 2007; Watkins & Baldo, 2004).
Emotional reactivity and psychological distress have been the two main dimensions assessed in couples’ emotional adjustment to infertility, although some inconsistencies in results have been found. The majority of studies have found that couples, but mainly women, do present higher levels of anxiety and depression than controls (Callan, 1987; Fassino, Pierò, Boggio, Piccioni, & Garzaro, 2002; Wang et al., 2007; Wischmann, Scherg, Strowitzki, & Verres, 2009), although the prevalence of psychological disturbance has no clinical relevance (Anderson, Sharpe, Rattry, & Irvine, 2003; Chachamovich et al., 2009; Nelson, Shindel, Naughton, Ohebshalom, & Mulhall, 2008). It is clear, then, that infertility is associated with some emotional distress, but with no clinical relevance (Greil, 1997; Verhaak et al., 2007).
Even though there is no severe emotional disturbance among infertile couples, several studies have shown that QoL is usually affected by infertility. Fekkes et al. (2003) assessed QoL with the Hopkins Symptoms Checklist (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974) and the Sickness Impact Profile (Bergner, Bobbitt, Carter, & Gilson, 1981), in terms of emotional, social, physical and cognitive functioning, to conclude that young infertile men and women experienced more social and emotional problems than a comparison group of people from the general population, and these differences were smaller for men. Another study (Drosdzol & Skrzypulec, 2008) found lower QoL scores in infertile women compared with presumed fertile women in all dimensions assessed (i.e. general health, health change, physical functioning, role physical, emotional role limitation, social functioning, bodily pain, vitality and mental health). Similar results were found by Monga, Alexandrescu, Katz, Stein and Ganiats (2004) and Nelson et al. (2008). In another study (Chachamovich et al., 2009), results indicated that infertile couples presented lower QoL in the physical, psychological and social relationships domains and higher QoL in environmental domain than healthy controls. Women presented higher QoL in the social relationships domain and lower QoL in psychological domain than their partners.
In summary, studies indicate that infertile couples present lower QoL than controls, although there are discrepancies in dimensions affected. Nevertheless, Ragni et al. (2005) found that although women reported lower QoL than men regarding social functioning, mental health and emotional role limitation, both men and women did not differ from Italian normative data. The authors suggest that gender differences in QoL were not due the infertility problem, but because women tend to report lower scores of health related QoL (Ragni et al., 2005).
Regarding the marital relationship, the field literature points out some inconsistencies in findings, with some studies reporting the stability of the marital relationship (Sydsjo, Ekholm, Wadsby, Kjellberg, & Sydsjo, 2005), while other suggested that infertile couples are more (Callan, 1987) or at least equally satisfied (Wischmann et al., 2009) with their marriage than presumed fertile couples, and some others reported lower scores of marital satisfaction than controls (Monga et al., 2004; Wang et al., 2007).
There is also some evidence that the infertility problem causes marital benefit (Holter, Anderheim, Bergh, & Moller, 2006; Schmidt, Holstein, Christensen, & Boivin, 2005), because infertility is a shared problem, forcing partners to communicate and share feelings about the problem and possible solutions, which promotes closeness and intimacy to the relationship (Greil, Porter, & Leitzo, 1989). Men seem to report higher marital adjustment than women (Slade, Emery, & Lieberman, 1997), although they also feel to a higher degree that treatment affected their marital relationship before and during treatment (Holter et al., 2006).
Although marital quality is usually high in infertile couples, infertility may have a detrimental effect on the couple’s sexual relationship, due to the scheduling and the lack of spontaneity of intercourse, the invasion of privacy by the medical team and because intercourse is a constant reminder of the couple’s inability to conceive (Greil et al., 1989). Indeed, studies focusing in the sexual relationship reported more sexual difficulties and lower sexual satisfaction in infertile women and men than controls (Drosdzol & Skrzypulec, 2008; Monga et al., 2004), although not indicating psychosexual problems (Slade et al., 1997).
The use of standardized measures to assess psychosocial adjustment is important to allow for comparisons of infertile couples with normative data and control groups. However, to better capture the experience of infertility, some studies have also focused on infertility related stress and concerns. Newton, Sherrard and Glavac (1999) found that men and women who reported greater infertility global stress also reported higher levels of depression. Specifically, more symptoms of distress were highly correlated with social, sexual and relationship concerns. Relationship and sexual concerns were related to problems in the marital adjustment. Infertility global stress was also associated with anxiety in both men and women. Similarly, in Fekkes et al. study (2003), a higher level of irrational beliefs about parenthood was related to higher levels of problematic functioning.
In a study assessing infertility concerns (Anderson et al., 2003), more of one quarter of women endorsed infertility related concerns about life satisfaction, control over life, self esteem, sexuality and self blame (in men, this happen only related to life satisfaction), and as in Newton et al. study (1999) total concern score was related to depression.
In summary, studies indicate that infertile couples experience some emotional difficulties, not clinically relevant, and have good and stable marital relationships, nevertheless reporting a deleterious effect of infertility in QoL, sexual dimension of the marital relationship and infertility stress.
ART treatment and its impact on the wellbeing of couples
A substantial amount of infertile couples will recur to ART to achieve parenthood. Undergoing ART is expensive (Mazure & Greenfeld, 1989), time consuming, interferes with professional life (Bouwmans et al., 2008) and is emotionally and physically demanding (Eugster & Vingerhoets, 1999). These procedures require a stimulation stage (self injected hormonal treatment and monitoring through regular ovarian ultrasounds and blood analysis), oocyte retrieval and embryo transfer stage, two weeks waiting period and a final a pregnancy test, to assess treatment outcome, even though clinical pregnancy needs to be confirmed later by a vaginal ultrasound (for more detailed description of the treatment, see Boyle, Vlahos, & Jarow, 2004; Santos & Moura-Ramos, 2010). Therefore, when considering emotional assessment before or during ART procedures, the precise phase of the treatment when the assessment occurs may affect research results.
