Cancer patients experience many emotional, social, cognitive, and physiological challenges that consequently tend to influence their quality of life (QoL) (e.g., Perry et al., 2007). In addition to these, in cases of breast cancer (BC), the individuals are especially susceptible to experiencing concerns and changes in their body image, femininity, and sexual functioning (e.g., Pritchard, 2007).
Chemotherapy (CT) is one of the main treatments used for BC and it can be adjuvant, when it is administered after surgery and/or radiotherapy; or, neoadjuvant or primary, when it is used as first-line therapy, before surgery (Beaver et al., 2016; Lennan, 2011). Some authors have pointed out that it is mainly CT that causes symptoms that negatively affect QoL (e.g., Lee et al., 2001), with significant impacts in the physical, cognitive, and social functioning (Cheng et al., 2013). Lee et al. (2001) listed the factors that influence the well-being and the QoL of BC patients receiving CT: individual’s characteristics; disease’s characteristics; psychological factors, such as the development of anxiety and/or depression; and, social support, that includes the relatives' support and the emotional and informational support from health professionals.
In this regard, it is possible to understand how CT can influence the psychological state of women with BC. As such, to contribute to more scientific knowledge about the psychological impact of CT and of other factors in women with BC during neoadjuvant CT, this present study has as main objective to comprehend which factors contribute to their psychological state, in these women’s perception, during or shortly after the submission to CT. For that, this project is a cross-sectional study, based on a qualitative approach with a descriptive and exploratory nature.
Method
Participants
A non-probabilistic sample of 25 women with BC who had been or were being submitted to neoadjuvant CT at the Centro de Mama of Centro Hospitalar Universitário de São João (CHUSJ; Oporto, Portugal) was studied. The inclusion criteria for participating in the study were: (a) to be 18 years old or older; (b) to be a female; (c) to have primary BC; (d) to have been or being submitted to neoadjuvant CT; (e) absence of recurrence or metastasis; (f) absence of major psychiatric disorders; (g) to be able to speak, read and comprehend Portuguese.
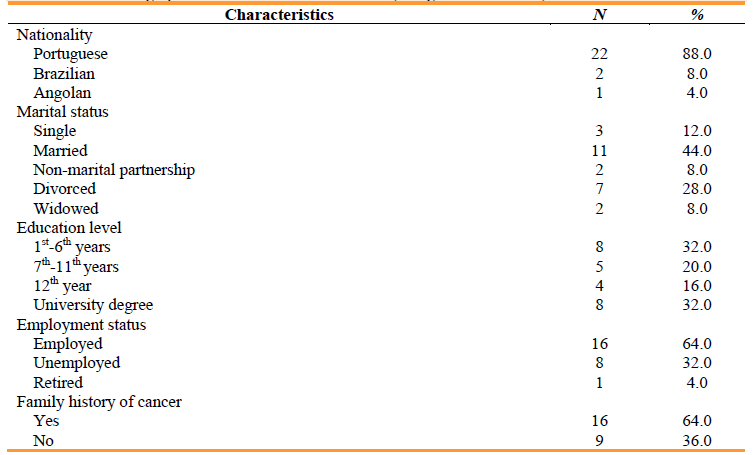
The demographic and clinical characteristics of the sample, regarding categorical variables, can be found in Table 1. The sample mainly comprises Portuguese women, but also two Brazilian women and one Angolan woman. The majority is married (n = 11), employed (n = 16) and has a family history of cancer (n = 16). In terms of education level, most women have primary school (n = 8) or a university degree (n = 8).
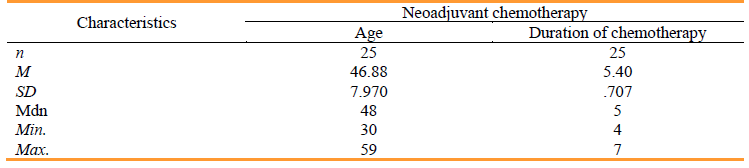
Regarding the continuous variables of sociodemographic and clinical characteristics, they can be found in Table 2. In terms of age, the mean was of 46.88 years, and, regarding the duration of CT, the mean was of 5.40 months.
Measures
In this study, it was administered a sociodemographic and clinical questionnaire that was purposely created to collect sociodemographic and clinical information about the participants. As such, it was collected sociodemographic data about age, nationality, marital status, educational level, and employment status of the women. Regarding clinical data, it was collected information about the diagnosis date, duration of CT up to the time of the interview, and family history of cancer. In addition, it was formulated a question to inquire women about at least three factors (if possible) to which they attributed their psychological state to.
