Introduction
Root canal treatment (RCT) involves the elimination of necrotic or vital pulp tissue and dental pain management. These outcomes are usually accomplished through proper mechanical preparation and the use of irrigation solutions.1 However, 1.9% to 28.8% of patients subjected to non-surgical RCT report post-endodontic pain (PEP) after treatment. This PEP originates from the periapical inflammatory response, provoked by biting and palpation, and usually persists from a few hours to many days, although 7% of patients experience persistente PEP for more than six months.2-5
The factors associated with PEP include the patients’ general health status, gender, periapical and pulp condition, apical patency, preoperative pain, obturation technique, instrumentation, and irrigants.6 Several preoperative procedures and pharmacotherapeutic agents have been proposed to diminish PEP, including the application of intracanal medicaments, occlusal reduction, and oral or parenteral administration of anti-inflammatories and analgesics. However, the effectiveness of these interventions in reducing PEP has not been comprehensively evaluated.7-9
Irrigation techniques are critical for successful endodontic therapy.10 Whereas several substances have been advocated for canal irrigation, the most frequently used irrigant is NaOCl.11-15 It has a significant antibiofilm activity, antimicrobial efficacy, and high ability to dissolve organic matter. The severity of NaOCl cytotoxicity depends on the solution concentration, pH, and duration of tissue exposure to the agent.16,17 The leakage of NaOCl during treatment may cause sequelae such as pain, swelling, bruising, and numbness comparable to a chemical burn.18 Moreover, due to the positive apical pressure generated during irrigation delivery, irrigant solutions may be pushed out into the periapical tissues, thereby inducing na inflammatory response and PEP.13,19 Therefore, safe and effective irrigation delivery systems are required to prevent the periapical inflammation associated with NaOCl use. Many irrigation devices have been developed using sonic or ultrasonic energy and apical negative pressure.20
EDDY (VDW, Munich, Germany) is a recently developed sonic irrigation activation device made with flexible polyamide, activated with 5000 to 6000 Hz using an air scaler.21 One study from 202122 evaluated the activation of NaOCl with EDDY and reported a similar pattern of PEP after 24 hours of EDDY and side-port endodontic needles irrigation. It reported no significant difference between EDDY and needle irrigation regarding the number of analgesics used.22 In this line of research, the present study aimed to compare the risk of PEP between irrigation using EDDY and manual syringe irrigation with needles with up-and-down movements (using a 27-gauge side-vented needle) among patients seeking initial non-surgical RCT. However, this study’s population is more representative of different clinical situations, including patients diagnosed with irreversible pulpitis and pulp necrosis, as well as patients with all levels of preoperative pain. The null hypothesi of the study is that there would be no difference in pain levels between manual irrigation and EDDY irrigation groups.
Material and Methods
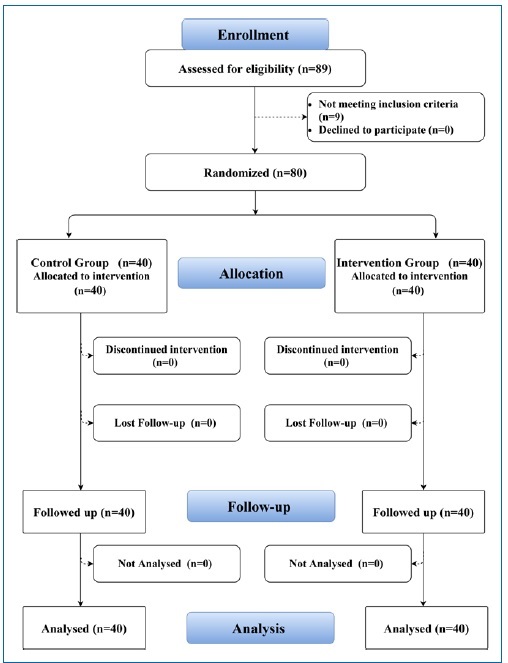
This prospective single-center randomized controlled clinical trial was conducted at the Dental Clinic of the Faculty of Dental Medicine of the University of Porto, Portugal, from February 13, 2020, to February 27, 2021. The study protocol was approved by the University of Porto’s Ethics Committee and documented at www.clinicaltrials.gov (ClinicalTrials.gov. Identifier: NCT03946306). The study was reported following the Consolidated Standards of Reporting Trials (CONSORT) guidelines.23
