Introduction
Restoring balance in a patient’s dentition often requires a multidisciplinary approach. When the treatment options to replace missing lateral incisors (MLI) involve orthodontic space closure, a minimally invasive approach to canine and premolar remodeling is often preferred over invasive interventions as a way to achieve functional and esthetic objectives.1-3 The most significant advantage of space closure over other approaches is that adolescents do not have to remain untreated until the facial skeleton matures.4
The replacement by an implant is also considered a possible solution. The main advantages are the possibility of obtaining an ideal occlusion, the maintenance of the canine in its natural position, and the clear benefit of avoiding any damage to the adjacent teeth.5,6The patient’s age is an inexact predictor of dental maturity because young patients develop at different rhythms.7 Nonetheless, the placement of implants in the anterior area presents some visible disadvantages, such as bone resorption, infra-occlusion of the implant, gingival retraction, recession of the interdental papillae, gingival changes (including blue staining of the gingiva), and exposure of the abutments.5,8-11
Unilateral agenesis is frequently associated with the dysmorphia or microdontia of the corresponding contralateral tooth.12 In particular, the microdontia of maxillary lateral incisors may represent a singular expression of molecular changes that impair the development of the incisors. As such, the condition should be considered in clinical diagnoses and when reviewing the patients’ family history as a way to identify agenesis.13,14In cases of microdontia, orthodontic planners may need to consider prescribing tooth positioning in all three dimensions if a future restorative treatment with minimal esthetic compromise is planned.15
The objective of this clinical report is to illustrate a minimally invasive approach to recovering esthetic disharmony due to bilateral maxillary lateral incisor agenesis (MLIA), unilateral MLIA, and microdontia using dental bleaching and a direct restorative procedure after orthodontic space closure.
Case reports
In three clinical cases, the procedures included clinical photography, radiography, and making impressions to produce study models. Orthodontic treatment involved space closure. Bolton’s anterior analysis was performed regarding tooth movement after orthodontic treatment with the six anterior upper and lower teeth.
Before the final restorative phase, at-home dental bleaching was prescribed in a 2-hour daily regimen with 16% carbamide peroxide (VivaStyle 16%, Ivoclar Vivadent AG, Schaan, Liechtenstein). The effectiveness of dental bleaching (dental color change) was evaluated before and after the bleaching treatment in the upper and lower incisors, canines, and premolars using a visual method (Vitapan Classical Shade Guide; Vita Zahnfabrik, Bad Sackingen, Germany), with the results indicating a color improvement to A1.
Four weeks after bleaching, single-shaded restorations were placed on the anterior sextant. After composite shade selection with tooth hydration, rubber dam isolation was applied to ensure an optimally clean and dry operating area. A silicone putty guide was fabricated from a diagnostic wax-up to obtain a favorable esthetic outcome with the addition of composite. Because the restorations were in enamel, we opted firstly to etch the enamel surface with phosphoric acid (Vococid®, VOCO, Cuxhaven, Germany) before applying a universal adhesive bonding agent (Futurabond U®, VOCO, Cuxhaven, Germany). To prevent the formation of an oxygen-inhibiting layer, glycerin gel was placed on the restoration and polymerized.
Finishing and polishing were performed using fine and extra-fine diamond finishing burs, abrasive discs, finishing strips, and felt-coated discs in conjunction with polishing paste (Enamelize, Cosmedent, Chicago, USA) with a felt-coated dental polishing buff (FlexiBuff, Cosmedent, Chicago, USA).
Case 1
Symmetrical bilateral MLIA
An 11-year-old female patient (Figure 1) presented with bilateral MLIA and a 2-mm midline diastema. An intraoral examination revealed healthy dentition and no symptoms or signs of periodontal disease (Figure 2). A panoramic radiograph showed the absence of both maxillary lateral incisors, mesial eruption of the canines, and the presence of deciduous maxillary canines and deciduous right maxillary lateral incisors (Figure 3).