Procedure
Initially, it was requested approval for the project from the Ethics Committee of CHUSJ, which was given. Then, through the Centro de Mama’s psychologist, it was initiated contact with the patients. Patients were invited to participate when they went to the service for formerly scheduled appointments, treatments, or exams, to ensure it was not necessary any special travel. When women accepted to participate in the study, then it was requested a written informed consent. Afterwards, the interviews were conducted, and the sociodemographic and clinical questionnaire was completed. Data was collected from January to June 2021. After the collection of data, statistical treatment was performed using the Statistical Package for Social Sciences (SPSS Inc), version 27.0.1, in which data was subjected to descriptive analysis.
Results
Regarding the question about at least three factors that women attributed their psychological state to, 20 women out of the total sample responded to it. Since the responses to this question were very diverse, it was used the Grounded Analysis. As such, based on the similarities among the responses, they were grouped into larger clusters.
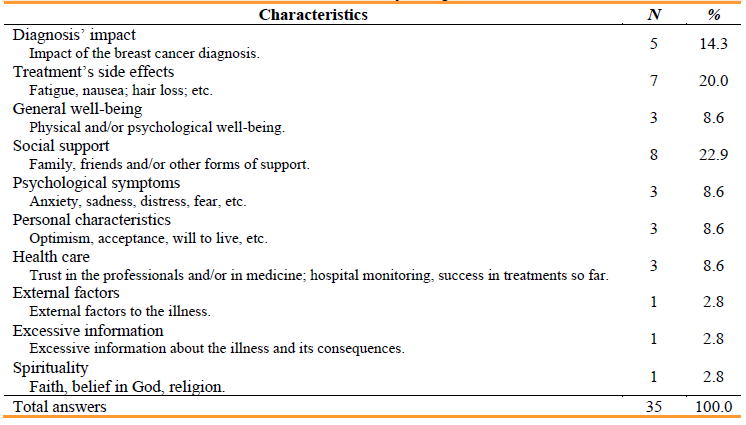
This analysis resulted in the identification of 10 categories that are presented in Table 3. In addition, Table 3 also presents examples of the responses that make up each category, and the respective frequencies by category.
As shown in Table 3, 35 responses were obtained in total, since each woman was asked to answer three factors if possible. Women mentioned more frequently “social support” (n = 8), followed by “treatment’s side effects” (n = 7) and “diagnosis’ impact” (n = 5). Other factors mentioned by several women were “general well-being” (n = 3), “psychological symptoms” (n = 3), “personal characteristics” (n = 3) and “health care” (n = 3). Three factors, namely “external factors”, “excessive information” and “spirituality”, were only mentioned once each.
Discussion
This study aimed to analyse the factors that women with BC who had been or were being submitted to neoadjuvant CT consider that contribute to their psychological state. The results showed that women attributed their current good psychological state to different factors, but the social support they received, the diagnosis’ impact and the treatments’ side effects were the three factors most mentioned. Focusing firstly on the more positive factors, these outcomes are consistent to what was found in literature, with many authors also referring the importance that social support has to women with BC, especially the family’s support (e.g., Carvalho et al., 2016; Cheng et al., 2013). In terms of personal characteristics, there were obtained answers such as “optimism”, “acceptance” and “will to live”, which seems similarly go along with some of the reports of BC women found in other works. Carvalho et al. (2016) describes “strength” and “will to live” as standpoints frequently mentioned by women; and Rodrigues and Polidori (2012) pointed out the reference to optimism, trust, courage and resilience as essential topics for these women.
Although some answers were given about spirituality, this is not in line with the literature, as spirituality is seen as a very important factor for women that provides them with hope, strength, and balance in the face of illness (e.g., Carvalho et al., 2016; Mattias et al., 2018), so it was expected that more women would name spirituality. Now, this may also depend on how patients interpreted the questions and whether they looked for more immediate and objective factors, having left spirituality somewhat aside as it is more subjective. These results can be important to psychologists since, in this study and in literature, social support, resilience, coping, and spirituality seem to have a positive impact on the psychological state of women with BC; as such, psychologists should invest in the development and in the administration of interventions that aim these dimensions to improve them and, consequently, promote a better well-being and QoL in this population.
