Introduction
The success rates of root canal treatments are highly dependent on the technical procedures, such as mechanical debridement, disinfection, and obturation of the root canal system space.1Neglecting care during these procedures may contribute to the establishment of an intracanal infection, either due to the growth of bacteria previously present inside the root canal system space or due to coronal microleakage.
The misidentification of the tooth anatomy may lead to limitations in the clinical procedures and outcomes of the root canal therapy since the persistence of periapical pathology appears to be related to the failure to identify and treat all root canals.2 This issue is of particular interest in maxillary molar treatments, which have a considerable prevalence of missed second mesiobuccal (MB2) root canals.2 Their presence was first reported by Hess and Zurcher in 1925,3 and then gained clinical notoriety after 1969 when Weine correlated the clinical significance of misidentifying this anatomy with failed root canal treatment.4 Since then, the anatomy of the maxillary molars’ mesiobuccal (MB) root has been extensively investigated by several clinical and laboratory studies.5
The high prevalence of multiple root canals in the MB root may be associated with the broad buccolingual dimension of the root and the presence of concavities on its mesial and distal surfaces.6
Although fewer studies have analyzed the maxillary second molar (MSM) morphology compared to studies on the maxillary first molar’s, both revealed the existence of great anatomical variability.7 It is widely recognized that the root canal system morphology is highly variable and may display some quite uncommon configurations. However, to date, there is no report of the presence of four MB (MB1, MB2, MB3, and MB4) root canals in the MSM. Therefore, the present study aims to report the successful root canal treatment of an MSM with six canals, of which four were in the MB root.
Case report
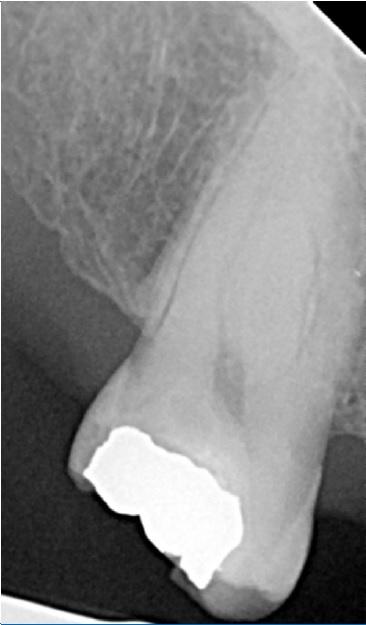
A 37-year-old Caucasian female patient was referred to an endodontic appointment with complaints of constant pain on the maxillary right side with irradiation to the preauricular area, not associated with thermal stimuli. Her medical history was noncontributory. The intra-oral examination revealed a distobuccal (DB) caries and an occlusal amalgam restoration on the maxillary right second molar (tooth 17) (Figure 1). The buccal surface of the MB cusp had an additional cusp - a paracone. The patient had no pain on palpation, and the mobility test and periodontal probing were within the normal limits, but there was tenderness to vertical percussion with no response to the cold sensitivity test (Endo Cold Spray, Henry Schein, Langen, Germany). The radiographic examination, conducted with periapical radiographs using the paralleling technique (Rinn XCP endodontics, Dentsply Maillefer, Switzerland), confirmed the presence of caries with no associated periapical lesion (Figure 2). The clinician established a diagnosis of pulp necrosis and symptomatic apical periodontitis.

Figure 1 Initial clinical photograph of tooth 17 revealing a large distobuccal decay and an extra cusp positioned on the buccal aspect of the traditional mesiobuccal cusp.
