In Portugal, it is estimated that in 2020 appeared approximately 7 000 new cases of breast cancer in women (European Commission, 2020). Breast cancer (BC) causes diverse psychological consequences associated with the fear of breast’s amputation (partial or total), which is a body part largely linked to the notions of sensuality, sexuality, and maternity (Silva, 2008). Furthermore, women also suffer changes in their social relationships, positive affect (PA), negative affect (NA) and spirituality (Paris et al., 2014). Therefore, comprehensive oncology care concerns all these aspects, valuing the importance of psychological interventions that meet the needs of the patients according to the different phases of illness and treatments (Strada & Sourkes, 2015).
This systematic review aims to synthesize the current knowledge about psychological interventions developed with women with BC, preferably during chemotherapy, and that were directed to these psychosocial dimensions, such as quality of life (QoL), resilient coping, social support, PA, NA, and spirituality.
Method
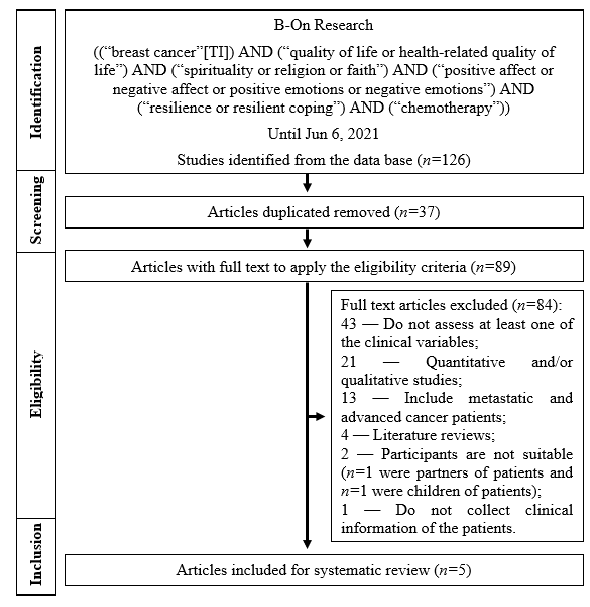
The present systematic review complies with the guidelines recommended in the guide Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Liberati, 2009). The following research question was created: What do we know about psychological interventions that aim the QoL, social support, spirituality, PA, NA, and/or resilient coping of women with BC? Firstly, eligibility inclusion criteria defined were the following: full-text publications in Portuguese, English or Spanish of the last 10 years; studies that assessed at least one of the variables of interest; and studies in which the participants were women aged 18 years or more and that had a diagnosis of BC. The procedure for the research in the database Biblioteca do Conhecimento Online (B-On) is presented in Figure 1. From this research resulted 126 studies and after the phases of study selection only five studies were included for final review.
Results
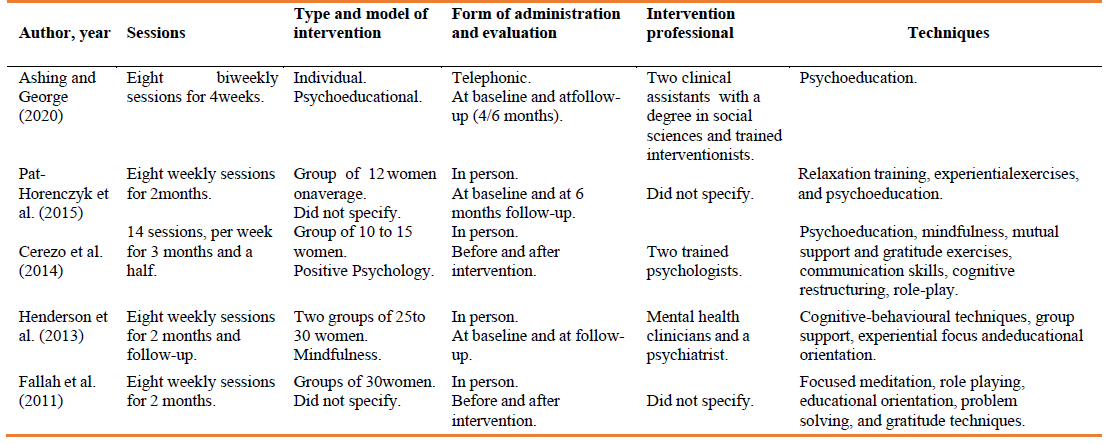
A summary of the interventional articles from this literature review can be found in Table 1. In Table 2 is presented a summary of the interventions mentioned in the studies.