In terms of health care, women in this study revealed that their trust in medicine and in the health professionals, and the hospital monitoring were factors that contributed positively to their psychological state. These results support the findings of Carvalho et al. (2016) and Cunha et al. (2017), which refer that the healthcare team often constitutes another form of support for women with BC. Finally, three women also referred general well-being, because they mentioned feeling good either physically and/or psychologically. In literature, although there are many studies in which women presented low levels of physical and/or psychological well-being, there are other studies, in which women showed good levels in these dimensions (e.g., Cheng et al., 2013).
Now, focusing on the less positive factors listed, a frequent answer given by the participants was the diagnosis’ impact. Many authors discuss the effect of a diagnosis of BC on women, namely they refer that the moment women know of the diagnosis they have an immediate fear of possible death and that marks the initial milestone of the psychological problems that may accompany women during cancer (Carvalho et al., 2016; Mattias et al., 2018). One question that can be raised is whether certain factors can have a greater impact at a given stage and then, over time, other factors take on a greater impact, since only some women mentioned the diagnosis’ impact. As such, it is possible that women that did not mention it were further along the cancer path, and maybe the BC diagnosis did have a major impact on their psychological state at an initial stage, but then as they progressed through the cancer course, other factors took on a greater impact. Consequently, this can be a clue for the multidisciplinary health team to act according to the needs felt at each moment of the BC’s trajectory, for example, with greater emphasis on the impact of the diagnosis at the beginning, but also never neglecting the personal needs of each woman.
Treatments’ side effects, particularly CT’s side effects, are often mentioned in literature as having a major psychological impact (e.g., Cunha et al., 2017; Rodrigues & Polidori, 2012), which supports the findings in this study. Psychological symptoms were also mentioned by women in this study, with the mention of fear, anxiety, and sadness, which is in line with the findings of other works that refer that women frequently feel these emotions during the course of cancer (e.g., Carvalho et al., 2016). Lastly, in terms of the answers given about the women’s psychological state, it seems important to highlight that one woman, namely a health professional, answered that she had excessive information about cancer. Normally, women want to know more information about cancer and treatments; however, some did not want full information about it because they considered that that would bring them more fear and anxiety (Beaver et al., 2016). Perhaps other participants also had access to excessive information, due to the easy and sometimes unreliable access to the internet, and, as such, this is a possible topic to be addressed directly by the health team with patients, in order to find out if they have read something about the disease on the internet, what they thought of what they read, if they have doubts, if something has upset them and if they want clarification.
Finalising, this present study has as main conclusions that women with BC submitted to neoadjuvant CT attribute their psychological state to diverse factors and that social support, spirituality, health care and other factors contribute positively to it, while other factors contribute negatively, such as the diagnosis and the side effects women experience. Regarding limitations of the study: it has a cross-sectional study design; it has a small sample size which may affect the reliability of the results; and it is based on a qualitative method that sometimes can be subjective and that can make the data’s interpretation more difficult. For future reviews, it is suggested the use of a bigger sample size and a quantitative assessment that complements the qualitative one to allow a more precise analysis of the results.
The main messages for the multidisciplinary health teams that this study provides are: that there must continue to exist investments in health care, since some women mentioned its importance; that joint and multidisciplinary work is important, namely inclusion and referral to mental health professionals for the enhancement of certain traits and dimensions, such as resilience, optimism, and social support, given the good effect they have psychologically on women; that online health literacy issues should also be addressed since they may have a negative impact on women with BC due to access to wrong information; and, given that it was raised the hypothesis that women’s needs may change during the cancer’s course, it is suggested that more assessments are done to try and perceive the needs moment by moment and then meet them.
The main message for psychologists is that there should continue to exist an investment in the development and administration of psychological interventions to improve the social support, coping, resilience, spiritual well-being and other dimensions, since they seem to be good contributors to these women’s psychological state. Finally, future studies should be carried out to improve knowledge about the experiences of women with BC during the different treatments they have to endure, and in Portugal since few studies were found, so that the patients’ needs can be met.
Author’s contribution
Ana Santos: Concetualização; Curadoria dos dados; Análise formal; Investigação; Metodologia; Administração do projeto; Visualização; Recursos; Redação do rascunho original; Redação - revisão e edição.
Isabel Silva: Concetualização, Análise formal, Metodologia, Administração do projeto, Validação, Visualização; Recursos; Supervisão, Redação - revisão e edição.
Raquel Guimarães: Concetualização, Metodologia, Administração do projeto; Supervisão
Rute Meneses: Concetualização, Metodologia