Since the beginning of the COVID-19 pandemic, there have been over 60 million positive cases and 1,4 million deaths worldwide attributed to this disease. Europe alone has had more than 18 million COVID-19 patients with more than 400.000 deaths (Our world in data, 2020). It has dramatically changed the way we live, work, and connect with other people. It has also had a profound impact on the emotional and physical support given to hospitalized patients and their families, who not only have to face the uncertainty of a “not-so-well-known” disease, but also the impossibility to care for and to be with their loved ones in such a challenging period of their lives.
In the past months, a multiplicity of testimonies has surfaced from healthcare workers (HCW), as well as from patients and family members, about the isolation and feelings of loneliness and abandonment of hospitalized COVID-19 patients. Dying in solitude and the impediments to saying goodbye have been pointed out by doctors and families as having a devastating impact on everyone involved (Bangkok Post, 2020; Channel News Asia, 2020; Harroon & March, 2020; Hornig & Stöhr, 2020; Lamas, 2020; Ramsey, 2020; The Jakarta Post, 2020).
Hospitalized patients are submitted to a multitude of acute and recurrent stressors. The need for hospitalization is a stressor by itself, due to the anxiety associated with the uncertainty of the prognosis as well as the separation from their loved ones and consequential loss of psychosocial support (Berwick & Kotagal, 2004; Guo et al., 2017; Williams, 2005). A negative emotional state, such as stress or anxiety, has been shown to influence the neuroendocrine, inflammatory, and hormonal responses, with repercussions in morbidity, mortality, and recovery time of patients admitted to Intensive Care Units (ICUs) (Papathanassoglou, 2010). However, the need for hospitalization does not just affect patients, as it can also trigger feelings of fear, anxiety, and psychological suffering in their loved ones, due to the requirements of providing emotional support to the patient while facing the reality of the situation and the possibility of loss (Williams, 2005). Furthermore, multiple studies have demonstrated that inpatient visits from loved ones reduce emotional stress while bringing about beneficial cardiovascular and hemodynamic effects (Bay et al., 1988; Griffin, 2003; Hepworth et al., 1994; Institute of Medicine (US), 2001; Kleman et al., 1993; Krapohl, 1995; Lazure, 1997; Medves et al., 2009; Morgan et al., 2005; Ramsey et al., 1999; Roland et al., 2001; Simpson & Shaver, 1990; Williams, 2005).
As the world is dealing with a new, unknown disease that requires total isolation of the infected patients, with possible fatal complications, hospitalization itself takes an even heavier toll on everyone involved. In 2003, amidst the SARS epidemic, Singapore and Hong Kong successfully implemented a communication system to bypass the need for in-person interaction through telephone and video calls, which positively impacted the physical and emotional well-being of the people involved (Gomersall, et al., 2006). Although scarce, the existing literature on the use of phone and video calls between patients and their loved ones suggests that these alternative communication methods carry several benefits. Telephone calls allow individuals to hear each other’s spoken words, vocalics, and paralanguage (non-verbal components, such as prosody, pitch, volume, or intonation) while video calls additionally allow for the visual perception of the other and their surrounding environment, as well as the interlocutor’s non-verbal language (Hensel et al., 2007). The adjoining visual non-verbal cues enhance the sense of social presence and communication of affective information (Brecher, 2013; Hensel et al., 2007; Short et al., 1976). As such, several case reports carried out in palliative care units and residential care facilities showed a reduction in social isolation and an improvement in general well-being in both patients and their families (Brecher, 2013; Hensel et al., 2007; Sävenstedt et al., 2003; Guo et al.,2017; Parsapour et al., 2011). In these articles, the authors also reported that video calls contributed to a sense of emotional and spiritual relief in the patient’s family and a sense of closure, promoting healthy mourning when that was the case. Furthermore, video calls require readily accessible and relatively inexpensive equipment, with little risk for their users, making it a suitable replacement for situations where inpatient visits are not allowed.
