Introduction
Pulpal and periodontal problems are responsible for more than 50% of tooth loss.1 The interrelationship between pulpal and periodontal disease may occur through the intimate anatomic and vascular connections between those tissues. These interrelationships have been traditionally demonstrated using radiographic, histologic, and clinical criteria.1 Several channels have been suggested as responsible for the interaction between the pulpal and periodontal disease processes.
These include neural (i.e., reflex) pathways, lateral canals, dentinal tubules, palatogingival grooves, periodontal ligament, alveolar bone, apical foramina, and common vasculolymphatic drainage pathways.1
The pathogenesis of an endodontic-periodontal lesion can range from quite simple to relatively complex. Knowledge of these disease processes is essential to determine the correct diagnosis.2 The key to success in treating these cases depends on taking a correct dental history to determine the cause and reach an exact diagnosis of the case development, leading to a very accurate and precise treatment strategy or protocol.3
The management of endodontic-periodontal lesions is truly challenging for the clinician because of the deleterious effects on the tooth structure and the supporting periapical structures. Nevertheless, current literature has been providing evidence of periodontal regeneration resulting in longterm retention in teeth with deep pockets associated with deep intra-bony defects, therefore changing the prognosis of these hopeless teeth.4 This case report aims to present the diagnosis and management of diferente endodontic-periodontal disease conditions with and without regenerative bone techniques.
Case reports
Case #1
An 18-year-old male patient was referred for an endodontic appointment at a private practice. His medical history was noncontributory. Examination revealed that tooth 36 (mandibular left first molar) had a previously initiated endodontic treatment and acute apical abscess, and tooth 37 (mandibular left second molar) responded positively to the cold sensitivity test (Endo Cold spray, Henry Schein, Germany) although with a lower intensity than the control tooth 46 (mandibular right first molar). Tooth mobility was within normal limits, and probing was within normal depths in all surfaces except the distobuccal and mesiobuccal of teeth 36 and 37, respectively (Figures 1 and 2), where the pocket depth was 10 mm with bleeding on probing. A cone-beam computed tomography (CBCT) was performed to better assess the extent of the boné lesion and showed the absence of cortical bone over the distobuccal and mesiobuccal surfaces of teeth 36 and 37, respectively, as well as a furcation defect in tooth 36 (Figure 3). A combined endodontic and periodontal problem was noticed. Tooth 36 was diagnosed with a true combined endo-perio lesion.5 Proper endodontic treatment and complementary external root scaling were proposed to and accepted by the patient, who gave informed consent.
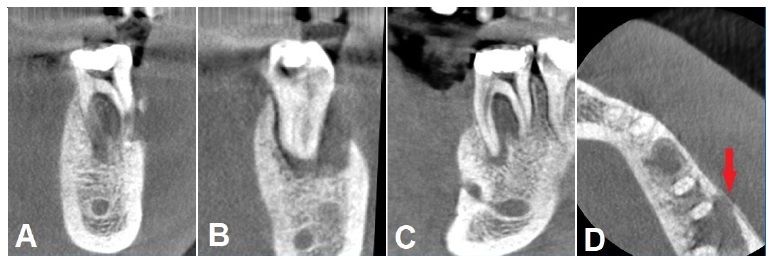
Figure 3 CBCT examination of tooth 36. A) coronal view of the mesial root; B) coronal view of the distal root; C) sagital view; D) axial view, the red arrows mark the endodontic-periodontal lesion
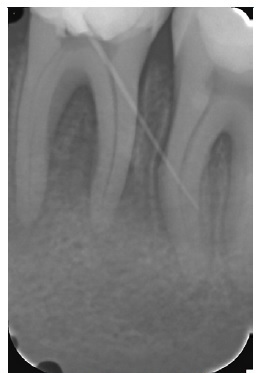