Figure 1 Case 1: Initial frontal view before orthodontic treatment, still with deciduous lateral incisors and canines (2014).
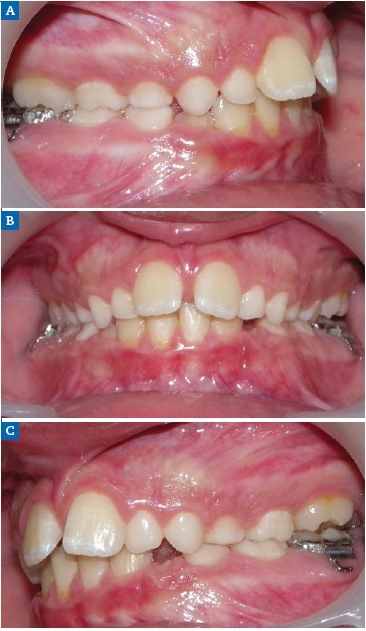
Figure 2 Case 1: Intraoral views of the (A) right, (B) frontal, and (C) left aspects before orthodontic treatment.

Figure 3 Case 1: Radiological investigation with a panoramic radiograph showing deciduous maxillary canines and right maxillary lateral incisor, as well as mesial eruption of permanent left and right maxillary canines.
Orthodontic treatment involving space closure was performed. After golden proportion (Figure 4) and Bolton’s anterior analysis, the presence of a 77.7% dental discrepancy in the anterior relation with mandibular excess was confirmed (14, 13, 11, 21, 23, 24, / 33, 32, 31, 41, 42, 43). Due to the agenesis of the maxillary lateral incisors and the need to perform esthetic restorations in the upper arch to improve smile harmony, a similar Bolton anterior discrepancy of 76% was obtained after restorations. After orthodontic treatment, shade selection was accomplished using a Vita Shade Guide (Figure 5), and dental bleaching was performed. Afterward, according to clinical findings and with careful consideration of all treatment options available for rehabilitation, it was decided that the maxillary canines and first premolars would be additively remodeled to the shape of lateral incisors and canines, respectively, using direct composite (Figure 6), which provides advantages in symmetrical cases.

Figure 6 Case 1: Maxillary canines and first premolars additively remodeled to the shape of lateral incisors and canines, respectively, using direct composite ((A) right, (B) frontal, and (C) left aspects).
Because the patient had a diastema, the risk of treatment relapse was overcome with long-term fixed retention using a bonded retainer (Figure 7).16 Meanwhile, the material used for the build-up was a hybrid composite (BRILLIANT EverGlow®, Coltène-Whaledent, Altstätten, Switzerland). Lastly, occlusal adjustments were performed, and final extra-oral photos (Figure 8) revealed a satisfactory integration of the restorations.

Figure 8 Case 1: Final frontal view after orthodontic treatment and composite build-ups (8-month recall, 2018).
Case 2
Asymmetrical unilateral MLIA
A 15-year-old patient presented with unilateral MLIA and microdontia (Figure 9). The left maxillary canine erupted mesially from its normal position, while the right maxillary lateral incisor was conical. Both central incisors were tipped to the left and associated with occlusal plane canting to the left. There was also an evident Bolton’s anterior discrepancy of 74.1 % (13, 12, 11, 21, 23, 24 / 43,42, 81, 71, 32, 33) due to maxillary asymmetric agenesis, a canine in place of the lateral incisor, and a conical contralateral (Figure 10). And due to agenesis of the mandibular central incisors and the presence of correspondent deciduous teeth. After the orthodontic treatment (Figure 11), the complexity of the asymmetric case required digital smile planning (Figure 12) and a diagnosis wax-up (Figure 13) to plan and visually demonstrate the desired result to the patient.

Figure 9 Case 2: Initial frontal view before orthodontic treatment, showing unilateral MLIA and microdontia.
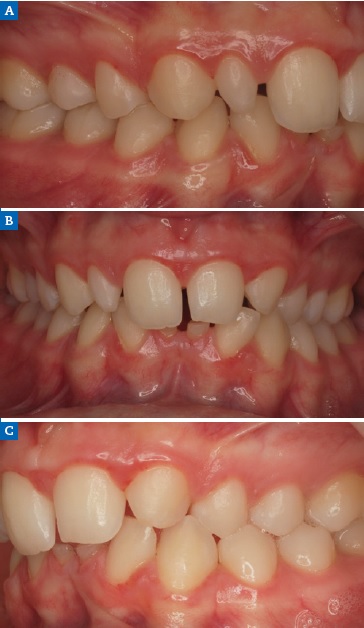
Figure 10 Case 2: Intraoral views of the (A) right, (B) frontal, and (C) left aspects before the orthodontic treatment.