The patients were clearly elucidated on the clinical interventions and were aware of the potential adverse events associated with RCT. Informed consents were signed prior to study processing. The steps of the study were implemented following the guidelines of the Declaration of Helsinki.24 According to a previous study,22 40 patients per group were recruited to compensate for participant dropouts during the follow-up period. The patient selection had the following inclusion criteria: patients older than 12 years who had been diagnosed with irreversible pulpitis or pulp necrosis. The exclusion criteria were as follows: patients younger than 12 years, pregnant women, patients receiving prophylactic antibiotics or under steroid therapy >5mg/day, patients with uncontrolled hypertension or diabetes mellitus, chronic renal failure, hematologic diseases, human immunodeficiency virus, or osteoporosis treated with bisphosphonates, and patients who had a history of head and neck irradiation therapy. Teeth with abnormal root canal anatomy or advanced periodontal disease were also ruled out. A total of 80 single-rooted anterior and premolar teeth with fully formed apices were selected.
Our randomization and blinding were the following: A computer-generated random-sequence table was used to randomly assign the included teeth to either group. Randomization was performed using random block sizes (http://www.randomization.com/) with an allocation ratio of 1:1. The sequentially numbered, opaque, sealed envelopes (SNOSE) method was applied to conceal the sequence until the patients were assigned to their respective interventions. Patients were assigned to either intervention as they sequentially entered this study. The investigators and the patients were unaware of the assigned treatment arms during the study period.
The preoperative evaluation included a dental assessment to assess the pulp status, tooth type, and tooth location, and the recording of preoperative pain using the visual analog scale (VAS). The VAS is a 10-point scale in which the left side corresponds to no pain while the right side corresponds to the worst pain ever. We chose this method because it has a high response rate and high levels of completion, takes less than one minute to complete, requires almost no training, and is well received by patients.25,26Moreover, it is considered accurate, valid, reliable, and reproducible, and there is empirical evidence of inter-rater reliability and test-retest reliability.25,27
The pain was assorted into the following six categories: zero corresponded to no pain, 1-2 to mild pain, 3-4 to moderate pain, 5-6 to severe pain, 7-8 to very severe pain, and 9-10 to the worst pain ever. The diagnosis was obtained with the pulp sensibility cold testing. Periapical radiographs were taken to evaluate the status of the periapical structures.
All patients were treated by the same experienced endodontist and received local infiltration anesthesia (Xilonibsa: lidocaine, with 1:80000 epinephrine, Inibsa*) before RCT. Each tooth was isolated using a rubber dam, and the access cavity was made. The working length (WL) was determined using stainless steel hand files and confirmed by periapical radiographs.
The root canals were instrumented with a preflaring of the canals with #10 and #15 k-files and Protaper Next® files X1, X2, and X3. The selected root canals were irrigated continuously with 5.25% NaOCl using a conventional endodontic syringe with a side-vented 27-gauge needle. In the control group, the final irrigation was with manual syringe irrigation with needles, using 1.5 mL of NaOCl per canal for 30 seconds in an up-anddown motion, with the needle 1 mm short of the WL without binding, followed by a 30-second pause and a repetition of the irrigation procedure. In the intervention group, the final irrigation was made with 1.5 mL of 5.25% NaOCl per canal activated using EDDY tips, 1 mm short of the WL without binding.
The activation was performed for 30 seconds, followed by 30-second pauses, and this cycle was repeated according to the manufacturer’s instructions. After the final irrigation protocol, the canals were dried, and sterile cotton pellets were placed in the pulp chamber with a provisional restoration. No intracanal medicament was applied, in order to diminish variables. The obturation was executed in the following appointment.