By analysing Table 1, it can be verified that all studies were experimental and had as main objective to evaluate the efficacy of a particular intervention in women with BC. In terms of sample, the participants were always women with BC. Regarding the main focus of the studies, Henderson and colleagues (2013) and of Fallah et al. (2011) tested the effectiveness of an intervention on spirituality, through a Mindfulness-Based Stress Reduction (MBSR) programme and a psycho-spiritual group intervention, respectively. Both studies documented an improvement on spirituality from pre-intervention to post- intervention: in the Henderson and colleagues’ study (2013) improvement was more significant in the intervention group, than in the control group and in the Fallah and colleagues’ study (2011) improvement was only verified in the intervention group, since the control group showed a reduction in spirituality.
Affect was assessed in women with BC after two interventions, namely: a telephonic psychoeducational intervention trial (Ashing & George, 2020); and a positive psychology-based group intervention (Cerezo et al., 2014). On both studies, women showed improvements in terms of affect: the first verified that the change in emotional well-being was statically significant, with the emotions related to sadness, coping and nervousness having significant improvements and the changes in NA were more significant in the intervention group than in the control group (35% of the participants showed an increase in NA); and the other showed higher scores on PA and total affect and lowest scores on NA from pre-test to post-test, more significant in the intervention group than in the waitlist group.
Table 1 Summary of the Interventional Studies
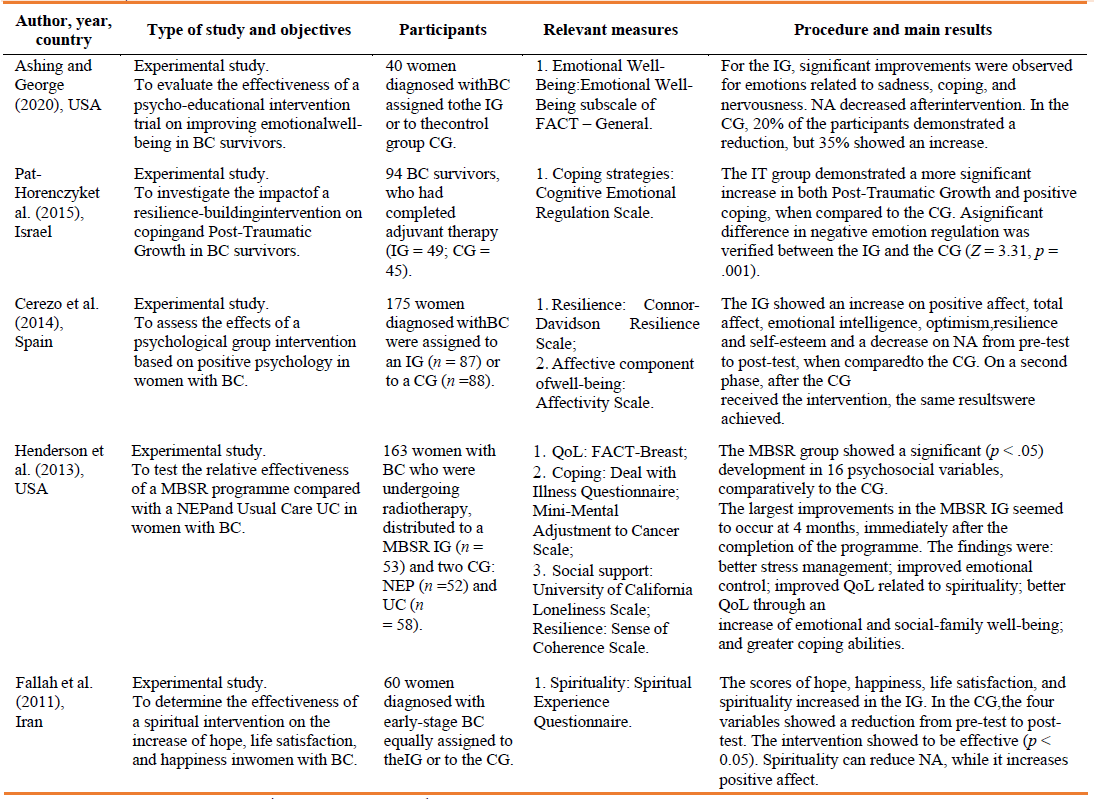
Note: BC = Breast Cancer; IG = Intervention Group; CG = Control Group; FACT = Functional Assessment of Cancer Therapy; NA = Negative affect; MBSR = Mindfulness-Based Stress Reduction; NEP = Nutrition Education Programme; UC = Usual Care; QoL = Quality of life.
