Introduction
Dental trauma is a worldwide public health problem affecting mainly school‑age children, with an average prevalence of 23% in primary dentition and 15% in permanent dentition.1
Traumatic dental injuries (TDIs) can be caused by falls,2 car accidents,3 and physical violence.2,3 As the practice of sports increases worldwide, it has become a progressively more prevalent etiology of dental trauma.4,5,6 According to a previous study,4 the prevalence of TDIs among athletes participating in the Pan American Games was 49.6%, of which 63.6% occurred during sports practice.
Some of the sequelae commonly found in cases of dental trauma are pulp necrosis,7 root resorption,7 coronary darkening,8 and loss of the dental element,9 as well as decreased quality of life.10,11The time elapsed between dental trauma and the first visit is crucial for determining the case’s prognosis.7 In cases of more severe trauma, such as avulsion, luxation, and root fractures, it is recommended that care be performed in emergency departments within three hours after the trauma has occurred.13 Therefore, immediate management associated with a correct diagnosis, besides careful clinical and radiographic follow‑ups, are the most effective ways to minimize the impacts caused by traumatic injuries.7
Considering the importance of a long‑term follow‑up in cases of severe TDIs, as well as the dissemination of these findings, this case report aims to describe a long‑term Clinical follow‑up of multiple sports‐related dental injuries.
Case report
This case was conducted according to the Helsinki Statement and was approved by an ethics committee. The case report was prepared according to the CARE guidelines.14 The patient signed an informed consent form authorizing the publication of the case’s photographs and details.
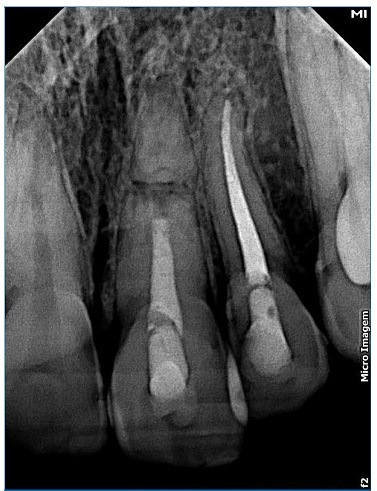
A 15‑year‑old Caucasian female patient was admitted to a private clinic 30 minutes after suffering a severe impact to the oral region during a basketball game at school in 2010. She was not wearing a mouthguard at the moment of the trauma. The intraoral examination revealed a cut on the lower lip and heavy bleeding in the maxilla’s anterior region (Figure 1). Besides, both teeth 21’s (left maxillary central incisor) and 22’s (left maxillary lateral incisor) crowns were slightly dislocated in a palatal and coronal direction, and tooth 21 had an enamel fracture (Figure 2). The patient had vital signs within the normal range and did not have any systemic alterations. Radiographic examination revealed a horizontal root fracture in the middle third of tooth 21 and an enlargement of the periodontal space of tooth 22 (Figure 3). Teeth 21 and 22 did not respond to the cold test with Endo Ice (Maquira, Maringa/PR, Brazil), while the response from teeth 12 (right maxillary lateral incisor), 11 (right maxillary central incisor), and 23 (left maxillary canine) was compatible with a normal pulp. The patient reported pain during the percussion exam on all teeth involved.

Figure 1 Clinical aspects at the emergency care: intense bleeding in the anterior region of the maxilla involving teeth 11, 12, 21, 22, and 23

Figure 3 Radiographic aspects at the emergency care: root fracture of tooth 21 and tooth 22’s extrusion
The teeth were diagnosed according to the classification criteria proposed by the International Association of Dental Traumatology (IADT),12 as follows:
• Tooth 12 - Subluxation;
• Tooth 11 - Subluxation;
• Tooth 21 - Enamel fracture, horizontal root fracture;
• Tooth 22 - Lateral luxation;
• Tooth 23 - Subluxation.
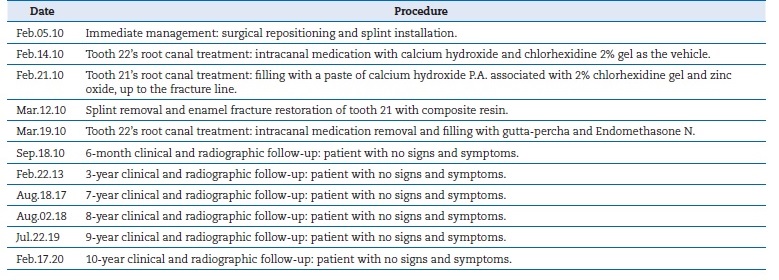
The clinical procedures are summarized in chronological order in Table 1. Firstly, under local anesthesia with 2% lidocaine with 1:100,000 epinephrine (Nova DFL, Rio de Janeiro, Brazil), surgical reduction of teeth 21 and 22 was performed (Figure 4). Subsequently, semi‑rigid splitting of teeth 12‑23 was performed with a 0.4‑mm
orthodontic steel wire (Orthometric, Marilia/SP, Brazil) and composite resin (Z100, 3M, Sumare/SP, Brazil) (Figure 4).