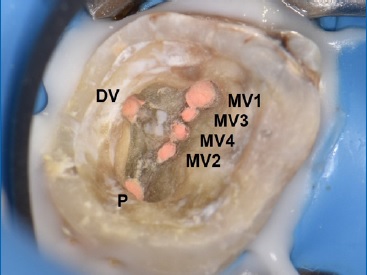
The treatment plan was non-surgical root canal therapy, which the patient accepted verbally and by filling an informed consent form. Infiltrative buccal anesthesia was performed with articaine HCL 4% plus 1:200,000 epinephrine (Artinibsa, Inibsa, Spain), followed by absolute rubber dam isolation and removal of the pre-existing amalgam restoration. No cracks or fissures were noted. The access cavity was established using round burs and refined with ultrasonic tips Start-X no. 1 and no. 2 (Start-X, Dentsply Maillefer, Switzerland) under magnification and lighting of a dental operating microscope (Alltion, Wuzhou, China). A careful observation of the pulp chamber floor revealed an extensive developmental groove between the MB and the palatal (P) root canals. The groove was explored with a DG-16 explorer and ultrasonic tips Start-X no. 1 and no. 2 (Start-X, Dentsply Maillefer, Switzerland), and three additional root canals (MB2, MB3, and MB4) were noted (Figure 3).

Figure 3 Pulp chamber floor after endodontic access, revealing four mesiobuccal orifice openings and single distobuccal and palatal canal orifices.
The root canals, which showed a supplementary Vertucci’s type XXI (4-1), were negotiated, and patency was achieved with #8 and #10 K-files (Ready Steel, Dentsply Maillefer, Switzerland).
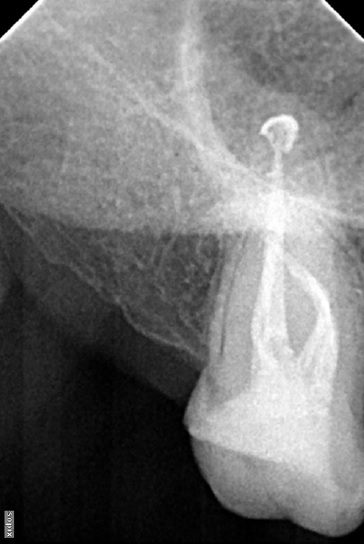
The working length was determined using an electronic apical locator (Root ZX Mini, Morita, Japan) and confirmed radiographically (Figure 4). Coronal preflaring was performed with an X rotary file (25.09, Endogal Endodontic System, Endogal, Spain) and the glide path with an A rotary file (15.03, Endogal Endodontic System, Endogal, Spain). The root canals were shaped also using Endogal System’s rotary files (Endogal endodontic system, Endogal, Spain) according to the manufacturer’s recommendations, at 250 rpm and 4.0 Ncm, with the sequence: B (20.04), C (25.04), and D (25.06) in all canals except for the MB, DB, and P root canals where the last file was an E (30.06) (Figure 5).
Copious irrigation with 5.25% sodium hypochlorite (Dentaflux, J. Ripoll SL, Spain) was performed throughout the procedure using 5-mL syringes with open-ended flat 30-G needles (Luer-Lock, Medibase, France). At the end of the first appointment, a temporary filling (Cavit W, 3M ESPE, Germany) was used to restore the access cavity. In the second appointment, a final irrigation protocol was performed with 10% citric acid, saline, and 5.25% sodium hypochlorite. In the end, passive ultrasonic irrigation was conducted (Irrisafe 20, Acteon, France).
The root canals were dried with paper points (Zipperer, VDW, Germany) and filled with gutta-percha and an epoxy resin-based sealer (AH Plus, Dentsply DeTrey, Germany) using the continuous wave of obturation technique accomplished with the B&L system (B&L, Biotech, Republic of Korea) (Figures 6 and 7). The access cavity was rinsed with alcohol, and the root canal orifices and the pulp chamber floor were sealed with flowable composite resin (Tetric EvoFlow, Ivoclar Vivadent, Liechtenstein). The tooth was permanently restored with cusp coverage composite resin (Tetric EvoCeram, Ivoclar Vivadent, Liechtenstein). At the 12-month follow-up, the patient was completely asymptomatic (Figure 8).
Discussion and conclusions
Current studies on the MSM reveal the existence of high anatomical variability.7,8The inner complexity of the MB root develops during morphogenesis and represents a constant challenge for professionals during root canal treatment.