Cerezo et al. (2014) and Henderson et al. (2013) applied a positive psychology- based group intervention and a MBSR programme, respectively. Both studies showed an improvement on resilience more significant in the intervention group than in the groups that did not receive the intervention. Coping was assessed by Henderson et al. (2013) and Pat-Horenczyk et al. (2015), that evaluated the effectiveness of a MBSR group programme and of a resilience-building group intervention, respectively. Active cognitive coping and active behavioural coping showed more significant improvements in the intervention group than in the other two control groups (Henderson et al., 2013) and 75% of the women of the intervention group reported an increase in positive coping and/or a decrease in negative coping after intervention, while in the control group only 29.2% of the women showed developments (Pat-Horenczyk et al., 2015).
Social support and QoL were assessed in the same study (Henderson et al., 2013). It was verified an improvement on QoL related to spirituality and to emotional and social- family well-being in the intervention group, higher than in the other groups (Henderson et al., 2013). However, regarding social support, although the study mentions it in the measures’ section and refers using the Revised University of California Loneliness Scale, there were not presented any results regarding it.
Discussion
A systematic review of the literature was carried out to synthetize the current knowledge about psychological interventions administered to women with BC and that assessed the evolution of their QoL, social support, spirituality, PA, NA, and coping resilient. Five studies that evaluate the efficacy of different interventions were found, specifically interventions based on mindfulness, on psychoeducation, on psycho- spirituality, on positive psychology, and on existential psychology. However, they have different numbers of sessions, have different durations, have different types of intervention and forms of administration, are managed by different professionals, and address different topics. Additionally, in some of the studies (i.e., Fallah et al., 2011; Pat- Horenczyk et al., 2015) there was some information that was not specified. Therefore, the conclusions reached may be also influenced by all these factors mentioned, which can make the comparison between interventions’ efficacy and results difficult.
All five studies demonstrated positive results, despite the target dimension or the intervention model. Although some interventions are focused on teaching or enhancing some characteristics, they have also seen improvements in other areas, because of the correlations among the variables. Some examples are a spiritual intervention showing improvements in NA and in PA (Fallah et al., 2011); and, a resilience-building intervention having a positive effect in coping, in the PA and in the NA of women with BC (Pat-Horenczyk et al., 2015).
This literature review allows us to conclude that: psychological interventions targeting these psychosocial aspects have been developed and administered in this population; psychological interventions that aim to improve certain psychological dimensions (e.g., spiritual well-being, coping, etc.) can also enhance wider dimensions (e.g., quality of life, well-being, etc.); and that most of these interventions achieved good results in improving these dimensions. These conclusions are important for health care, since several of these dimensions will influence the psychological adjustment to the disease (Stanton et al., 2001) and should be valued by health professionals in order to promote the best possible adjustment.
Regarding this review’s limitations, the following are important to mention: an excessive number of descriptors were defined which may have led to the exclusion of relevant studies that could be about psychological interventions administered to women with BC; it was only used one database (B-On); and the variety of the variables assessed, of the intervention-model, of the techniques used and of the psychometric instruments applied can make the analysis of these results complicated and does not allow generalisations. Furthermore, some of the studies did not specify information, which would allow more clarity about the interventions and their results. Also, some studies do not mention who the interventionists are, which could be important to know, to possibly compare with other interventions, since who delivers the intervention may influence its results. It is suggested for future reviews the inclusion of less psychosocial dimensions, to have a larger number of interventional studies, which could allow more generalisations. Further deepening of knowledge about psychological interventions aimed at women with BC seems crucial, to understand whether these produce good results and whether they help meeting these women’s needs and to provide more hints about what health professionals, namely psychologists, could do different to achieve even better outcomes, namely better QoL and well-being.
Author’s contribution
Ana Santos: Conceptualization; Formal Analysis; Investigation; Methodology; Project Administration; Visualization; Resources; Writing - Original draft; Writing - Revision and edition.
Isabel Silva: Conceptualization; Formal Analysis; Methodology; Project Administration; Validation; Visualization; Resources; Supervision; Writing - Revision and edition.