Nine days after the first visit, the patient returned, reporting spontaneous pain on tooth 22. Electric (Pulp Tester Digital, Odous De Deus, Belo Horizonte/MG, Brazil) and thermal (Endo Ice, Maquira, Maringa/PR, Brazil) tests were redone, and pulp necrosis of tooth 22 was suspected after negative responses. No definite diagnosis was reached for the periapical tissues due to recent trauma. The patient was anesthetized with 2% lidocaine with 1:100,000 epinephrine administered by buccal infiltration. The tooth was isolated with a rubber dam. Afterward, access and chemical‑mechanical preparation with rotary instruments (Protaper Universal, Dentsply Maillefer - Ballaigues, Switzerland) were done, and no bleeding was detected, confirming pulp necrosis. During the instrumentation procedure, 2% chlorhexidine gel (Endogel, Essencial Pharma, Itapetininga/MG, Brazil) was inserted into the root canal at each rotatory instrument change, followed by 5‑ml irrigation with saline solution.15 The root canal was drained and filled with an intracanal medication paste composed of calcium hydroxide powder (Biodinamica, Ibipora, PR, Brazil) and 2% chlorhexidine gel as the vehicle, in the proportion of 1:1.16 This intracanal medication was inserted with a lentulo spiral. Subsequently, the tooth was sealed with composite resin (Z100, 3M, Sumare/SP, Brazil).
A week later, the patient returned, reporting spontaneous pain aggravated by occlusion followed by pain during palpation on tooth 21 and edema in the region. Pulp necrosis was diagnosed after negative responses to the electrical and cold tests. No periapical lesion was detected. Endodontic treatment was performed following the same protocol used in the treatment of tooth 22. Special care was taken to keep the file tip within the tooth’s coronal fragment to avoid damaging the pulp of the root’s apical fragment. The root canal was dried and permanently filled with a paste of putty consistency composed of calcium hydroxide powder associated with 2% chlorhexidine gel and zinc oxide (S.S. White Artigos Dentarios, Ltda., Rio de Janeiro/RJ, Brazil). The paste was prepared in a 2:1:2 ratio, as proposed by a previous study.17 It was placed in increments with medium and fine‑medium vertical condensers up to the fracture line. Then, the root canal was sealed with composite resin (Z100, 3M, Sumare/SP, Brazil), and an incision was performed in the gingival mucosa to drain the abscess.
A month later, the patient came back with no signs and symptoms. The splint was removed, and the enamel fracture on tooth 21 was restored with composite resin (Z350, 3M, Sumare/SP, Brazil). One week after removing the splint, the patient returned asymptomatic to complete the endodontic treatment on her tooth 22. The intracanal medication was removed with rotatory instruments under abundant irrigation with 2% chlorhexidine gel and 0.9% saline solution, and irrigation with 17% EDTA for smear layer removal. Subsequently, the root canal was filled with gutta‑percha and Endomethasone N (Septodont, Saint‑Maur‑des‑Fosses, France) as root canal sealer. Lastly, her tooth was sealed with composite resin (Z350 - 3M, Sumare/SP, Brazil).
Clinical and radiographic follow‑ups were performed after 6 months, and then 3, 7, 8, 9, and 10 years. In the 10‑year control, the patient remained asymptomatic. Her teeth 11, 12, and 23 continued to respond positively to the sensitivity tests and seemed to be in function (Figure 5). Root fracture’s consolidation with rounding of the fracture edges, calcification of the apical third, bone formation between the fragments, and absence of periapical lesion or root resorption were noted radiographically (Figure 6). Moreover, the obturation paste of calcium hydroxide associated with 2% chlorhexidine gel and zinc oxide was still filling the root canal of teeth 21 after ten years.
Discussion and conclusions
Sports practice is commonly described as one of the main etiological factors of traumatic injuries in children and adolescents.4,5 In this case report, the patient reported suffering dental trauma during a basketball game in her school while not wearing a mouthguard. According to a previous epidemiological study,4 basketball is among the sports with the highest prevalence of dental trauma (70.6%), only after combat sports such as wrestling (83.3%) and boxing (73.7%). This prevalence shows the importance of wearing mouthguards during sports practice, especially in modalities that require physical contact. Accordingly, in their recent systematic review,18 the authors found a significant reduction in dental trauma prevalence among athletes who wore mouthguards (7.5%) compared to those who did not (59.5%).