In Reading, Chang and Kerin study (1989), women were assessed in the day 8 of the stimulation phase and results indicated that 20% of women presented clinical signs of anxiety and depression and scored higher on fatigue and lower in vigour than controls group. Similarly, another study (Volgsten, Skoog Svanberg, Ekselius, Lundkvist, & Poromaa, 2008) found that about 30% of infertile women and 10% of infertile men fulfilled criteria for a depressive and/or anxiety disorder during the oocyte retrieval stage and Yong, Martin, and Thong (2000) reported similar anxiety scores the days before oocyte retrieval and pregnancy test. In a study that aimed to examine daily emotional, physical and social reactions in men and women during all the IVF or ICSI treatment (Boivin & Takefman, 1996), results found that distress but also optimism were higher during oocyte retrieval and the embryo transfer stage and on the pregnancy test day. The authors consider that the uncertainty related to treatment procedures is the most important determinant of reactions during IVF, namely trying to find out if each stage has passed was successful. The authors also highlighted that although women are more distressed than their partners, the type and pattern of couple’s reactions were very similar, and differences that were found, namely higher reported in fatigue in women, can be explain by the procedures per se (Boivin et al., 1998).
In summary, although couples entering treatment are in general well adjusted (Eugster & Vingerhoets, 1999), there is a great variability in adjustment along the treatment (Boivin & Takefman, 1996) (Eugster & Vingerhoets, 1999; Greil, 1997; Hammarberg, Astbury, & Baker, 2001; Verhaak et al., 2007). It is then expected that assessments carried out during treatment will indicate higher distress than assessment prior or in the beginning of the treatment.
Research on infertility and ARTin Portugal
Although the use of ART has been widely undertaken in Portugal since 1985, its legal framework has just recently been approved in 2006 (Law no. 32/2006), regulated in 2008 (Decree no. 5/2008) and further developed in 2009 (Judgment no. 101/2009). Similarly, financial Government assistance to couples undergoing ART only began in July of 2009 (Order no.10910/2009), after the collection of the data which served as basis for this paper.
Until recently, there were few studies on infertility and ART in Portugal and very few were dedicated to the psychological experience. Studies published have focused on characterization of oocyte donors (Pereira & Leal, 2005) and of pregnancy and transition to parenthood after ART (Gameiro, 2009; Gameiro, Moura-Ramos, Canavarro, & Soares, 2009, 2010). The first sociological approach to infertility and the first epidemiological study about its prevalence in Portugal were also published recently (Remoaldo & Machado, 2008; Silva-Carvalho & Santos, 2009). Therefore, there has been a recent but growing interest about infertility in Portugal, although there are still few studies concerning the psychological adjustment of infertile couples, both before and while they are undergoing treatment.
In the present study, we examined the psychosocial adjustment of three groups of Portuguese couples: infertile couples, couples undergoing ART and presumed fertile couples. The group of presumed fertile couples was included for reference purposes. Adjustment was assessed with measures of emotional reactivity and psychological distress, quality of life, marital quality and infertility stress. Specifically, first we aimed to compare the three groups regarding women and men’s emotional and marital adjustment and quality of life. We considered the couple as the unit of analysis so that the interdependence that is known to exist between two members of a couple could be accounted for (Kenny, Kashy, & Cook, 2006). Second, we aimed to identify the dimensions of psychosocial distress and infertility stress that best discriminate between groups.
For our first aim, we defined the hypotheses for group differences in our study as follows:
1. There will be differences in emotional adjustment among the three groups: Couples undergoing ART will present higher positive and negative emotional reactivity than presumed fertile couples. Infertile couples will present higher negative emotionality than presumed fertile couples. Women will present higher negative emotional reactivity than men; Couples undergoing ART are expected to present higher psychological distress than infertile and presumed fertile couples, and this difference is expected to be higher for women.
2. Infertile couples and couples undergoing ART will present lower QoL than presumed fertile couples.
3. Infertile couples and couples undergoing ART will present higher marital quality and intimacy than presumed fertile couples. Infertile couples and couples undergoing ART will present higher difficulties in sexual relationship than presumed fertile couples;
4. Infertile couples will present higher infertility stress than presumed fertile. For our second aim, we defined our hypothesis as follows:
5. Emotional adjustment dimensions and quality of life will discriminate couples undergoing ART from the other groups;
6. Higher marital satisfaction will discriminate infertile couples and couples undergoing ART from presumed fertile;
7. Worse adjustment of women will contribute to discriminate between couples undergoing ART from infertile and presumed fertile couples.
METHOD
Participants
A total 174 women and 148 men responded to the assessment protocol. Because both partners participation was required to perform dyadic analysis, 148 couples were included in final sample. All couples were married or cohabiting for at least one year. Three different groups were composed: 79 couples undergoing ART (ART Group), 25 infertile couples (Infertile Group) attending their first medical appointment in an infertility medical centre, and 44 presumed fertile couples (PF Group). Sample characteristics are presented in Table 1.
Table 1
Participants’ characteristics
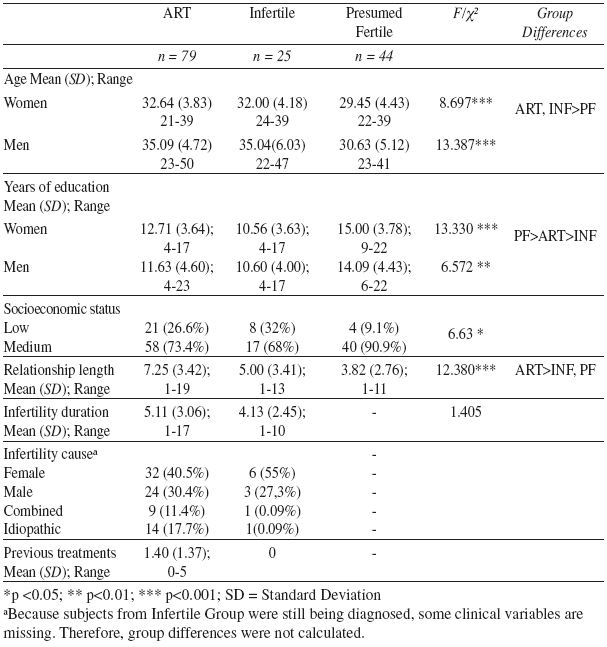
Couples undergoing ART and Infertile couples were older than PF couples. ART couples have been longer in a relationship when compared with Infertile and PF couples. There were also differences related to years of education and socioeconomic status. Infertile couples had the lower years of education and PF group had the largest proportion of couples from the medium level of socioeconomic status.