The PEP was assessed by the VAS. None of the patients had analgesics prescribed immediately after the treatment, and all were advised not to take any analgesics at any point before the follow-up. PEP was assessed by phone at 8, 24, and 48 hours postoperatively. If any patient mentioned substantial pain, they were advised to take 600 mg of ibuprofen every 6 hours until the pain disappeared. Patients allergic to non-steroidal anti-inflammatory drugs were advised to take paracetamol.
Regarding the statistical analysis, continuous normally distributed data were reported in the form of mean and standard deviation and were compared using the Student’s t-test.
Non-normally distributed data were reported using median and range, and the related groups were compared using the Kruskal-Wallis test. Categorical variables were expressed in the form of numbers and percentages, and their particular groups were compared using Pearson’s chi-square test with Fisher’s exact test. Friedman’s post-hoc sign test was implemented to reveal the difference in the VAS levels at diferente time intervals within the EDDY and manual groups. The significance was established at p<0.05. Statistical analysis was performed using SPSS software version 25 for Windows (SPSS Inc., Chicago, IL, USA). Figures were renovated using GraphPad Prism (GraphPad Software, Inc, San Diego) software version 8.
Results
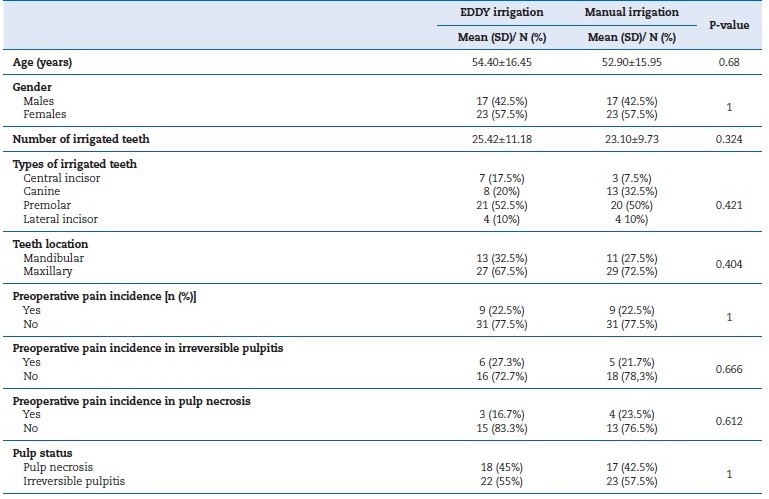
A total of 89 patients were assessed for eligibility to be included in this study. Out of those, 80 patients were randomly assigned to EDDY or manual groups. The mean age of the included patients was 54.40±16.45 and 52.90±15.95 in EDDY and manual groups, respectively (p=0.68). There was no statistically significant difference between both groups regarding the number of irrigated teeth (p=0.324), types of irrigated teeth (p=0.421), and teeth location (p=0.404) (Figure 1 and Table 1).
Regarding pulp status, 18 (45%) patients were diagnosed with pulp necrosis in the EDDY group, in contrast to 17 (42.5%) patients in the manual group. Irreversible pulpitis was diagnosed in 22 (55%) and 23 (57.5%) cases among EDDY and manual groups, respectively (Table 2).
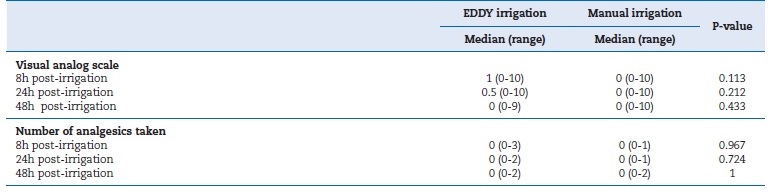
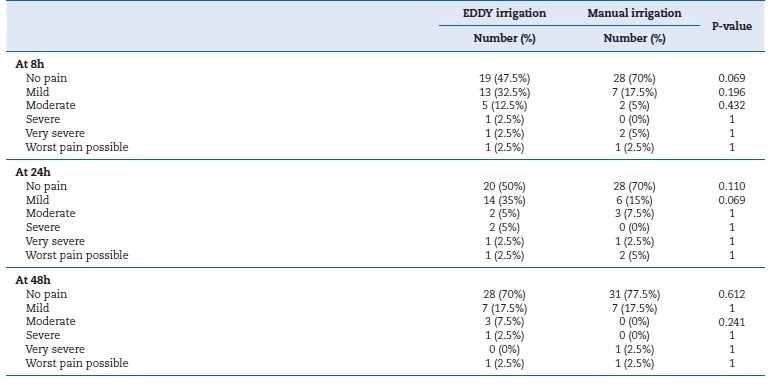
Considering the incidence and intensity of PEP eight hours after irrigation, the median levels of VAS were 1 (0-10) and 0 (0-10) among EDDY and manual groups, respectively (p=0.113).
