Introduction
Dens invaginatus may be defined as a dental anomaly that most probably occurs during the tooth development phase, resulting in an invagination of the dental papilla previous to the complete tooth calcification.1 Other different terms have been suggested to describe this phenomenon, such as dens in dente; dentoid in dente; dilated composite odontoma; dilated gestant odontoma; invaginated odontoma; or tooth inclusion.1 These different nomenclatures might be associated with the lack of consensus regarding the etiology of this malformation.2 Moreover, numerous theories have been proposed to explain the dens invaginatus condition and, although environmental and genetic factors appear to be both involved, the definitive cause is still not fully understood.3-5
Different classifications involving different benchmarks have been suggested for this condition. The most used was introduced by Oehler in 19576 and divides this condition into three categories (types) according to its extension and possible communication with periodontal tissues, based on radiographs.
Type I is defined as a partial invagination that extends only into the crown. Type II represents a partial invagination that extends inside the root, with or without pulp communication, but without direct contact with the periodontal ligament. Type III consists of a complete invagination that may communicate laterally (type IIIa) or apically (type IIIb) with the periodontal ligament, creating a pseudo- foramen. Generally, there is no communication with the pulp in these cases.6
According to twenty studies from 1873 to 20077 reporting dens invaginatus prevalence on permanent teeth, this condition’s prevalence may range from 0.3% to 10.0% of the population.7 This wide variation may be a consequence of different study designs or diagnostic criteria.1,7,8 The most affected teeth are maxillary lateral incisors, followed by maxillary central incisors, canines, and, less frequently, posterior teeth.1,3 In rare cases, mandibular teeth may also be affected, as well as primary teeth or supernumerary teeth.1,3 Double and triple invaginations have also been reported.1,3
The dens invaginatus malformation may go unnoticed due to the absence of significant clinical signs or symptoms. Most cases are radiographic findings whose appearance depends on their extension.1,4,7-9 Clinically, aberrant crown morphology and a deep foramen can be found.10The undiagnosed invaginations may work as a possible pathway for microorganisms to enter the pulp and periodontal tissues. Moreover, these teeth are more prone to develop caries and peri-radicular lesions.1,3,9
The complex internal anatomy of the dens invaginatus type IIIb makes its normal endodontic treatment modality harder and more delicate. The treatment procedures depend on the type of dens invaginatus and pulp diagnosis.4,5,10The present case report aims to document the nonsurgical endodontic treatment of a mandibular canine presenting with dens invaginatus type IIIb with healthy pulp and an acute apical abscess.
Case report
A 12-year-old male patient was referred for an endodontic appointment with spontaneous pain and an acute abscess with swelling of the tissues associated with tooth 33 (left mandibular canine). The intraoral observation confirmed the presence of an acute periapical abscess adjacent to the canine, which was tender to percussion and had no visible crown filling, caries lesion, or fracture. The tooth appeared to be sub-erupted with an apparent extension of the crown enamel to the lingual area (Figure 1). Response to the cold sensitivity test (Endo cold spray, Henry Schein, Langen, Germany) was normal in both adjacent teeth (lateral incisor and first premolar) and the affected canine.
The radiographic examination revealed a periapical lesion on tooth 33. Moreover, there was an enamel-lined invagination, apparently communicating with the oral cavity and running adjacent to the pulp root canal system from the coronal to the apical third of the root, ending in a malformed apex.
Apparently, a tooth malformation was establishing a direct communication between the oral environment and the periapical tissues, which was consistent with an Oehler’s dens invaginatus type IIIb (Figure 2). A cone-beam computed tomography (CBCT) (Promax, Planmeca, Helsinki, Finland) was performed to confirm the anatomic diagnosis and establish the treatment plan (Figure 3). Prior to the scanning, this imaging method’s importance was properly explained to the patient’s parents, who agreed to it.

Figura 2 Preoperative periapical radiograph revealing a dens invaginatus type IIIb associated with a periapical lesion
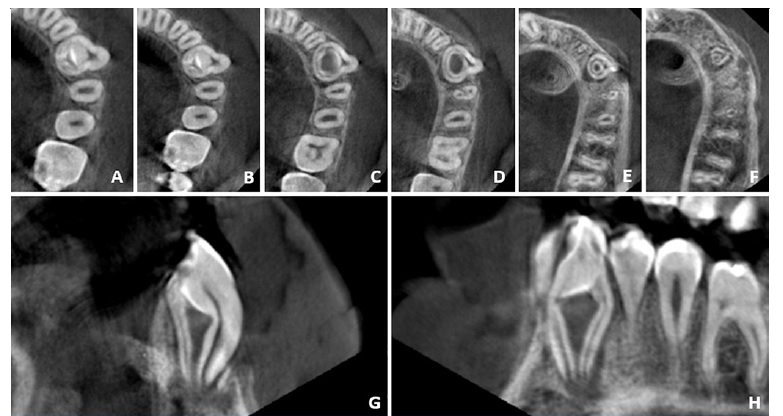
Figura 3 Different CBCT views revealing the characteristics of the dens invaginatus. (A-F) Axial slices from coronal to apical; (G) Sagittal view; (H) Coronal view
The clinician established an endodontic diagnosis of normal pulp and acute apical abscess, possibly originating from the passage of microorganisms from the foramen coecum to the apical area. The root canal treatment plan was proposed and accepted by the patient, who also filled the informed consent form.