Measures
Socio-demographic and clinical form. This form included socio-demographic data (age, length of relationship, years of education, profession and socioeconomic status) and clinical data (infertility duration, infertility cause and number of previous ART treatments). Socioeconomic status (SES) was measured using a standardized classification developed for Portuguese population, considering low, medium and high categories (Simões, 1994). Clinical information regarding infertility history and treatment procedures was obtained from the patients’ medical records.
Emotional adjustment was assessed with the Emotional Assessment Scale and the Depression, Anxiety and Somatization subscales of the Brief Symptom Inventory.
The Emotional Assessment Scale (EAS) (Carlson et al., 1989; Portuguese version by Moura-Ramos, 2006) is a 24item (emotions) scale where subjects are asked to mark how much they feel at the moment on a 10 cm analogical scale. The Portuguese version of the scale revealed seven factors: anxiety, happiness, fear, guilt, anger, surprise and sadness, with good internal consistency reliability and good construct validity (cf. Moura-Ramos, 2006). Cronbach alpha coefficients ranged from .80 to .89 for ART group, .75 to .84 for infertile group and .63 to .91 for the PF group. In the present study, surprise was not considered because of low internal consistency in one group (α<.60).
The Brief Symptom Inventory (BSI) (Derogatis, 1993; Portuguese version by Canavarro, 1999). In this 53item scale, participants were asked to assess the frequency of specific symptoms during the past week on a 5point scale (0Never to 5Very often). In the present sample, subscales Cronbach alpha coefficients ranged from .76 to .96 for ART group, .82 to .98 for infertile group and .71 to .95 for the PF group.
Quality of life (QoL) was assessed with the World Health Organization Quality of Life Bref instrument WHOQoLbref (WHOQoLGROUP, 1995; Portuguese Version by Vaz Serra et al., 2006). This is a 5point scale with 26 items that assess QoL in relation to four specific domains (physical, psychological, social relationships and environment). In the present sample, Cronbach alpha coefficients for subscales ranged from .71 to .80 for ART group, .73 to .86 for infertile group and .64 to .81 for the PF group.
Marital quality was assessed with the ENRICH Marital Inventory (ENRICH) and personal validation, communication and open to the exterior Scale (PAIR).
The ENRICH (Olson, Fournier, & Druckman, 1983; Portuguese version by Lourenço, 2006) is a multidimensional scale with different facets contributing to overall satisfaction in marital relationship. It comprises 109 items with a 5point scale that provides summed scores of the women and men’s evaluation of their relationship. Cronbach alpha coefficients ranged from .69 to .82 for ART group, .68 to .83 for infertile group and .72 to .79 for the PF group. In the present study, egalitarian roles subscale was not used due to low internal consistency (α<.60).
The PAIR (Schaefer & Olson, 1981; Portuguese version by Moreira, Amaral, & Canavarro, 2009) assesses the degree of intimacy in a dyadic relationship in a 36item 5point scale. The Portuguese version has three factors: personal validation, communication and open to the exterior. The PAIR also includes a conventionality scale to assess social desirability in the subjects’ responses. Cronbach alpha coefficients ranged from .69 to .85 for ART group, .83 to .89 for infertile group and .78 to .85 for the PF group. Communication and open to the exterior subscales were not used in this study because of low internal consistency scores in one of the groups (α<.60).
Infertility Stress was assessed with the Fertility Problem Inventory (FPI) (Newton et al., 1999; Portuguese version by Moura-Ramos, Gameiro, & Canavarro, 2008). In this 46item scale, participants are asked to rate how much they agree or disagree with fertility related concerns or beliefs and responses are given in 6point scale. In the present sample, Cronbach alpha coefficients for these subscales ranged from .72 to .82 for ART group and .74 to .78 for infertile group. Relationship concern and rejection of childfree lifestyle subscales were not used because of low internal consistency in one of the groups (α<.60). This scale was not administered to the PF Group.
Procedures
Participants from ART and infertile groups were invited to participate in the study during a routine appointment with the psychologist at the Genetics and Human Reproduction Service in Coimbra University Hospitals and Reproductive Medicine in the Vila Nova de Gaia Central Hospitals. Ethical approval was obtained from both hospitals’ Research Ethics Committees. Participants from the infertile group were recruited during their first appointment in the Hospital, to which they had been referred to due to inability to conceive after for more than one year. Couples undergoing ART procedures were recruited in the beginning of ART, during hormonal simulation phase (6th8th day). At these points, information regarding infertility or ART process was given to the couples and participation in the study was asked. Study participants did not received psychological intervention. Inclusion criteria were age (18 years or older), history of infertility and literacy skills to complete the assessment protocol. PF couples were recruited from general population by convenience procedures. Inclusion criteria were having between 2040 years, being childless and not being pregnant or trying to get pregnant at that moment.
When recruiting participants, a full explanation of the research objectives, the participants’ role and the researchers’ obligations was given. If participants agreed to collaborate, they filled out an informed consent form.
Data analyses
Data analyses were performed using the couple as a unit. The database was restructured in order to consider each couple as the subject of the analysis and each partner score was a different variable. Analysis of covariance using the General Linear Model (GLM) for Repeated Measures were performed, more specifically MANCOVAs (for multivariate analysis) and ANCOVAs (for total scores), with Group (1 – ART, 2 – Infertile, and 3 – PF) as the between-subjects factor and Gender (1 Women, 2 Men) as the within subjects factor, so that within couple differences could be explored (Kenny et al., 2006). Years of education and SES were inserted as covariates in all the analysis. Age and length of relationship were not inserted as covariates because were considered as defining characteristics of the groups.
Pillai’s trace criterion was used because of its robustness with unequal samples sizes (Tabachnick & Fidell, 2007). When effects were found, post-hoc analysis using Bonferroni procedures were performed to detect group and gender differences.