The endodontic treatment was performed under an operating microscope (Alltion AM - 4604, Alltion, China) in two appointments. In the first appointment, deep scaling of teeth 36 and 37 was done with ultrasonic tips, followed by irrigation with 0.2% chlorhexidine (Bexident Post, Isdin, Spain). After proper anesthesia with 1.8 mL of 4% articaine with 1:200.000 epinephrine (Artinibsa, Inibsa, Spain) and isolation with a rubber dam (R&S dental dams, CFPM, France), the access cavity was prepared on tooth 36. Upon establishing access with highspeed round burs and refining the access cavity with Endo-Z burs (R&S Dental Dam, CFPM, France), two mesial and two distal canals were found. The canals were scouted with ISSO 0.10 and 0.15 stainless-steel hand k-files (Ready Steel, Dentsply Maillefer, Switzerland), and working length was established with the electronic apex locator (Mini Root ZX, Morita, Japan) (Figure 4). All the canals were shaped with Wave One Gold Primary and Medium files (Wave One Gold, Dentsply Maillefer, Switzerland) coupled to a VDW Silver motor (VDW, Germany), according to the manufacturer’s instructions. Copious irrigation with 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain) at room temperature,7 using a 5-mL syringe and a 27-G notched needle (CanalPro Slotted-End Tips, Coltene, Australia) placed at least 1 mm from the apex,6 was done throughout the whole endodontic treatment. The tooth was provisionally restored with IRM (IRM, Dentsply, Switzerland) until the second session.
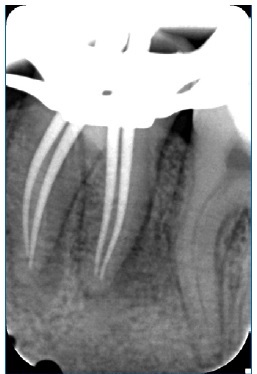
At the second visit, after cone fitting (Zipperer gutta-percha cones, VDW, Germany) (Figure 5) and manual dynamic agitation of the irrigants with the fitted gutta-percha points, the final irrigation protocol included one-minute irrigation with 17% EDTA (EDTA, Laboratorios Clarben S.A., Spain) followed by a final flush of 5.25% sodium hypochlorite.8 The canals were dried with paper points (Zipperer, VDW, Germany) and filled with gutta-percha and an epoxy resin-based sealer (AH Plus, Dentsply DeTrey GmbH, Germany) with the continuous wave of obturation technique using the B&L system (B&L system, Biotech, Korea) (Figure 6). The canals were sealed with a flowable composite resin (Supraflow R&S, CFPM, France), and the crown was subsequently restored directly with composite resin.
One month after completing the endodontic treatment, the patient was asymptomatic, and probing was within physiologic values in both teeth 36 and 37. Tooth 37 responded normally to the ice sensitivity test. A CBCT was done 12 months after treatment to plan implant placement at the site of tooth 35, and it showed almost complete restitution of bone trabeculation on the furcation area and buccally (Figure 7). The patient remains symptom-free.
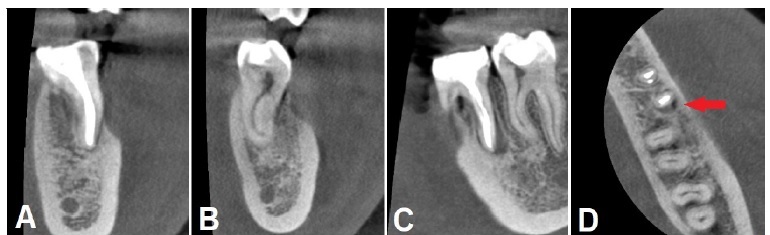
Figure 7 CBCT exam of tooth 36 one year after concluding the treatment. A) coronal view of the mesial root; B) coronal view of the distal root; C) sagittal view; D) axial view, the red arrows mark the remaining periapical lesion
Case #2
A 45-year-old male was sent for an endodontics appointment to perform the root canal treatment of tooth 46 (mandibular right first molar). The patient´s medical history was noncontributory, and he did not present any complaints. The only sign that raised some concern was a persistent fistula in the gingiva adjacent to tooth 46. The intra-oral examination revealed a large crown temporary filling on tooth 46. No secondary caries or potential fractures were visible. The tooth was asymptomatic on percussion, mobility was within normal parameters, and the buccal side near the furcation area had na 8-mm periodontal probing. The adjacent teeth responded normally to the ice sensitivity test (Endo Cold spray, Henry Schein, Germany), while no response was obtained in tooth 46. Radiographic examination revealed that the temporary filling reached the pulp chamber space, and the coronal root canal system had been enlarged (Figure 8). Bone radiolucency was observed apically in both roots and the furcation area. An endodontics diagnosis of previously initiated endodontic treatment with asymptomatic apical periodontitis,9 associated with a periodontal furcation defect (class 2 according to Hamp et al.10), was made. The endodontic and periodontal problems combined could be defined as a pulpal and periodontal lesion.
