Introduction
Dental ceramic is considered ideal for restoration procedures, and the increased search for non-metal restorations has led to research and improvement of ceramic systems, such as zirconia.1-4Zirconia combines biocompatibility with excellent mechanical properties and a translucency more similar to natural teeth, thus reducing the risk of opaque areas.5-7Zirconia also has the advantage of being easy to fabricate using CAD/CAM technology.8 The greatest weakness of zirconia is its sensitivity to low-temperature degradation.9,10
There are currently two types of restorations with zirconia: stratified (veneered with glass-based feldspathic ceramic) and monolithic (polished or painted). Monolithic zirconia has been increasingly used to minimize the chipping of stratified zirconia.11,12 Some monolithic-zirconia systems have better aesthetic properties (more translucent), and others have better mechanical properties.13 Since monolithic zirconia has been used as an alternative to conventional ceramic systems, the ideal chairside finishing of zirconia should be discussed.
Ceramic restorations usually have a glazed surface that ideally should stay intact.1-3 The glaze is a vitrified layer that seals the pores of the ceramic’s surface. It is composed of a colorless glass powder that is melted over the last superficial layer, producing a light reflection similar to that of natural teeth.1-3 However, in clinical settings, ceramic restorations are sometimes subjected to occlusal and anatomic readjustments, usually conducted with diamond burs, which destroy the glaze surface, making it rough.14-16 Rough ceramic surfaces are more abrasive to antagonist teeth and restorations.17 Furthermore, the roughness of intraoral hard tissues favors the adhesion and retention of bacteria and, thus, may increase the risk of caries and periodontal disease.18 Other important features related to the roughness of ceramic restorations are that it may cause soft-tissue inflammation, favors pigmentation, causes a decrease in fracture resistance, and may result in unsatisfactory aesthetics.15,18
To reestablish the polishing of ceramic restorations, dentists may opt either for reglazing or using sets of polishing burs. A new glaze can only be performed in a laboratory and requires an extra session for the restoration procedure to be complete. Furthermore, an additional glaze firing may cause adverse effects on the ceramic, such as its devitrification.1 On the other hand, polishing systems can be a chairside procedure involving only one clinical session.15 When chipping or ceramic wear occurs, it is also imperative to reestablish the ceramic’s polishing.2
Considering the increasing need for intraoral polishing of zirconia restorations, this in vitro study aimed to evaluate the 2D and 3D surface roughness of different types of ceramic after finishing and polishing and compare three polishing techniques using three different polishing kits. Thus, the following hypotheses were studied: 1) There are no differences between the roughness of the three ceramics studied, and 2) For each ceramic, the polishing kit used does not influence the ceramic roughness.
Material and methods
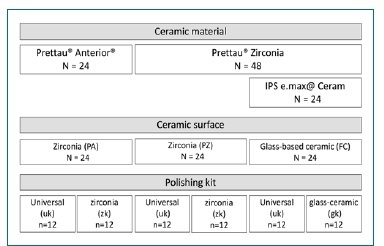
The roughness of three types of ceramic was studied after polishing the material surface with a universal or specific polishing kit. The sample size (n=12) was estimated with a power analysis based on the data from a pilot study, to provide statistical significance (α=0.05) at 80% power.
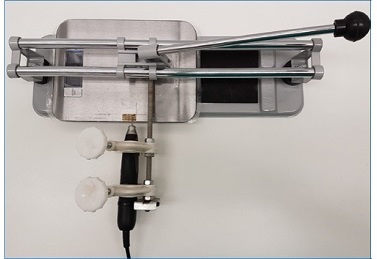
The specimens were obtained from 2-mm-thickness slabs of two types of 3Y-TZP zirconia: Prettau® Zirconia (Zirkonzahn SRL, Gais, Italy) and Prettau® Anterior® (Zirkonzahn SRL, Gais, Italy). Forty-eight specimens of Prettau® Zirconia and 24 specimens of Prettau® Anterior® were produced to achieve final standardized dimensions (length: 20 mm, width: 12 mm, thickness: 1.6 mm). After sintering according to the manufacturer’s instructions, all Prettau® Anterior® and 24 of the Prettau® Zirconia specimens were pigmented with the A3 color and glazed. A 0.4-mm layer of a fluorapatite veneering ceramic (IPS e.max® Ceram, Ivoclar Vivadent AG, Schaan, Liechtenstein) was applied, according to the manufacturer’s instructions, over each of the remaining 24 specimens of Prettau® Zirconia. Thus, three different groups representing three types of ceramic surfaces were set: Prettau® Anterior® (PA), Prettau® Zirconia (PZ), and IPS e.max® Ceram (FC). The specimens were uniformly worn by mechanically conditioning with a medium-grit diamond cylindrical bur (ISSO S6881 314 016 - Brasseler Lemgo, Germany) mounted in a laboratory handpiece (AnyXing 300D, Micro-NX Co., Ltd., Korea) at 10,000 rpm with water cooling. The bur was passed over the specimen’s surface for 20 seconds in a single direction, maintaining the bur’s long axis parallel to the surface under standardized pressure (1 N). A device with a parallelizer attached to the handpiece and a scale to control the exerted pressure was conceived to apply equal wear to every specimen. In this system, each specimen was fixed with double-sided adhesive tape (Figure 1). The bur was replaced after every five specimens to prevent wear changes.