In recent months, multiple institutions have adapted in order to allow patients with COVID-19, and other diseases, to maintain some sort of contact with their loved ones, namely through video calls. In the United Kingdom, at the Royal Hospital for Neuro-disability (2020) the “Staying Connected” system was implemented to allow video communication between patients and family members using iPads and Android tablets (Royal Hospital for Neuro-disability, 2020); at the Royal Melbourne Hospital, in Australia, a videoconference model was installed at the ICUs (The Royal Melbourne Hospital, 2020); and the New-York Presbyterian Hospital, in the USA, encouraged patients and families to keep in touch using Skype or FaceTime (New-York Presbyterian, 2020).
The first COVID-19 case in Portugal was diagnosed on 2 March 2020 (Público, 2020). The country then experienced a controlled but steady rise of COVID-19 cases, including those in need of hospital care. Restrictions regarding daily activities and social contact began soon after, as well as restrictions of inpatient visits. Our hospital, São Francisco Xavier, located in Lisbon, recognized the need to overcome the communication barrier generated by COVID-19 and, in mid-April, the COVID-19 designated units were equipped with smartphones and tablets donated by a Portuguese technology company.
The present report aims at describing the different practices in using video calls to bring COVID-19 patients and their families closer. The authors also reflect on the benefits and pitfalls of this new communication method on hospitalized patients’ psychosocial support.
Methods
Participants
A convenience sample was used, consisting of four HCW responsible for managing the use of the videophones and tablets in each of the four COVID-19 wards.
Materials
The authors developed a semi-structured interview based on the available literature on technologically-based interpersonal communication for hospitalized patients (Brecher, 2013; Guo et al.,2017; Hensel, 2007). The interview consisted of broad, open-ended questions interspersed with more specific questions regarding the HCW general impression on video communication used in the wards and evaluation of perceived utility, barriers, benefits, or detriments inherent to the use of this technology in the COVID-19 units.
Procedure
Participants were recruited by email invitation. The interview took place via phone call, in June 2020, two months after the implementation of the communication devices. Responses were transcribed and analyzed by the authors, which inductively grouped the answers into themes or categories and evaluated similarities and differences between responses. In the final analysis, the data was comprised of the following: (1) description of the unit: severity of COVID-19 cases, total capacity and number of admissions; (2) generic patient data: gender distribution, age (mean), average length of stay and deaths; (3) description of video call communications: frequency, duration, access to personal means of communication, and the existence of communication protocols; and (3) perceptions of videophone communication use: advantages, pitfalls, feedback from patients and their families, and feedback from HCW.
Results
COVID-19 designated units
During April and May, São Francisco Xavier hospital had four COVID-19 designated units: three internal medicine wards, for mild and moderate COVID-19 patients, and one ICU (Unidade de Cuidados Intensivos Polivalente), for severe and in need of organ support patients.
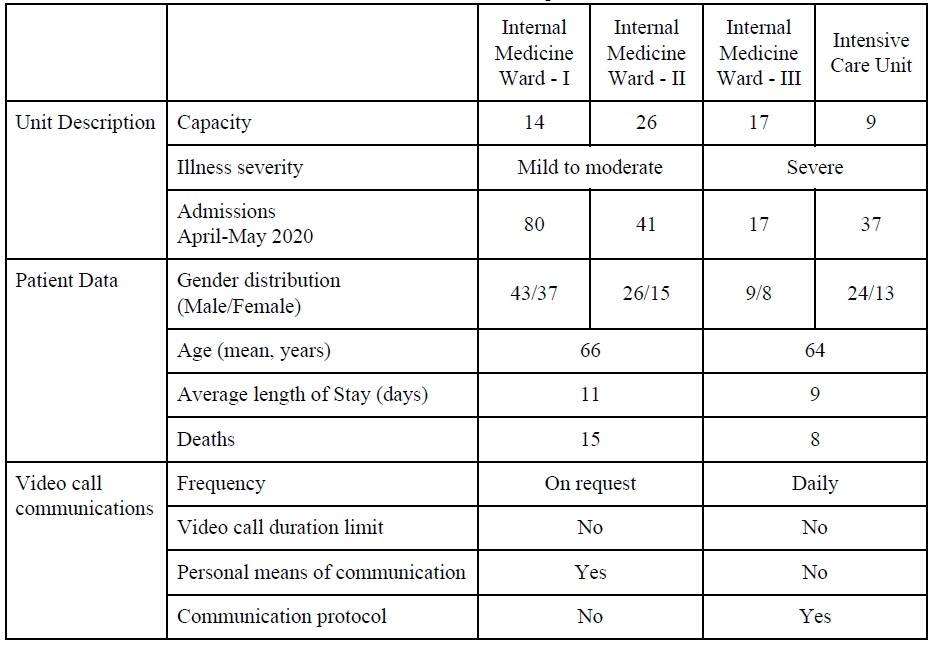
The three internal medicine wards prepared to treat COVID-19 patients have a full capacity of 57 patients (14, 26, and 17, respectively). During April and May, a total of 138 patients were admitted (80+41+17), with an average length of stay of 8,18 days, and a total death toll of 11 patients.