Immediate management of severe dental trauma, preferably within three hours, is crucial for a better prognosis.13
In cases of lateral luxation and root fractures, IADT recommends immediate dental element repositioning followed by splinting for four weeks.12 In this case report, the patient came to the clinic 30 minutes after having suffered the trauma. So, her dental elements were immediately repositioned, and a semi‑rigid splint was placed and left immobilized for four weeks. The use of the splint in this study is justified by the lack of flexible material and the need to stabilize dental elements at that time. Although the IADT recommends the flexible splint to minimize the chances of dental ankylosis,12 scientific evidence is still inconclusive on the prognosis of luxated or fractured teeth with different types of splints.19,20,21,22,23Furthermore, case success seems to be more related to the kind of traumatic injury than the splint characteristics.24,25 In this case report, there were no radiographic signs of ankylosis or root resorption during the entire follow‑up period.
IADT recommends endodontic treatment for traumatized teeth to avoid root resorption if pulp necrosis is detected.12 In this study, the patient’s tooth 21 was diagnosed with pulp necrosis 14 days after the trauma due to not responding to sensitivity tests. The patient also presented painful symptoms. The preponderance of pulp necrosis in the coronary fragment after root fractures is about 20%, while the apical fragment remains vital in most cases.25 Thus, tooth 21 was treated endodontically up to the root fracture line12 and filled only with an obturation paste composed of calcium hydroxide P.A., 2% chlorhexidine, and zinc oxide.16 This paste has antibacterial properties;26 is biocompatible,27 and acts as a physical barrier, helping seal root canals.28 It was originally proposed as a treatment for avulsed teeth but currently is equally used in the apexification of teeth with open apex28,30,31and the treatment of horizontal root fractures, with satisfactory results.16,29,32 That paste is used as a filling material in root fractures due to inducing the formation of a mineralized barrier,28,31 which was observed during this case’s radiographic follow‑up with roundness of the fracture edges and bone formation between the fragments. These findings are similar to those obtained by other authors33,34who filled the root canal of fractured roots with MTA. However, unlike in Yildrim and Gencoğlu’s study,33 no coronary darkening was observed in this case report. In addition, like in another case,34 the obturation paste used in this study was still filling the root canal after 10 years.
Pulp necrosis prevalence in permanent teeth after lateral luxation can reach 91.3%.35 Moreover, the longer the time between pulp necrosis and endodontic treatment, the worse the prognosis. IADT recommends monitoring tooth luxation to avoid false‑negative results from vitality tests. Likewise, root canal treatment should only be performed if there are clinical signs of pulp necrosis or radiographic evidence of periapical involvement.12 However, in this report, endodontic treatment was carried out 9 days after trauma, when the patient came to the clinic reporting spontaneous pain and having no response to the thermal, electrical, and cavity tests.
The use of chlorhexidine gel as a chemical substance for root canal system disinfection in our treatment protocol is of particular interest. Chlorhexidine is already widely used in dentistry because of its characteristics, including substantivity and a broad spectrum of antibacterial activity, and it is proven to have efficacy against bacteria present in the root canal of necrotic teeth.15,16A recent systematic review36 showed that both chlorhexidine and sodium hypochlorite effectively promote bacterial decontamination in
the root canal. In our research center, we adopted chlorhexidine as a standard chemical substance in all endodontic treatment cases, regardless of the etiology (caries, trauma, or prosthetic reasons). Over the years, we have obtained a great success rate from the cases treated with this protocol.37,38.39 However, there is still no randomized clinical trial comparing the clinical and radiographic outcomes of traumatized and necrotic teeth treated with hypochlorite versus chlorhexidine.
Aside from emergency care and correct diagnosis, long‑term clinical and radiographic monitoring of traumatized teeth is imperative.12 This study presents a long evaluation period where the case’s positive evolution was observed, including total remission of signs and symptoms and no radiographic signs of periapical lesion or root resorption. In addition, after 10 years of follow‑up, teeth 11, 12, and 23 still responded positively to sensitivity tests.
This study is not free of limitations. Firstly, its scientific evidence level is low because it is a single case report. Secondly, the case has no computed tomography images, which prevents a more detailed analysis of root fracture repair.
In conclusion, it was possible to observe the long‑term clinical and radiographic success of multiple sports‑related dental injuries. This paper reinforces the importance of immediate care for the success of severe cases of dental trauma and the importance of using mouthguards as a preventive measure during sports practice.