The specimens of each type of ceramic surface were then randomly divided to create six experimental groups according to the several combinations between ceramic surface and polishing kit (Figure 2). A universal polishing kit ((uk) ref: 9771, Meisinger, Neuss, Germany) was used for half of the specimens of the three types of ceramic surface studied. A polishing kit designed specifically for each type of ceramic material was used for the other half: a kit specifically conceived for zirconia [(zk) ref: DCA04/DCA10, Meisinger] was used for PA and PZ, and a kit indicated for glass-based ceramic ((gk), ref: 9742, Meisinger) was used for polishing FC.
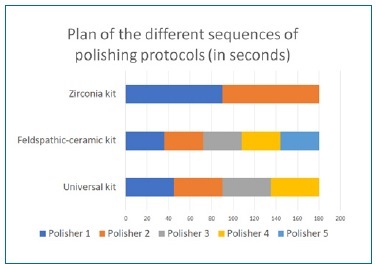
The polishers were inserted in a handpiece (10,000 rpm) mounted in the same device used to mechanically condition the specimens, as previously described. Polishing was performed for 180 seconds (90 seconds as in the previous step - xx axis, and 90 seconds perpendicular to it - yy axis) with each kit, regardless of the number of polishers used (Figures 3 and 4), according to the manufacturer’s instructions, under a standardized pressure of 2 N. After polishing and cleaning with ethanol, the 72 specimens were analyzed using white-light interferometry to assess the surface texture (Bruker NPFLEX, Stuttgart, Germany). Each reading was performed on a 1600x1600μm measurement area with a 10x magnifying lens, a lateral resolution of 1 μm, and a vertical resolution of 1 nm.

Figure 4 Zirconia polishing kit (left), glass-based ceramic polishing kit (middle), and universal kit (right) (Meisinger, Germany).
The Sa (mean roughness) parameter was selected for the 3D roughness analysis according to the ISO standard.19 The Ra (mean roughness) parameter was used to analyze the 2D roughness in each axis.
Statistical analysis was performed with standard statistical software (IBM SPSS Statistics, Version 25, IBM Corp., NY, USA). Since homoscedasticity was not set (Levene’s tests; p<0.05), non-parametric tests were used. Kruskal-Wallis tests, followed by multiple comparison tests, were used to compare roughness between ceramic surfaces (α=0.05). For each ceramic, the effect of the polishing kit was analyzed using Mann-Whitney U tests (α=0.05).
Results
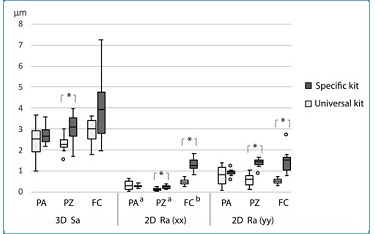
No statistically significant differences (p≥0.05) were found between the different types of ceramic surface for any parameter except the xx axis of the 2D Ra, with FC showing higher roughness (p<0.001) than both zirconia ceramics. Figures 5, 6, and 7 show representative images of the results obtained in 3D profilometry for each of the ceramic surfaces studied. The 3D Sa median value ranged between 3.9 μm for FC-gk and 2.3 μm for PZ-uk (Table 1). No statistically significant differences were found between polishing kits for PA (p=0.514) and FC (p=0.068) (Figure 8). However, polishing the PZ with the zk led to a significantly (p=0.004) higher 3D Sa than polishing with uk.
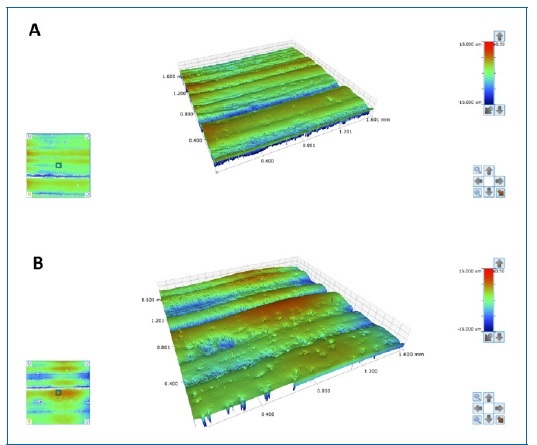
Figure 5 Profilometry 3D image of a Prettau® Anterior® specimen after polishing with the zirconia kit (A) and with the universal kit (B).

Figure 6 Profilometry 3D image of a Prettau® Zirconia specimen after polishing with the zirconia kit (A) and with the universal kit (B).