The ICU has a total capacity for 9 patients and admitted a total of 37 patients between April and May, with an average length of stay of 9 days. During that time, 8 patients passed away (Table 1).
HCW
Each ward has a designated HCW to manage video call equipment and communications, who were recruited by the authors All HCW are doctors, three women and one man, aged late 30s to 50, all Internal Medicine specialists, in a high hierarchical position in each ward with several management responsibilities.
Video call communication
All units were equipped with a smartphone and a tablet, and these devices were used for video calls between inpatients and their families, with no time restriction. Clinical information was provided daily to families via phone call.
COVID-19 Internal Medicine Wards
Two internal medicine wards received mostly younger patients that used their own means of communication and therefore did not benefit from hospital devices. In these wards, some older and/or more dependent patients were offered the possibility of connecting with their loved ones through video calls using the hospital devices. These devices were managed by the hospital staff, who established the connection and then allowed the patients to communicate with their families, alone or under supervision, depending on each patient’s autonomy. However, since there was no communication protocol in place, patients were often unaware of the availability of such devices. Family members who asked about alternative means of communication with their loved ones would eventually be told about the video call facility. There were a few cases of patients who died before being able to communicate with their families.
The third internal medicine ward admitted mostly older patients. Although they could benefit from video call devices, some barriers compromised their routine use, such as technological difficulties (lack of SIM cards and Skype accounts), as well as user-related difficulties (patients with advanced dementia, hearing loss, or loved ones who were not comfortable with technology). It was the imminent death of a patient that unlocked the use of the video call devices in this ward: as an elderly patient’s health state deteriorated, her son asked if the family could see her and say goodbye. In view of this request, efforts were made to get a device for the unit. The patient’s son and granddaughters were able to see and speak to her through a video call, despite the patient no longer being responsive. She died a few hours later, and her son later thanked the HCW, underlining the importance of this last goodbye. After this episode, HCW started using these devices at least once a week per patient, acknowledging the importance of these contacts, which they described as “beautiful and happy moments”, and allowed for the “humanization of care”.
All the HCW reported that video calls made from the hospital’s gadgets were not widely used, pointing to the absence of a structured protocol for making these contacts as the main reason for the lack of routine use. Other possible causes preventing a wider use of the devices included work overload, time limitations, lack of communication and coordination between professionals, and lack of awareness for the importance of this initiative, seen by some HCW as a “waste of time”.
COVID-19 Intensive care unit
In the ICU, a communication protocol was implemented: the same designated doctor provided the patient’s clinical information to a designated family member, every morning, via phone call. This intended to reduce miscommunication between the family and the clinical team. The nursing team was briefed on the information provided to the family members, and every afternoon, according to previously scheduled slots, they established the video calls between patients and their families. Due to the patients’ greater need for assistance, almost all contacts were supervised, and the video calls had no time limit. Family members could also request video calls or extra clinical information by contacting the ICU secretary, who would contact the doctor responsible for the communication protocol to make the necessary arrangements. A protocol with the hospitals’ Mental Health Crisis Management Team was implemented, in order to provide psychiatric/psychological support to distressed COVID-19 patients or family members. This resource was used two times, during April and May.