In young patients, the continuous deposition of secondary dentin may narrow the kidney-bean-shaped MB root canal in the mesiodistal direction, shaping it into an isthmus connecting both extremities that may eventually close in certain portions of its length, creating multiple root canals.9
Because the lingual portion of the MB root is smaller, this dentin deposition over time may reduce the canals to dimensions that make them more difficult to locate. Additionally, the possible merging and fusion with other canals may lead to a more difficult identification and negotiation of these MB palatal canals.10
According to a recent CBCT study in a Caucasian population that included 778 MSMs, the prevalence of three-rooted morphologies was 73% and the proportion of MB2 root canals was 44%, highlighting the higher anatomic variability in MB roots.11 A recent meta-analysis that included cadaver imaging and intraoperative studies mentioned that the prevalence of the MB3 canal in MSMs was 0.3%.12 Several in vitro studies from different populations documented a prevalence of three canals in MB roots ranging from 0.6% to 4.2%,7,13 while in vivo assessments reported a prevalence between 0.2% and 1.8.13,14
The discrepancy in MB3 canal prevalence among studies may be related not only to the assessment methodology but also to the sample variability, even though the percentages are recurrently low. Despite the efforts to improve the methodologies of anatomy study designs for findings reliable and duly updated as possible,15 the prevalence of the MB4 canal in MSMs has not been documented yet.
In the present case report, four root canals were noted in the MB root, displaying a supplementary Vertucci’s type XXI (4-1) configuration according to Sert and Bayirli16 with both DB and P roots showing a Vertucci’s type I. The fact that a fourth root canal was observed in the MB root of an MSM highlights the root canal system’s unpredictability and the need for a careful evaluation of the pulp chamber floor during endodontic procedures. Previously documented case reports showing six root canals in the MSM are uncommon. Junior et al.17 and Chawla et al.18 described this configuration with two MB, one DB, and three P root canals, while Suresh et al.19 reported an MSM with fused roots and the existence of three MB, two DB, and one P root canals and Kim et al.20 documented two root canals in each of the three roots.
The present case also showed a paracone cusp. Firstly described by Bolk21 and later classified by Dahlberg,22 this extra cusp positioned on the buccal aspect of the traditional MB cusp may have its own pulp tissue and be linked to supplemental roots and root canal systems.23 Therefore, its presence, although rare, should not be ignored.
Several studies report a significant difference in exploring the pulp chamber floor with or without magnification.24 The use of the dental operative microscope became essential for detecting and managing all root canals in the present case.
Additionally, a proper access cavity design is of utmost importance for superior visualization of the entire pulp chamber floor and establishing straight-line access to the canal orifices. When extra canals in the MB root are suspected, the access opening may be extended mesially, creating a trapezoidal shape instead of a triangular one.25,26
The concomitant use of ultrasonic tips allows adequate exposure of the entire pulp chamber developmental grooves and respective canal orifices in a conservative manner, preserving pericervical dentin.27 Moreover, recent evidence showed that the dentin thickness in the danger zone of MB2 and MB3 root canals might be low, suggesting that these root canals may be best prepared with smaller instruments to avoid excessive dentin removal from a thin area.5,24 Due to the previous reasons, despite the small isthmus linking the four MB root canal entrances, the orifices were not united to avoid removing excessive dentin in the pulp chamber floor and from the pericervical area.
Additionally, these MB roots show great inner complexity involving multiple canals with merging and ramifications. Thus, proper debridement, irrigation protocol, and three-dimensional canal filling are even more technically sensitive and demanding.27,28
Knowledge of the internal root canal anatomy and its variations has a great impact on the diagnosis, management, and success of root canal treatment. Also, a specific armamentarium may be required to optimize the procedures, namely, the dental operative microscope, exploratory probes, and specific ultrasound tips. Therefore, adequate instruments combined with crown, root, and root canal anatomy awareness may lead to an outcome improvement of these cases. Figure 8. Twelve-month recall radiograph showing no radiographic changes.