Effect sizes are presented in all analysis using partial eta squares (ηp2), which can be interpreted as the proportion of total variation attributable to the factor, partialling out (excluding) other factors from the total non-error variation. Effects sizes were considered: η2 = .01 a small effect size, .06 a medium effect size and .14 large effect size (Kittler, Menard, & Phillips, 2007). Posthoc power calculations demonstrated that the achieved sample size was sufficient to detect medium to large effects [f=.30, p<.05, power = .90, G*Power 3] (Faul, Erdfelder, Lang, & Buchner, 2007). Significance level used was .05. However, because small effects would not be detected, marginally significant differences (p<0.1) will also be reported and discussed. Finally, to identify the best dimensions that help to classify group membership, three discriminant function analyses (DFA) were performed.
RESULTS
There were no significant differences in any adjustment measures between women whose spouses did or did not participate in the study (data not presented). Table 2 presents the descriptive (estimated marginal means, accounting for the covariates, and standard errors) of adjustment measures and multivariate and univariate main and interaction effects. Means ± standard deviations for significant results for men and women are presented in text.
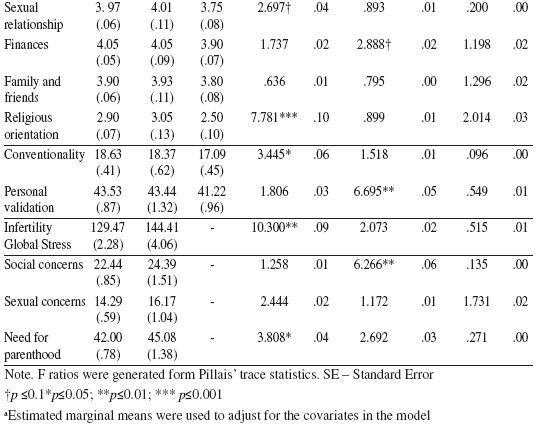
Table 2
Descriptives, Multivariante Main and Interaction Effects and Univariate analysis
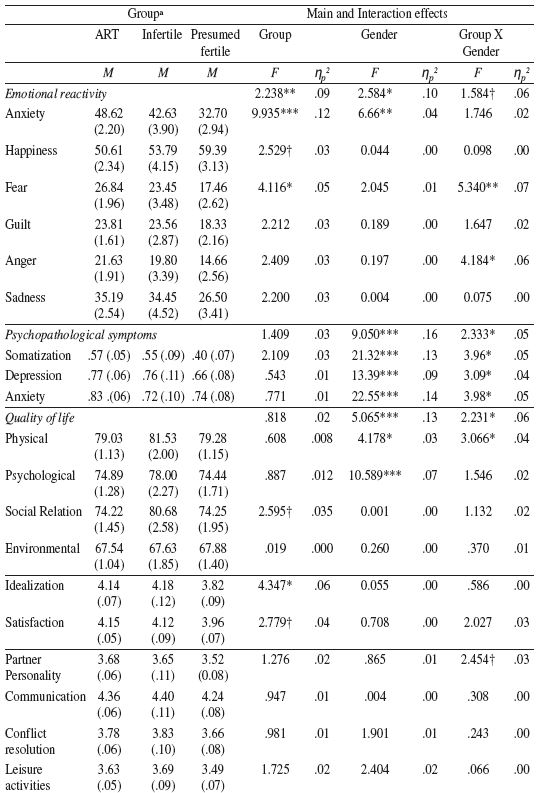
Emotional reactivity
The multivariate group effect for emotional reactivity was significant, indicating that ART couples have higher anxiety and fear than PF couples. There was also a within-subjects multivariate effect, indicating that women presented higher anxiety than men [44.30±2.18 vs. 38.34±2.07, respectively]. A multivariate Gender X Group interaction effect with marginally significant trend was also found, indicating that ART women presented higher fear and anger than ART men [Fear: 32.35±2.90 vs. 21.33±2.25, p<.05; Anger: 24.69±3.06 vs. 15.87± 2.20, p<.001, respectively].
Psychological distress
About 15.6% of ART and 12.0% of infertile women scored above norms (considered Mean ± 1 Standard Deviation) in anxiety, against 4.2% of presumed fertile women. In depression, these percentages were 16.5%, 20% and 13.6%, respectively. Although indicating higher prevalence of depression in infertile couples and anxiety in ART women, differences were not statistically significant. Similar results were found in men.
No multivariate group effect was found. A gender main effect was found, indicating that women presented higher levels of somatization, depression and anxiety than men [Somatization=.64±.06 vs. .38± .04; Depression=.85±.07 vs. .61±.05, Anxiety=.91±.07 vs. .62±.04, respectively]. These gender effects were classified by interactions effects. Univariate analysis indicated that ART women have higher scores on somatization [Somatization=.78±.08 vs. .37± .05; F (1,74) = 33.36, p<.001, ηp2= .31] than ART men. Women in ART and PF groups reported higher depression than men [ART Group: .98±.09 vs. .55± .06, respectively, F (1,78) = 29.183, p≤..001, ηp2= .27] and PF group: .78±.09 vs. .54± .07, respectively, F (1,43) = 5.296, p≤.05, ηp2= .11]. The same results were found in anxiety [ART Group: 1.08±.08 vs. .58± .05; respectively, F (1,78) = 43.276, p≤.001, ηp2= .36; PF Group: =.83±.07 vs. .64±.07 respectively; F (1,43) = 4.103, p≤.05, ηp2= .09]. Noteworthy, gender differences were much larger and significant in ART group than in PF Group. No gender differences were found in Infertile Group.
Quality of life
No differences were found between groups. However, a gender main effect and a Gender X Group interaction effect were found. Gender differences show that women had lower QoL in Psychological domain than men [73.46±2.18 vs. 78.10±1.3, respectively]. A Gender X Group interaction effect was found, indicating that ART women had lower QoL in physical domain than ART men [75.92±1.50 vs. 82.14±1.22, respectively, F(1,74) =15.804, p≤.001, ηp2 = .18].
Marital relationship
A main effect for Group was found in idealistic distortion. Post hoc comparisons indicated that couples undergoing ART presented higher levels of social desirability when compared to PF couples (p=.022). Similarly, a marginally significant trend was found when comparing infertile couples and PF (p=.066), pointing in the same direction.