The ICU HCW reported that, although some family members had trouble seeing their loved ones in an ICU context, the video calls also contributed to the families’ better understanding of the disease and its severity. All families gave positive feedback about the use of tablets and smartphones in the ICU, pointing out that, for several of them, it was the only moment they were able to see their loved ones since they had been hospitalized. One of the families that praised this initiative had every member infected and apart (the husband was in the ICU, the wife was home alone, and her 80-year-old mother was also alone, in a different city). The patient’s wife reported that she felt very lonely and worried about her family, and being able to see her husband every day was very important for her mental health and well-being and to get her through a “really hard time”.
The interviewed HCW identified these factors as the main reason for the early engagement of HCW and families and the intervention’s success. They reported that the staff felt “joy in being involved in this alternative way of caring for the patients”.
Discussion
The mandatory isolation of COVID-19 hospitalized patients from their loved ones, urged the implementation of alternative means of communication to bypass inpatient visits and minimize its impact on the physical and emotional well-being of the people involved.
In the present study, we found a generalized acknowledgment of the importance of offering video calls in the COVID-19 units, namely its positive emotional impact on patients, family members, and HCW involved. However, there were some major differences in the way these were implemented, which ultimately impacted each ward’s overall experience, namely: the existence of a communication protocol and the staff’s awareness and engagement with the initiative.
Amongst the internal medicine wards, it was highlighted that several factors led to the scarce use of the hospital devices, such as work overload, time limitation, lack of communication and coordination between staff members, hardware and software difficulties, patient limitations, and also lack of importance given to this initiative by some HCW. Although technology-related difficulties and patients’ impairments were also reported in the ICU, none of these factors were recognized as barriers to the use of video call devices. Although we acknowledge that the work overload and time limitation reported by the internal medicine HCW had its influence on the use of the communication devices, we believe the absence of a structured protocol for offering the video calls led to uncertainty as to whom was responsible for the contacts which, consequently, were made haphazardly. Further contributing factors were the staff’s lack of awareness of the video calls’ importance, and their disposition and ability to resolve technological obstacles or reorganize their work schedule to accommodate this extra task.
Based on the testimonies given by the different HCW, we believe that the implementation of a structured and straightforward protocol is essential to guarantee a regular and optimized use of the communication devices. Looking at the ICU’s positive example, we recommend that every communication protocol must comprise: a HCW designated as supervisor; the early identification of patients that rely on hospital devices for communicating with their families; a defined circuit of communication (i.e., families must be informed of the patient's clinical status before the video call and preferably always by the same HCW); a well-defined frequency of communication and scheduled periods for that purpose; assigned HCW responsible for establishing the video calls; the registration of contacts made; and rules for its usage (e.g., keeping the mask on while making video calls in the ward).
Furthermore, we propose increased dissemination of information about the positive impact of communication between inpatients and their families. Although it is easy to neglect this at a time of crisis and work overload, the humanization of care and the continued presence of emotional support are vital for the well-being of patients, families, and HCW. As it was stated, in the wards where the video call system was used routinely, the HCW did not see it as another extra task but rather as delivering proper care to their patients.
Video calls require accessible and inexpensive equipment, with little risk for users. Further studies in internet-based communications for hospitalized patients should focus on adding quantitative data to illustrate benefits and define an adequate design for the intervention, namely the contacts’ optimal frequency and duration. This would lead to the development of widespread protocols and standardized interventions. This is especially relevant given that we are still facing the COVID-19 pandemic, might face others in the future (Ross et al., 2015), and it would be beneficial to have well-defined protocols for communication put in place in time. This would facilitate the implementation of such protocols and their seamless integration in healthcare services. Lastly, in our view, this technology’s use entails broad advantages for COVID-19 patients and other medical situations where inpatients have no visits or regular contacts with their loved ones.