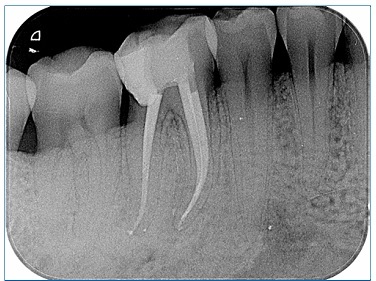
The root canal therapy complemented by a surgical approach to the furcation problem was proposed to and accepted by the patient, who gave informed consent. The general root canal treatment procedures followed the ones previously described for case #1. The endodontic procedure was made over two appointments under an operating microscope (Opmi Pico, Zeiss, Germany), the tooth was properly anesthetized, a rubber dam was placed, and an access cavity was prepared. After determining patency and working length, the root canal mechanical instrumentation was made using Wave One Gold Primary (Wave One Gold, Dentsply Maillefer, Switzerland). The root canal system space was irrigated with 5.25% sodium hypochlorite.7 No intracanal medication was used. In the second appointment, after the final irrigation protocol,8 the root canals were filled with gutta-percha and sealer with the continuous wave of obturation technique using a System B unit (System B, Sybron Endo, USA) and an Obtura II unit (Obtura II, Obtura Spartan, USA), and provisionally restored (Figure 9).
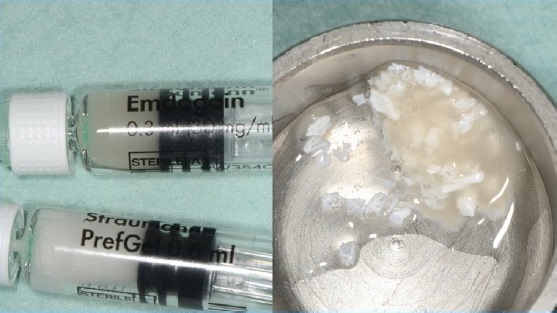
Two months after the root canal treatment, the patient was symptom-free, but the fistula was still present near the furcation area. The periodontal approach included a full-thickness flap to expose the furcation. The granulomatous tissue was removed with scalers, and then bone regeneration with Emdogain (Emdogain, Straumann, Switzerland) and Bio-Oss (Bio-Oss, Geistlich, Switzerland) supported by a Bio-Guide (Bio-Guide, Geistlich, Switzerland) membrane was made (Figures 10, 11, 12, 13, 14 and 15). The tissue was moved coronally to obtain first-intention healing and avoid membrane exposure (Figure 16). A 12-month radiographic and clinical follow-up showed periapical and periodontal healing, while the patient remains asymptomatic (Figures 17 and 18).