Regarding marital satisfaction, a marginally significant group main effect was found, indicating that couples undergoing ART presented higher scores than presumed fertile couples (p=.065).
A group main effect marginally significant trend was found. Univariate analysis indicated that there were significant differences in religious orientation between ART and infertile couples when compared to PF couples (p=.003 and p=.002), respectively.
Intimacy in the relationship
A main effect for group was found in conventionality, indicating that ART couples presented higher scores than PF couples (p=.036). In personal validation, a gender main effect was found, indicating that women presented higher scores than men [43.59±.66 vs. 41.87±.74, respectively].
Infertility stress
A group main effect was found in the global stress, indicating that infertile group
presented higher stress than ART couples (p=.002). A multivariate gender effect marginally significant was found, indicating that women presented more social concerns than men [24.61±1.04 vs. 22.21±.93, respectively].
Identification of the dimensions discriminating among groups
Only variables that presented group main effects or interaction effects in previous MANOVAs were included in the DFA model. Variables were considered to discriminate among groups if they loaded on the structure matrix above .3 (Tabachnick & Fidell, 2007).
Table 3
Discriminant functions between ART group, Infertile group and Presumed Fertile group
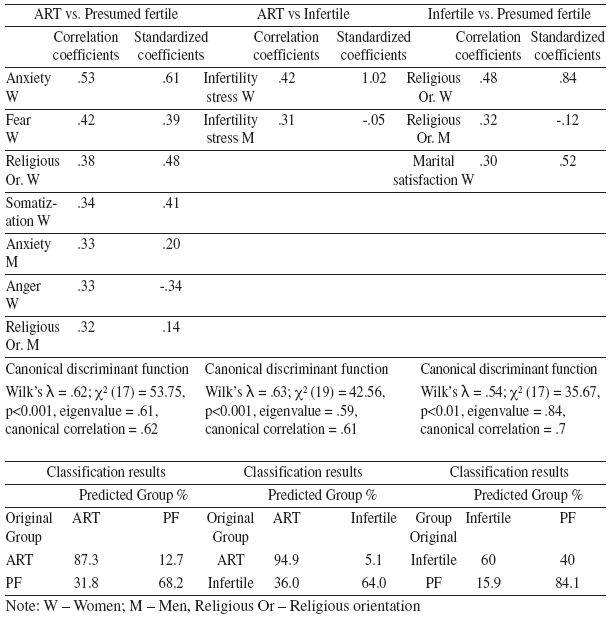
The best discriminating variables between ART group and PF group are related to emotional reactivity in women, namely anxiety and fear, partially confirming our first and sixth hypothesis. Religious orientation in both partners was also a discriminant factor. This discriminant function allowed for the correct identification of 87.7% of the ART Group and 68.2% of the PF group. Concerning the comparison of couples undergoing ART and Infertile couples, infertility global stress in both partners was the best discriminant factor. The discriminant factor allowed the correct identification of 94.9% of the ART group and 64% of the infertile group. Religious orientation of both partners and women’s marital satisfaction discriminated Infertile and presumed fertile couples, allowing for the correct identification of 60% and 84.1% of cases, respectively. Our hypothesis 5 was partially confirmed.
DISCUSSION
The present study aimed at describing the adjustment of Portuguese infertile couples and couples undergoing ART. For this purpose we used a couple based analytical approach with a comparative design. The main finding of our study was that couples undergoing ART presented more emotional adjustment difficulties. This has proved to be especially true for women undergoing ART, who presented higher negative emotionality, more depressive, anxious and somatic symptoms and lower physical quality of life than their spouses. In summary, undergoing ART procedures may cause high physical discomfort and emotional distress in both members of the couple but especially in women, who are subjected to most treatment procedures. The results suggest that treatments may be demanding event for couples, but especially for women, and that they may thus beneficiate more from professional help during this phase.
When comparing infertile couples with presumed fertile couples, there are more similarities than differences. Results suggest no differences in couples’ adjustment, with the exception of marital quality. As previously hypothesized, results suggest that infertile couples and couples undergoing ART are more satisfied with their marital satisfaction than presumed fertile. Additionally, both infertile couples and couples undergoing ART presented higher scores in religious orientation, which reflects a more conservative conception of life and religious values (Olson et al., 1983), which was an important dimension discriminating among group membership, suggesting that, for couples suffering from infertility, traditional roles of parenthood may be of foremost importance.
Nevertheless, when studying adjustment to ART treatment, some differences were salient, confirming our hypotheses. Women undergoing ART procedures presented higher levels of somatic symptoms and low physical quality of life. This may be due to the treatment effects, because by the time of this assessment women are undergoing hormonal stimulation and other medical procedures, which may cause physical discomfort and pain (Boivin et al., 1998; Boivin & Takefman, 1996). Additionally, women undergoing ART and those presumed fertile women are more depressed and anxious than their partners. Although this can be interpreted as a illusory gender effect, as suggested by Edelmann and Conolly (2000), differences are much higher in couples undergoing ART, suggesting that heightened emotional disturbance may be due to the impact of undergoing ART treatment. It is important to acknowledge that women are usually much more involved with the treatment because they are the ones who are submitted to most of the medical procedures and are more frequently in contact with the fertility centre, and therefore, it is expected its impact to be higher. Nevertheless, even considering that a considerate amount of participants presented emotional disturbance, these results were not significantly different from controls, as reported by other studies (Anderson et al., 2003; Chachamovich et al., 2009; Nelson et al., 2008).
The impact of ART treatment seems to affect much more the emotional adjustment than other areas of the couples’ life. Indeed, no differences were found in social relationships or environmental domains and the differences in marital quality are indicative of a better relationship in couples undergoing ART when compared to presumed fertile couples, suggesting that infertility and ART do not have a negative impact in marital quality, but, conversely, my enhance partnership and intimacy in the relationship (Greil et al., 1989), mainly for couples undergoing ART, which, as suggested by these authors, have had to communicate and to work on solutions to the infertility problem.