Figure 11 Case 2: Intraoral views of the (A) right, (B) frontal, and (C) left aspects after the orthodontic treatment.
Left maxillary canine contouring procedures (Figures 8 and 9) were performed as indicated by the diagnostic wax-up.19 First, the canine eminence was reduced on the labial surface, and the tip of the canine was flattened to produce an incisal edge. Second, the distal incisal angle was slightly rounded to reproduce a lateral incisor. Third, ORMOCER® (ORganically-MOdified-CERamic) composite (Admira Fusion, VOCO, Cuxhaven, Germany) without bisphenol A (BPA) was added to the adjacent teeth to improve the distal and mesial dimensions of the left maxillary central incisor and left maxillary first premolar, thereby diminishing the canine and harmonizing the smile line (Figure 14). In addition, because the mandibular primary left central incisor presented mobility due to root resorption, it was extracted, and the mandibular primary right central incisor was restored (Figure 15).
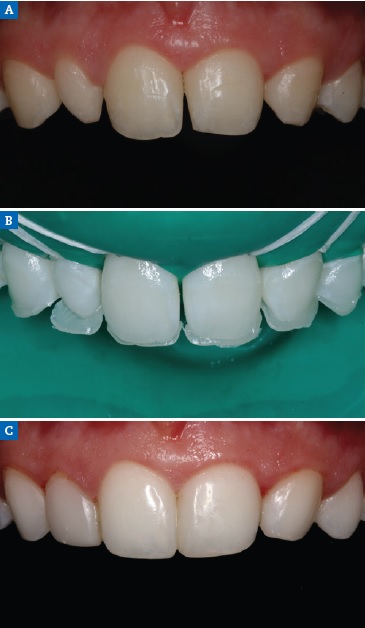
Figure 14 Case 2 restorative protocol: (A) Preoperative view, (B) Palatal shell in composite based on silicone matrix obtained from the wax-up, (C) One-year recall.

Figure 15 Case 2: Intraoral view after the extraction of the mandibular primary left central incisor and restoration of the mandibular primary right central incisor.
The occlusion was monitored at maximum intercuspation for protrusive and lateral guidance to assess any interference and obtain anterior guidance. Some adjustments were made in the left maxillary central incisor and left maxillary canine to promote optimal occlusion. With all the esthetic and functional limitations of this case with Bolton’s anterior discrepancy, a ratio of 70.6% was obtained. A ratio lower than 77.2% indicates anterior maxillary excess. Thus, it was explained to the patient that rehabilitation of the lower arch would be necessary in the future to compensate for the space caused by the deciduous mandibular central incisors’ loss and the volume of the mandibular central incisors that present agenesis to reduce the maxillary Bolton’s anterior excess. At the 1-year follow-up, the restoration revealed excellent marginal integrity and high polish (Figures 16).

Figure 16 Case 2: Final frontal view after orthodontic treatment and composite build-ups (1-year recall, 2018).
Case 3
Symmetrical microdontia
A 19-year-old female patient presented with primarily esthetic concerns. An intraoral examination revealed a Class I right molar, a Class II left molar, and a deep bite (Figure 17). Orthodontic treatment was performed to obtain bilateral Class I molar and canine relationship and, in turn, improve the overbite and remove the traumatic occlusion responsible for the gingival recession on the left mandibular incisor. Bolton’s anterior analysis confirmed a dental discrepancy in the anterior sector to mandibular excess with a proportion of 83.1% (13, 12, 11, 21, 22, 23 / 43, 42, 41, 31, 32, 33). It was caused by the maxillary dental microdontia and the need to carry out esthetic restorations in the upper arch. A space was created on the distal surface of both microdontic lateral incisors to establish the Bolton’s proportion17 (Figure 18). After orthodontic treatment, shade selection was accomplished using a Vita Shade Guide (Figure 19), and dental bleaching was performed to optimize the harmony of the smile.
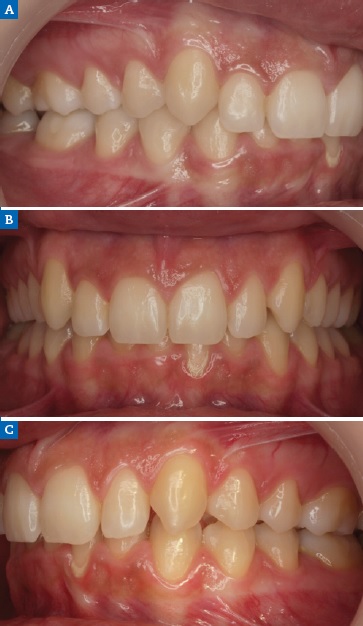
Figure 17 Case 3: Initial intraoral views of the (A) right, (B) frontal, and (C) left aspects before the orthodontic treatment, revealing a Class I right molar, a Class II left molar, and a deep bite.