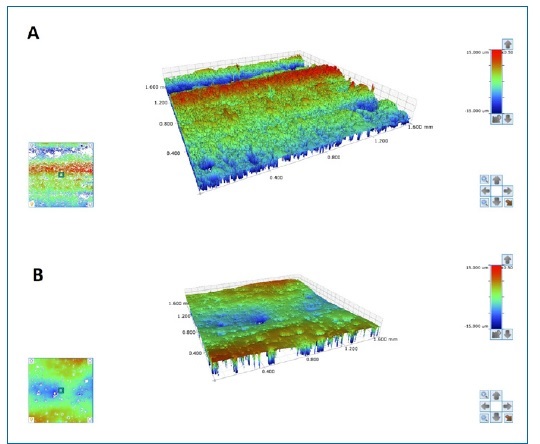
Figure 7 Profilometry 3D image of a glass-based ceramic specimen after polishing with the glass-based ceramic kit (A) and the universal kit (B).
Table 1 Descriptive statistics
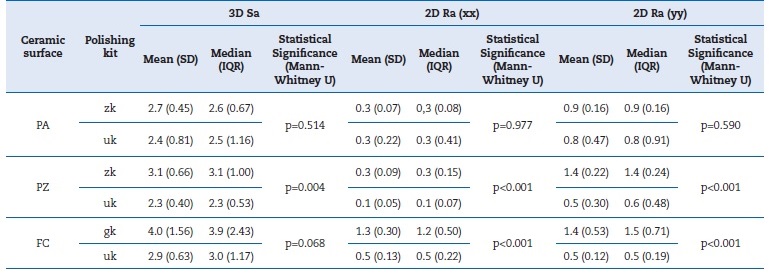
PA - Prettau® Anterior®; PZ - Prettau® Zirconia; FC - IPS e.max® Ceram; zk - polishing kit specific for zirconia; uk - universal polishing kit;
gk - polishing kit specific for glass-based ceramic; SD - standard deviation; IQR - interquartile range
The 2D Ra median ranged between 1.2 μm for FC-gk and 0.1 μm for PZ-uk in the xx axis and between 1.5 μm for FC-gk and 0.5 μm for FC-uk in the yy axis (Table 1). No diferences were found between the two kits used to polish the PA on neither the xx axis (p=0.977) nor the yy axis (p=0.590). Nevertheless, the polishing kit statistically influenced the 2D Ra of the PZ and FC. For both ceramic surfaces, the universal polishing kit achieved a significantly (p<0.001) lower 2D Ra than the specific polishing kit, both in the xx and the yy axis.
Discussion
Clinical occlusal adjustments of monolithic-zirconia restorations are inevitable. The required adjustments are conducted using fine-grit diamond burs because medium-grit burs cause 6 to 8 times more depth damage on the surface than those, thus compromising the strength and reliability of monolithic zirconia.8 However, this investigation used a medium-grit bur to simulate the worst scenario and thus enhance the diferences between the polishing kits.
Most studies analyze ceramic-surface roughness only at 2D.8,17,18,20,21However, surfaces with similar Ra might have different surface topographies. In order to better quantify and differentiate these surfaces, we also assessed 3D roughness.
The 3D evaluation takes into account the 3D characteristics of the ceramic surface and obtains images of the studied surfaces, which is not possible in the 2D evaluation. Regarding 3D roughness, Sa is a 3D parameter expanded from the roughness (2D) parameter Ra. Because Sa is little influenced by isolated extreme values, stable and consistent results can be obtained.22
Variations in roughness values might be explained by variations in the pressure exerted by the operator while handling the instruments, original defects of the samples, and small variations in the reading area of the roughness meter on the samples.23 In an attempt to avoid this problem, this study used a system conceived to control the exerted pressure to minimize potential errors in the wear and polishing processes.
Since differences were found between the ceramics in the xx axis of the 2D Ra, the first hypothesis in the study was rejected, with FC being rougher than zirconia ceramics. This finding may be explained by the FC’s lower hardness compared to surfaces like zirconia, which may have caused its specimens to withstand better the wear with the bur’s long axis parallel to the surface (xx axis).
The lower the Ra and Sa, the more effective the polishing system.20,22 Polishing both Prettau® Zirconia and glass-based ceramic with the universal kit allowed better results than using the specific kit (zk and gk, respectively) in every 2D and 3D parameter. Thus, the second hypothesis was rejected for these two ceramic surfaces. The uk is the most recent polishing set released by its manufacturer. This kit includes four polishers, while zk has only two. Several studies have warned about the importance of using a sequence of polishers to reduce surfasse roughness progressively.21,22 Although gk has one more polthan the shape of gk (points). Regarding PA, no relevant diferences were found in any of the assessed parameters between the two polishing kits, so, for this ceramic surface, the second hypothesis could not be rejected. This finding may result from the hardness of PA being higher than PZ’s, so it is more difficult to find differences between kits.
Future research assessing the clinical performance of polishing in the long term could consolidate the results obtained in this study. Comparing the Ra and Sa parameters and the surface wear after polishing in a brushing simulation machine may replicate what happens when ceramic wear occurs and can be a valuable and worthwhile approach.23