However, although these findings confirm our hypothesis, they should be interpreted cautiously due to the infertile and undergoing ART couples’ tendency to respond in a social desirable manner. The tendency, already described elsewhere (Greil, 1997), although not found in Wischmann et al. (2009) study , was reported by participants in our study: when assessing their marital relationship and intimacy, both couples undergoing ART and infertile presented higher levels of idealistic distortion and conventionality than presumed fertile couples. Although idealization of the partner can be an important ingredient of couples’ satisfaction (Murray, Holmes, & Griffin, 1996), we should not exclude that results concerning marital satisfaction could be partially explained by a tendency to present a better relationship.
In summary, our results are consistent with the occidental field literature, suggesting there are more similarities than differences in infertile and presumed fertile couples (Greil, 1997; Verhaak et al., 2007). Additionally, undergoing ART seems to be a very demanding experience, affecting emotional reactivity and causing great distress, although without clinical relevance and not affecting other areas of couples’ life. As described in the literature, infertility may cause marital benefit, leading to higher marital satisfaction among infertile couples. However, this may be truer in couples with longer infertility and more treatment experiences, who have learnt to cope better with their childlessness, and to experience less distress and more intimacy, than couples just entering in infertility medical setting (Fekkes et al., 2003; Greil et al., 1989).
The use of two different groups of infertile couples and a group of presumed fertile couples, different measures of psychosocial adjustment and infertility stress, namely general and infertility specific measures, and a design accounting for the non-indenpendence of the couples’ scores are three major strengths of the present paper. Additionally, because no previous research on psychosocial adjustment of Portuguese infertile couples’ recurring to ART had been published, our results contributed to a better understanding of the Portuguese infertile couples and couples recurring to ART.
However, some limitations should also be addressed. First of all, it has been acknowledged that there is great variability in adjustment to infertility and ART, depending on age, duration of infertility, number of previous treatments, years of education, so future research should focus on the impact of these variables in psychological and marital adjustment. Additionally, the small sample sizes in each group can highly limit the generalization of the present results. The small sample size also reduced power in the analysis, only allowing the detection of medium to large effects and therefore not identifying small effects, which can inflate the risk of Type II error (accepting a false null hypothesis). To reduce type II error, marginally significant linear trends were reported, allowing to hypothesize that differences would have been found if the sample was larger.
Our results can have important implications for clinical practice with couples referred to ART. Even considering that before entering treatment couples have similar adjustment compared to controls, the initiation of the treatment accentuates some adjustment difficulties, namely in women. The impact of the invasive medical procedures and the constraints in professional life associated with expectancies related to the success of the treatment highlight patients’ negative emotions like anxiety and stress. Fertility centre healthcare providers should develop efforts to minimize emotional difficulties among couples recurring to IVF in order to promote a better adjustment to IVF procedures, by providing psychoeducative information regarding the IVF process, namely its physical and emotional demands; because there is great variability in couples’ adjustment, efforts should be made to target interventions to the couples’ needs. Decreasing psychological distress and negative emotionality during treatment can be important in reducing dropout rates and in improving IVF success rates (Demyttenaere et al., 1992; Smeenk, Verhaak, Eugster, & van Minnen, 2001). Future research should address effects of different treatment strategies in psychosocial impact (Verberg et al., 2008) and other predictors of adjustment during the IVF procedure. Recognition of all the factors that have an impact on couples’ adjustment can help professionals designing intervention strategies targeted to the identified needs.
REFERENCES
Anderson, K. M., Sharpe, M., Rattray, A., & Irvine, D. S. (2003). Distress and concerns in couples referred to a specialist infertility clinic. Journal of Psychosomatic Research, 54, 353355. doi: 10.1016/S00223999(02)003987
Bergner, M., Bobbitt, R. A., Carter, W. B., & Gilson, B. S. (1981). The sickness impact profile: Development and final revision of a health status measure. Medical Care, 19, 787805.
Boivin, J., Andersson, L., Skoog-Svanberg, A., Hjelmstedt, A., Collins, A., & Bergh, T. (1998). Psychological reactions during in-vitro fertilization: Similar response pattern in husbands and wives. Human Reproduction, 13, 32623267.
Boivin, J., Bunting, L., Collins, J. A., & Nygren, K. G. (2007). International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Human Reproduction, 22, 15061512. doi: 10.1093/humrep/dem046
Boivin, J., & Takefman, J. E. (1996). Impact of the in-vitro fertilization process on emotional, physical and relational variables. Human Reproduction, 11, 903907.
Bouwmans, C. A., Lintsen, A. M., Maiwen, A., Verhaak, C. M., Eijkemans, M. J., Habbema, J. D., Hakkaart-Van Roijen, L. (2008). Absence from work and emotional stress in women undergoing IVF or ICSI: An analysis of IVF-related absence from work in women and the contribution of general and emotional factors. Acta Obstetricia et Gynecologica Scandinavica, 87, 11691175. doi: 10.1080/00016340802460305
Boyle, K. E., Vlahos, N., & Jarow, J. P. (2004). Assisted reproductive technology in the new millennium: Part II. Urology, 63, 217224.
Brandes, M., van der Steen, J. O., Bokdam, S. B., Hamilton, C. J., de Bruin, J. P., Nelen, W. L., & Kremer, J. A. (2009). When and why do subfertile couples discontinue their fertility care? A longitudinal cohort study in a secondary care subfertility population. Human Reproduction, 24, 31273135. doi: 10.1093/humrep/dep340
Callan, V. J. (1987). The personal and marital adjustment of mothers and of voluntary and involuntary childless wives. Journal of Marriage and the Family, 49, 847856.
Canavarro, M. C. (1999). Inventário de sintomas psicopatológicos: BSI. In M. R. Simões, M. M. Gonçalves, & L. S. Almeida (Eds.), Testes e provas psicológicas em Portugal (Vol. 2, pp. 95109). Braga: APPORT.
Carlson, C. R., Collins, F. L., Stewart, J. F., Porzellius, J., Nitz, J. A., & Lind, C. O. (1989). The assessment of emotional reactivity: A scale development and validation study. Journal of Psychopathology and Behavioral Assessment, 11, 313325.