Patients who received EDDY experienced a statistically significantly higher incidence (p=0.041) of PEP (52.5%) compared to the manual group (30%). Mild pain was reported in 13 (32.5%) and 7 (17.5%) cases among EDDY and manual groups, respectively (p=0.196). There was no statistically significant difference between both groups regarding the number of analgesics taken (p=0.967) (Tables 2 and 3, and Figure 2).
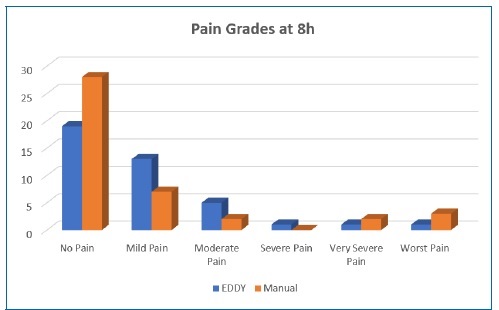
Figure 2 Bar chart showing the median levels of pain severity according to the visual analog scale between EDDY irrigation and manual irrigation groups at eight hours.
There was no statistically significant difference between both groups regarding the median pain levels 24 hours post-irrigation, with a median of 0 (0-3) and 0 (0-1), respectively. Post-irrigation pain occurred in 20 (50%) and 12 (30%) cases within EDDY and manual groups (p=0.068), respectively. The number of patients who experienced mild pain was 14 (35%) in the EDDY group and 6 (15%) in the manual group (p=0.069).
The difference in the median number of analgesics taken was not statistically significant between both groups (p=0.724) (Tables 2 and 3 and Figure 3).
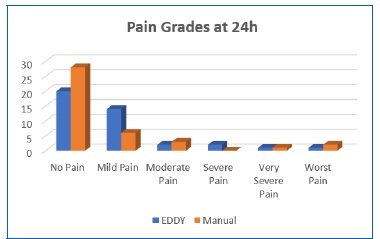
Figure 3 Bar chart showing the median levels of pain severity according to the visual analog scale between EDDY irrigation and manual irrigation groups at twenty-four hours.
The median levels of post-endodontic treatment pain 48 hours after irrigation were 0 (0-9) and 0 (0-10) in EDDY and manual groups, respectively (p=0.433). Then, 12 (30%) patients developed PEP in the EDDY irrigation group, in contrast to 9 (22.5%) patients in the manual group (p=0.446). There was a similar proportion of mild pain, accounting for 7 (17.5%) cases within both groups (p=1.000). Consequently, there was a similar median number of analgesics taken, 0 (0-2), among EDDY and manual groups (p=1.000) (Tables 2 and 3 and Figure 4).
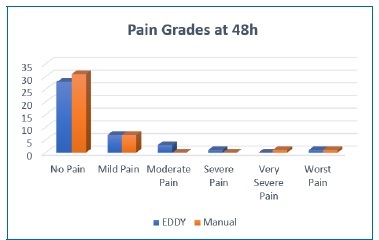
Figure 4 Bar chart showing the median levels of pain severity according to the visual analog scale between EDDY irrigation and manual irrigation groups at forty-eight hours.