Figure 18 Case 3: Intraoral views of the (A) right, (B) frontal, and (C) left aspects after the orthodontic treatment.
Then, to improve the morphology of the microdontic lateral incisors, a nanohybrid ORMOCER-based composite was applied. The right and left maxillary canines were also restored on the mesial face to enhance their anatomical shape (Figure 20A). This treatment plan made it possible to improve the Bolton discrepancy in the anterior mandibular excess relationship from a value of 83.1% to 79.6%. Diamond impregnated silicone polishers were used after occlusal adjustment (Figure 20B).
Cross-polarized photography revealed the monoshade resin color integration with natural teeth (Figure 20C). Intraorally, an optimal overbite and an overjet relationship were established, as was a good buccal occlusion with a Class I molar and canine. The gingival recession on the left mandibular central incisor was also improved. At the 3-year follow-up, the rehabilitation showed good soft-tissue adaptation and excellent esthetic maintenance (Figures 21).

Figure 20 Case 3 lateral view: (A) Postoperative view, (B) Final polishing, (C) Photography with cross-polarization.
Discussion and conclusions
Beauty is usually associated with harmony, which is one of the chief goals of esthetic rehabilitation. With a multidisciplinary team, cases of symmetrical or asymmetrical MLIA or microdontia can be harmonized.18
In treating cases with high esthetic demands such as those presented here, besides the position of teeth, it is important to consider the gingival architecture. In cases of MLIA, the extrusion of the canine and intrusion of the first permanent pre-molar typically mimic the gingival architecture associated with a natural smile.19
To optimize the harmony of smiles, it is important to evaluate the color before evaluating the morphology and proportion.
Canines present a more saturated color than incisors,20 which is more noticeable in more mesial positions such as in symmetrical bilateral MLIA (Case 1) and asymmetrical unilateral MLIA (Case 2). Following enameloplasty, color correction should be considered to brighten the teeth using bleaching techniques.21-23Moreover, the restorative procedure has to be completed at least 3 or 4 weeks after dental bleaching to prevent any negative effects of bleaching on bond strength and stabilize the color.24
Dental morphology and ideal tooth proportion were also important in the treatment plans for the three present cases.
According to Levin, the golden proportion (i.e., a constant ratio of 1.618:1) can be a guideline for determining the MLI width and, thus, was used in these cases.25 However, this guideline was more relevant in Case 2, an asymmetric case involving unilateral agenesis and microdontia on a contralateral tooth.25,26 Even so, it was somewhat inconsistent in terms of relative tooth width because the golden proportion results from perceived tooth size observed from a frontal aspect and thus had no relation with the teeth’ actual width. Another way to determine the amount of space to create for an MLI is the Bolton analysis,27 which we also used in all three cases. It is widely accepted that a diagnostic wax-up and a smile simulation provide the most effective and esthetic outcomes for patients, as performed on the asymmetric unilateral MLIA in Case 2.
The approach to space closure is improved when the canines have similar dimensions and both lateral incisors are missing, as in Case 1.18 In turn, in cases of unilateral MLI, like Case 2, the discrepancy in the canine’s shape, size, and color compared with the lateral incisor can make it more challenging to achieve an esthetic and, as much as possible, symmetrical result.
In Case 2, the restoration of the upper left canine to mimic the lateral incisor should be more incisal because it looks shorter than the upper right lateral incisor. In addition, the premolars are not totally in a Class II relationship on the left side to compensate for the excess Bolton anterior tooth discrepancy in the maxilla. This situation happens not only because of the permanent mandibular central incisors’ agenesis but also due to the presence of their respective deciduous teeth, which presented a reduction in mesiodistal size. To reduce the Bolton discrepancy, the premolars should be more mesialized and the left canine’s width reduced. Also, the space in the lower arch (central incisors’ area) should be increased to rehabilitate in the future. However, our goal was to leave space to rehabilitate one of the lower central incisors, considering the hypodivergent biotype, agenesis, and the consequent loss of bone structure.