Chachamovich, J., Chachamovich, E., Fleck, M. P., Cordova, F. P., Knauth, D., & Passos, E. (2009). Congruence of quality of life among infertile men and women: Findings from a couple-based study. Human Reproduction, 24, 21512157. doi: 10.1093/humrep/dep177
Cousineau, T. M., & Domar, A. D. (2007). Psychological impact of infertility. Best Practice & Research in Clinical Obstetrics and Gynaecology, 21, 293308. doi: 10.1016/j.bpobgyn.2006.12.003
Demyttenaere, K., Nijs, P., Evers-Kiebooms, G., & Koninckx, P. R. (1992). Coping and the ineffectiveness of coping influence the outcome of in vitro fertilization through stress responses. Psychoneuroendocrinology, 17, 655665.
Derogatis, L. R., Lipman, R. S., Rickels, K., Uhlenhuth, E. H., & Covi, L. (1974). The Hopkins symptom checklist (HSCL): A self-report symptom inventory. Behavioral Science, 19, 115.
Derogatis, L. R. (1993). BSI: Brief Symptom Inventory: Administration, scoring and procedures manual. Minneapolis, MN: National Computers Systems.
Drosdzol, A., & Skrzypulec, V. (2008). Quality of life and sexual functioning of Polish infertile couples. The European Journal of Contraception and Reproductive Health Care, 13, 271281. doi: 10.1080/13625180802049187
Edelmann, R. J., & Connolly, K. J. (2000). Gender differences in response to infertility and infertility investigations: Real or illusory? British Journal of Health Psychology, 5, 365375.
Eugster, A., & Vingerhoets, A. J. (1999). Psychological aspects of in vitro fertilization: a review. Social Science & Medicine, 48, 575589.
Fassino, S., Pierò, A., Boggio, S., Piccioni, V., & Garzaro, L. (2002). Anxiety, depression and anger suppression in infertile couples: A controlled study. Human Reproduction, 17, 29862994.
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175191.
Fekkes, M., Buitendijk, S. E., Verrips, G. H., Braat, D. D., Brewaeys, A. M., Dolfing, J. G., Macklon, N. S. (2003). Health-related quality of life in relation to gender and age in couples planning IVF treatment. Human Reproduction, 18, 15361543. doi: 10.1093/humrep/deg276
Gameiro, S. (2009). The relational ecology of the transition to parenthood in couples that conceived spontaneously or through Assisted Reproductive Technologies. Unpublished Doctoral Dissertation. Universidade de Coimbra. Coimbra, Portugal.
Gameiro, S., Moura-Ramos, M., Canavarro, M. C., & Soares, I. (2009). Desfechos do parto e depressão pós-parto em mulheres que recorreram a técnicas de reprodução medicamente assistida. Acta Obstétrica e Ginecológica Portuguesa, 3, 134142. [ Links ]
Gameiro, S., Moura-Ramos, M., Canavarro, M. C., & Soares, I. (2010). Psychosocial adjustment during the transition to parenthood of Portuguese couples who conceived spontaneously or through ART. Reseachin Nursing and Health, 33, 207220.
Greil, A. L. (1997). Infertility and psychological distress: A critical review of the literature. Social Science & Medicine, 45, 16791704.
Greil, A. L., Leitzo, T. A., & Porter, K. L. (1989). Sex and intimacy among infertile couples. Journal of Psychology and Human Sexuality, 2, 117138.
Hammarberg, K., Astbury, J., & Baker, H. W. G. (2001). Women’s experience of IVF: A follow-up study. Human Reproduction, 16, 374383. doi: 10.1093/humrep/16.2.374
Holter, H., Anderheim, L., Bergh, C., & Moller, A. (2006). First IVF treatment: short-term impact on psychological wellbeing and the marital relationship. Human Reproduction, 21, 32953302. doi: 10.1093/humrep/del288
Kenny, D. A., Kashy, D. A., & Cook, W. L. (2006). Dyadic data analysis. New York: The Guilford Press.
Kittler, J. E., Menard, W., & Phillips, K. A. (2007). Weight concerns in individuals with body dysmorphic disorder. Eating Behaviors, 8, 115120.
Lourenço, M. (2006). Casal: Conjugalidade e ciclo evolutivo. Unpublished Doctoral Dissertation. University of Coimbra. Coimbra, Portugal.
Mazure, C. M., & Greenfeld, D. A. (1989). Psychological studies of in vitro fertilization/embryo transfer participants. Journal of in Vitro Fertilization and Embryo Transfer, 6, 242256.
Monga, M., Alexandrescu, B., Katz, S. E., Stein, M., & Ganiats, T. (2004). Impact of infertility on quality of life, marital adjustment, and sexual function. Urology, 63, 126130.
Moreira, H., Amaral, A., & Canavarro, M. C. (2009). Adaptação do personal assessment of intimacy in relationships scale (PAIR) para a população Portuguesa: Estudo das suas características psicométricas. Psychologica, 50, 353373. [ Links ]
Moura-Ramos, M. (2006). A adaptação materna e paterna ao nascimento de um filho: Percursos e contextos de influência. Unpublished Masters Thesis. Universidade de Coimbra.
Moura-Ramos, M., Gameiro, S., & Canavarro, M. C. (2008). Inventário de problemas de fertilidade: Características psicométricas da versão portuguesa do Fertility Problem Inventory. Proceedings da XIII Conferência Internacional de Avaliação Psicológica: Formas e Contextos, Braga, Portugal.
Murray, S. L., Holmes, J. G., & Griffin, D. W. (1996). The benefits of positive illusions: Idealization and the construction of satisfaction in close relationships. Journal of Personality and Social Psychology, 70, 7998.
Nelson, C. J., Shindel, A. W., Naughton, C. K., Ohebshalom, M., & Mulhall, J. P. (2008). Prevalence and predictors of sexual problems, relationship stress, and depression in female partners of infertile couples. Journal of Sexual Medicine, 5, 1907–1914. doi: 10.1111/j.17436109.2008.00880.x
Newton, C. R., Sherrard, W., & Glavac, I. (1999). The fertility problem inventory: Measuring perceived infertility-related stress. Fertility and Sterility, 72, 5472.