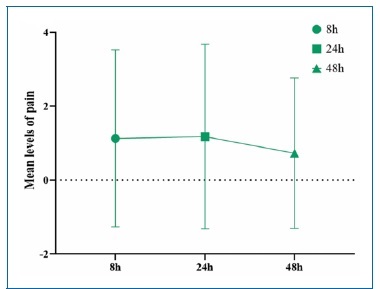
The VAS levels of patients who received EDDY were statistically significantly different between 24 hours and 48 hours (p<0.001) and between 8 hours and 48 hours (p<0.001). There was no statistically significant difference between the pain scores at 8 and 24 hours (p=0.375). As for the manual irrigation group, the median pain levels decreased significantly from 24 hours to 48 hours (p=0.004) and 8 hours to 48 hours (p=0.021) The median pain levels were similar at 8 and 24 hours (p=1.000) (Figures 5 and 6).
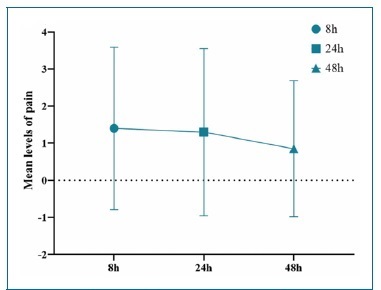
Figure 5 Line graph with error bars showing the mean levels of pain severity according to the visual analog scale at 8, 24, and 48 hours among patients who received EDDY irrigation.
Discussion
Methods to prevent PEP include proper selection of instruments, techniques of instrumentation, irrigants and devices used during RCT.6,28,29 A safe irrigation delivery system is desirable to prevent periapical tissue damage and lessen PEP.
However, the available evidence is limited, with few studies assessing the impact of using different irrigation devices on PEP during RCT. This clinical trial aimed to reveal the safety and efficacy of EDDY during initial non-surgical RCT on PEP. It showed that patients in whom EDDY was used experienced a higher rate of PEP, particularly during the first 24 hours after endodontic therapy. After such time, the pattern of PEP was similar between EDDY and manual groups. It is noteworthy that subjects were randomly assigned to each group and the degree of preoperative pain was not considered for this distribution.
The PEP rate showed a gradual descending trend with time, with pain decreasing noticeably at 48 hours post-RCT compared to pain at 8 hours. There was no difference between the number of analgesics taken at the end of the follow-up between EDDY and manual irrigations. This finding agrees with a study from 2011 that reported an approximate drop of 30% in pain prevalence from the first to the seventh day of endodontic treatment.30 Moreover, another study from 2021 reported a similar pattern of PEP after 24 hours of EDDY and side-port endodontic needles irrigation.22 It also reported no significant difference between EDDY and needle irrigation regarding the number of analgesics used. Contrary to the presente study, it reported a significantly lower PEP associated with EDDY compared to side-port endodontic needle irrigation during the first 24 hours.22
The highest association of PEP with EDDY might be related to the concentration of NaOCl used (5.25%) compared to a concentration of 3%.22 We chose this concentration because a study from 2012 observed that 5.25% NaOCl had better effectiveness in dissolving organic tissue, greater antibacterial action, a more alkaline pH, and a shorter effectiveness time.
However, it is more irritating to the periapical tissues.18 Accordingly, a 2019 study revealed a significantly higher PEP intensity associated with the application of 5.25% NaOCl in mandibular molars with non-vital pulp, compared to 1.3% NaOCl.31
The NaOCl cytotoxic effect may be further augmented by the rotating tips of EDDY, resulting in more debris extrusion and inflammation.32,33
Conclusions
EDDY during initial RCT is associated with a higher incidence of PEP, mainly in the 24 hours following treatment, compared to manual irrigation. Afterward, the rate of PEP was similar between EDDY and manual irrigation, with a gradual decline in pain intensity.
This randomized clinical trial is particularly important because there is little information about these topics. However, there are some limitations regarding the results’ evaluation because of the inclusion of random cases of pulp necrosis and irreversible pulpitis with different levels of perioperative pain.
Further randomized clinical trials with adequate sample sizes and longer follow-up periods are necessary to reveal the efficacy and safety of EDDY during initial RCT.