For economic reasons, we opted to keep the deciduous tooth. However, the ideal procedure would be a rehabilitation with implants if the bone volume is favorable, or a Maryland.
According to some authors, a canine should usually be 1 mm wider than the lateral incisor that it will replace, which requires mesial and distal reduction and recontouring by enameloplasty to obtain the desired width.28 In Case 2, the canine eminence of the labial surface was reduced. On the other hand, in Case 1, with bilateral canine mesialization, only the additional approach with composite was needed to perform coronoplasty. Zachrisson demonstrated that if all of those reductions are executed using diamond burs with water spray cooling, the long-term implications for tooth sensitivity will be minimal.29
However, if dentine is exposed due to enameloplasty and/or recontouring, restoration may be necessary.29,30 In Case 1, the direct addition of resin to square off the mesial and distal incisal corners was more relevant to the final symmetrical result.
Furthermore, in Case 2, the left side of the first premolar was restored to appear like the maxillary canine. In Case 3, the patient presented with microdontia, which may represent a different expression of MLIA with a symmetrical outcome. A fundamental part of the overall treatment plan was orthodontic treatment to correct the deep overbite and traumatic occlusion and the Bolton discrepancy due to microdontic mesiodistal maxillary lateral incisors. After the orthodontic treatment, the restorative phase was essential to correct that discrepancy and consequently achieve more esthetic goals.31
In the present cases, direct restoration with composite was chosen over indirect restoration primarily because the treatment used did not involve any injury to dental tissue and was more affordable.32-34 The reversible nature of adding composite is a technique that allows for other treatment approaches in the future. An important benefit of that procedure over other restorative materials is that repair may be possible intraorally without risking the modification of esthetics or mechanical performance.35
It is clear from the available independent in vitro and clinical data that simplified adhesives are subpar compared to adhesives that include an extra hydrophobic resin, i.e., twostep self-etch and three-step etch & rinse adhesives.36-38However, when bonding to enamel, universal adhesives have good results and a much higher success rate as long as enamel is etched with phosphoric acid, which is the better way to improve the durability and stability of this adhesive system.36-38
There is no clinical evidence that nanofilled composite resin results in better overall clinical performance than hybrid composite resin.39-41According to different studies,42,43 nanofiller resin seems to be the most prone to staining, perhaps due to a sub-ideal dub integration of the nano-aggregated particles. In addition, hybrid composite resins result in a light propagation pattern similar to the natural tooth structure and better than nanofilled composite resin.44 Thus, one of the advantages of current hybrid composite resins over nanofilled composite resin is their excellent optical properties.45 Moreover, the nanohybrid ORMOCER-based composite is a BPA-free material. BPA monomer is an endocrine disruptor potentially linked to hormone-related problems like obesity and breast cancer, which should be considered when treating young patients.46 The decision to apply a single shade in these cases was highly favorable given the good optical color integration of that type of composite resulting from a chameleon-like effect and good polish retention.45 Photographs taken with a cross-polarizing filter allow clinicians to check the color integration of restorations because it eliminates specular reflections from the surface of teeth.47-49
Our results are similar to those reported by other authors who showed how anterior composite restorations demonstrated good clinical performance in the long term, with annual failure rates ranging from 0.0% to 4.1%.30,50 However, patients should be informed that restorations require periodic maintenance because the texture and shade of the material will change over time.
Patients with MLIA may require complex multidisciplinary care from a young age. Although harmonious outcomes are most challenging to achieve in cases of unilateral agenesis with microdontia, a carefully planned, methodically executed orthodontic-restorative approach can produce satisfactory results with a natural, definitive appearance that improves the patient’s self-esteem.






