Olson, D. H., Fournier, D. G., & Druckman, J. M. (1983). Assessing marital and premarital relationships: The PREPARE/ENRICH Inventories. In E. E. Filsing (Ed.), Marriage and Family Assessment (pp. 229250). Newsbury, CA: Sage Publications.
Pereira, A. O., & Leal, I. P. (2005). Dadoras de ovócitos: Quem são? Análise Psicológica, 23, 269276. [ Links ]
Ragni, G., Mosconi, P., Baldini, M. P., Somigliana, E., Vegetti, W., Caliari, I., & Nicolosi, A. E. (2005). Health-related quality of life and need for IVF in 1000 Italian infertile couples. Human Reproduction, 20, 12861291.
Rajkhowa, M., McConnell, A., & Thomas, G. E. (2006). Reasons for discontinuation of IVF treatment: A questionnaire study. Human Reproduction, 21, 358363.
Reading, A. E., Chang, L. I., & Kerin, J. F. (1989). Psychological state and coping styles across an IVF treatment cycle. Journal of Reproductive & Infant Psychology, 7, 95103.
Remoaldo, P., & Machado, H. (2008). O sofrimento oculto: Causas, cenários e vivências de infertilidade. Porto: Afrontamento.
Santos, A. T., & Moura-Ramos, M. (2010). Esterilidade e procriação medicamente assistida. Coimbra: Imprensa da Universidade de Coimbra.
Schaefer, M., & Olson, D. (1981). Assessing intimacy: The PAIR inventory. Journal of Marital and Family Therapy, 7, 4760.
Schmidt, L., Holstein, B. E., Christensen, U., & Boivin, J. (2005). Does infertility cause marital benefit? An epidemiological study of 2250 women and men in fertility treatment. Patient Education and Counseling, 59, 244251.
Silva-Carvalho, J. L., & Santos, A. (2009). Estudo Afrodite: Caracterização da infertilidade em Portugal (Vol. 1. Estudo na Comunidade). Porto: Faculdade de Medicina da Universidade do Porto.
Simões, M. (1994). Investigações no âmbito da aferição nacional do teste das Matrizes Progressivas de Raven Unpublished Doctoral Dissertation. Universidade de Coimbra. Coimbra, Portugal.
Slade, P., Emery, J., & Lieberman, B. A. (1997). A prospective, longitudinal study of emotions and relationships in in-vitro fertilization treatment. Human Reproduction, 12, 183190. doi: 10.1093/humrep/del288
Smeenk, J. M., Verhaak, C. M., Eugster, A., & van Minnen, A. (2001). The effect of anxiety and depression on the outcome of in-vitro fertilization. Human Reproduction, 16, 14201423.
Smeenk, J. M., Verhaak, C. M., Stolwijk, A. M., Kremer, J. A., & Braat, D. D. (2004). Reasons for dropout in an in vitro fertilization/intracytoplasmic sperm injection program. Fertility and Sterility, 81, 262268. doi: 10.1016/j.fertnstert.2003.09.027
Sydsjo, G., Ekholm, K., Wadsby, M., Kjellberg, S., & Sydsjo, A. (2005). Relationships in couples after failed IVF treatment: A prospective follow-up study. Human Reproduction, 20, 19521957. doi: 10.1093/humrep/deh882
Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics. (5th ed.). Boston: Pearson.
Vaz Serra, A., Canavarro, M. C., Simões, M. R., Pereira, M., Gameiro, S., Quartilho, M. J., Paredes, T. (2006). Estudos psicométricos do instrumento de avaliação da qualidade de vida da Organização Mundial de Saúde (WHOQOLBref) para Português de Portugal. Psiquiatria Clínica, 27, 4149. [ Links ]
Verberg, M. F., Eijkemans, M. J., Heijnen, E. M., Breoekmans, F. J., De Klerk, C., Fauser, B. C., & Macklon, N. S. (2008). Why do couples dropout from IVF treatment? A prospective cohort study. Human Reproduction, 23, 20502055. doi: 10.1093/humrep/den219
Verhaak, C. M., Smeenk, J. M., Evers, A. W., Kremer, J. A., Kraaimaat, F. W., & Braat, D. D. (2007). Women’s emotional adjustment to IVF: A systematic review of 25 years of research. Human Reproduction Update, 13, 2736. doi: 10.1093/humupd/dml040
Volgsten, H., Skoog Svanberg, A., Ekselius, L., Lundkvist, O., & Poromaa, S. (2008). Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Human Reproduction, 23. 20562063. doi: 10.1093/humrep/den154
Wang, K., Li, J., Zhang, J. X., Zhang, L., Yu, J., & Jiang, P. (2007). Psychological characteristics and marital quality of infertile women registered for in vitro fertilization and intracytoplasmic sperm injection in China. Fertility and Sterility, 87, 792798. doi: 10.1016/j.fertnstert.2006.07.1534
Watkins, K. J., & Baldo, T. D. (2004). The infertility experience: Biopsychosocial effects and suggestions for counselors. Journal of Counseling and Development, 82, 394402.
WHOQoLGROUP. (1995). The World Health Organization Quality of Life Assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41, 14031409.
Wischmann, T., Scherg, H., Strowitzki, T., & Verres, R. (2009). Psychosocial characteristics of women and men attending infertility counselling. Human Reproduction, 24, 378385. doi: 10.1093/humrep/den401
Yong, P., Martin, C., & Thong, J. (2000). A comparison of psychological functioning in women at different stages of in vitro fertilization treatment using the mean affect adjective check list. Journal of Assisted Reproduction and Genetics, 17, 553556.
Zegers-Hochschild, F., Adamson, G. D., de Mouzon, J., Ishihara, O., Mansour, R., Nygren, K., van der Poel, S. (2009). The international committee for monitoring assisted reproductive technology (ICMART) and the World Health Organization (WHO) revised glossary on ART terminology. Human Reproduction, 24, 15. doi: 10.1093/humrep/dep343
Este trabalho recebeu apoio da Fundação para a Ciência e Tecnologia (FCTSFRH/BD/23152/2005, SFRH/BPD/63063/2009, FEDER/POCTI–SFA–160–192).
Recebido em 30 de Maio de 2009/ Aceite em 1 de Novembro de 2010