Discussion and conclusions
One of the main objectives in Dentistry is to preserve the tooth structures in a healthy and functional condition. Clinical cases with an endodontic-periodontic involvement, though having a poor prognosis, can still be solved when the Figure 12. Degranulation of the furcation area treatment follows a structured and interdisciplinary approach. Good oral hygiene, patient compliance, and the tooth’s restorability are considered the important requirements to decide to save the tooth rather than extracting it.11,12
A recent analysis by Setzer and Kim13 demonstrated that while the survival rates of endodontically treated teeth and implants are comparable, the success rates may not be. After 7 to 9 years, the success rate for implants was 74.0%, while for endodontically treated teeth was 84%. and the implant group had a significantly higher rate of complications.13Furthermore, in 17.9% of the implant cases versus only 3.6% of the endodontic cases, survival occurred because complications were treated.13 Peri-implant diseases are the major biological complication in implants,14 and the history of periodontal disease should be considered a risk factor for future peri-implant disease.14
Anti-infective therapy aims to suppress the bacterial load and establish a balance between bacterial burden and host response to allow for healing.15 As Sjögren et al.16 and Fabricius et al.17 showed, bacteria persisting in the root canal after chemomechanical procedures or intracanal medication will not always sustain an infectious process. Furthermore, intracanal medication can be inactivated by dentin, tissue fluids, and organic matter,18 presenting limited effectiveness in eliminating bacteria from the root canal.19 The literature also reports resistance to calcium hydroxide,15 a commonly used intracanal medication, by E. faecalis and Candida albicans.20,21
Therefore, due to the nature of the endodontic-periodontic lesion presented in the mandibular first molars, it was imperative that the therapy regimen included endodontic treatment, considering that achieving a proper chemomechanical debridement and complete sealing of the root canals is of the most importance.22
Vakalis et al.23 demonstrated that root canal treatment followedby periodontal treatment could be very effective and result in the improvement of clinical parameters together with alveolar bone gain.23 Endodontic-periodontal lesions with a primary endodontic cause and a secondary periodontal involvement should first be treated endodontically,5 and only after a 2- to 3-month period would any required and adequate
periodontal therapy be considered.24 The true combined and concomitant lesions require a treatment plan that envolves both endodontic and periodontal treatment from the beginning.
Due to the interactions between these diseases in the true combined lesion, the two treatments should not be too widely spaced in time to avoid re-contamination from the untreated cause.24 In case #1, both treatments were initiated in the same session. As for the concomitant lesions, such as in case #2, due to the independent pathological origins, the treatments may be more spaced in time, and the endodontic procedure should be performed first since the prognosis is mostly associated with the tissues’ response to periodontal therapy and further healing, which should not be disturbed by other pathological conditions.24 The results of the present case report suggest that guided tissue regeneration following root canal treatment resulted in a significant amount of bone fill and showed significant improvement in the clinical parameters when used in furcation defects.
Cortellini et al.4 in 2011 demonstrated that regenerative periodontal treatment is effective even in hopeless teeth and may therefore be an alternative to extraction.11 Regenerative periodontal treatment can be performed with guided tissue regeneration using a bone graft and membrane or using biological factors such as an enamel matrix derivate. Both methods result in a comparable clinical outcome,1 but enamel matrix derivatives offer less discomfort for the patient and show less postoperative complications.25 The use of an enamel matrix derivative has been shown to significantly improve probing attachment levels (1.1 mm) and reduce pocket depths (0.9 mm) when compared to a placebo or control, as discussed by Esposito et al.,26 and is also effective in treating class 1 and 2 furcation defects.27
Clinical protocols for regenerative procedures with enamel matrix derivates have suggested the use of EDTA for root surface conditioning to remove the smear layer produced by scaling and root planning and selectively remove the mineral from the dentin or cementum surface, exposing a collagenous matrix.28,29,30,31 However, the literature suggests no statistically significant differences in the reduction of probing depth and clinical attachment level gain following regenerative procedures with or without root surface conditioning with EDTA. Therefore, no EDTA was used in the clinical protocol of case #2.31
The present case report demonstrates that a multipronged approach can help improve and maintain the natural dentition to achieve health, comfort, esthetics, and function. The treatment should follow the suggested protocol, which starts with an oral prophylaxis session, immediately followed by root canal treatment of the affected tooth. Anti-infective treatment and periodontal regenerative therapy can then be performed to guide the wound healing toward the regeneration of lost periodontal structures. Further research, especially clinical trials, is needed to evaluate the suggested treatment approach or alternative options.32