The endodontic treatment was performed over three appointments due to time limitations. After proper anesthesia and rubber-dam isolation, access to the lumen of the invaginated tissues was performed under a dental operating microscope (Opmi Pico, Zeiss, Oberkochen, Germany) and having as reference the anatomic landmarks provided by the CBCT in order to avoid exposing the circular-like root canal system and, consequently, the pulp tissue. A high-speed round bur was used under water cooling to perform the access opening. The drilling started in the foramen coecum, which was observed in the crown enamel’s extension to the lingual area and confirmed in the CBCT examination. Access to the invagination lumen was achieved without exposing the pulp tissue, and the access was enlarged with ultrasonic tips (ProUltra, Dentsply Maillefer, Tulsa, USA) to perform proper lumen disinfection and space filling. A 0.10-sized stainless-steel k-file (K-File, Dentsply Maillefer, Ballaigues, Switzerland) was used to confirm patency. The working length was established using an electronic apex locator (Root ZX II, Morita USA Inc, Irvine, USA) and confirmed with a periapical radiograph. The apical size could not be determined due to being greater than a 0.80 k-file.
Copious irrigation with 5.25% sodium hypochlorite was performed, and irrigant sonic activation was used (Endoactivator, Dentsply Maillefer, Ballaigues, Switzerland). A temporary filling material (Cavit W, 3M ESPE, Munich, Germany) was used between visits.
In the third appointment, with the patient already painfree and without abscess, the tooth kept its normal response to the cold sensitivity test. The final irrigation protocol included 60-second irrigation with 17% EDTA, followed by a final rinse with sodium hypochlorite. The invaginated tissues’ lumen was filled with ProRoot MTA (ProRoot MTA,
Dentsply Tulsa Dental, Tulsa, USA), which was delivered with an MTA gun (MTA gun, Dentsply Tulsa Dental, Tulsa, USA) and packed with a 0.30 size paper point’s (Zipperer, VDW, Munich, Germany) coronal back surface. The filling and packing quality were controlled with periapical radiographs (Figures 4, 5, and 6). The access opening was directly restored with a resin composite (Tetric Evoceram, Ivoclar Vivadent, Vaduz, Liechtenstein) (Figure 7). At the six-month follow-up, the patient remained pain-free, the tooth remained vital with a normal response to the cold sensitivity test, without any kind of discoloration, and apical radiolucency was almost completely resolved (Figure 8).
Discussion and conclusions
The complex internal morphology of dens invaginatus makes these teeth an endodontic challenge.11 The first case reports of conventional endodontic treatment on dens invaginatus are from the 1970s. Before then, teeth with this condition were considered to have a poor prognosis, and the best treatment choice was extraction.1,12
One of the most relevant clinical objectives is to preserve the teeth in the least invasive way possible, keeping their aesthetics and function as intact as possible. With increased knowledge of this condition’s morphology, different technical approaches have been reported and proposed according to the different types of dens invaginatus and the pulp health condition.
Treatment options may range from sealing or restoring the remaining enamel defect with resin composite to nonsurgical root canal treatment, pulp revascularization, endodontic surgery, or even intentional replantation, when the pulp is necrotic.3-5,11,12To confirm the diagnosis and have a more accurate understanding of the tooth morphology, using three-dimensional imaging is extremely important.3,8CBCT imaging provides a three-dimensional geometric tooth reconstruction with relatively low radiation.5,8 It has become an important tool for treatment planning.8,9
The present case is an example of Oehlers’s dens invaginatus type IIIb.6 In this case, the response to the pulp sensitivity test was normal. Thus, the treatment option established was the nonsurgical endodontic treatment of the invagination while simultaneously trying to leave intact the pulp tissue in the main root. This clinical approach has been previously recommended in cases with a pulp space separated from the invaginated lumen.1,3,12Although the dens invaginatus’ anatomy can be complex and should not be underestimated, the developments of modern endodontics made the management of this condition more efficient, reliable, and predictable.3,9
Approaching these cases with the help of dental microscope magnification and ultrasonic instrumentation has provided new abilities to the clinicians. Thus, the chemomechanical preparation became more predictable.12,13Ultrasonic tips provide a safer debridement of the coronal part of the root and serve to activate and enhance the irrigants’ efficacy.3 Nickel-titanium rotating instruments are not advisable for the apical part of the root due to the invagination’s inconsistency and the risk of instrument fracture. The use of conventional endodontic files is preferred.5,12
Regarding the final obturation, this unusual anatomy may lead to large apical sizes where conventional filling with gutta-percha may not be the best treatment modality.12) In the present case, MTA was used to fill the entire invaginated lumen space. MTA remains the gold-standard biomaterial for this type of procedure, and various in vitro and in vivo studies have demonstrated that it promotes tissue regeneration when in contact with the peri-radicular area. Moreover, it is biocompatible, prevents microleakage,14and increases the resistance to vertical root fracture.15On the other hand, it has the disadvantage of possibly leading to tooth discoloration,16which has not happened in the present case, at 6 months of follow-up.
Additionally, research has been devoted to determining the best timing to perform bonding procedures over MTA. Although the procedures at 7 days appear to present a superior behavior,17in the present case, it was performed immediately due to a patient management situation, to avoid a fourth appointment on a young patient.
Although the present case’s treatment was considered successful after six months, such cases should have a longer follow-up.3 There are different treatment options for dens invaginatus, depending on its type and pulp status. An early diagnosis is crucial, and even though dens invaginatus cases may be complex, a well-established treatment planning allied with modern endodontic techniques and biomaterials might provide a successful and predictable outcome. Accessing the invaginated lumen only while keeping the surrounding pulp tissue isolated and healthy might be a good clinical approach for dens invaginatus type IIIb presenting a normal pulp.




















