Introduction
Removable dentures have been used to treat edentulism for many years, and they still remain the most frequent option to replace missing teeth.1 Polymethylmethacrylate (PMMA) is the clinician’s first choice for various prosthesis fabrications. Besides denture bases, PMMA has other applications in dentistry: artificial teeth confection, individual trays, printed or milled models, occlusal splints, relining and repairing of dental prostheses, temporary crowns, and some orthodontic devices.2-5
PMMA is an odorless polymer of acrylic acid that was reported for the first time by Redtenbacher in 1843.6 However, the development of PMMA for biomedical applications was a gradual process that took decades. This polymer’s popularity for dental applications has increased since its introduction in 1937 in Philadelphia by Walter Wright and Vernon Brothers,7 due to its unique properties, such as aesthetics, cost-effectiveness, fit accuracy, low density, and easy manipulation.8,9 However, PMMA dentures can suffer fractures due to water sorption, poor impact resistance, and poor flexural strength. So, conventional PMMA has been modified to improve its properties (such as conductivity, water sorption, solubility, impact resistance, flexural strength, and surface hardness).2 Other shortcomings of PMMA are polymerization shrinkage, which influences dimensional changes and denture- base inaccuracies,10 and its biocompatibility, having been associated with mucosal irritation due to the presence of residual monomer.11
Some mechanical drawbacks in dentures, such as poor fatigue strength, low impact strength, and weak bonding strength, result in fatigue failure or accidental denture fracture.12,13 Denture fractures are a very frequent clinical issue reported worldwide. Approximately 70% of dentures have been reported to suffer fractures within 3 years of fabrication, with a 29% incidence of maxillary midline fractures.14 El-Sheikh et al.15 reported that repair was most commonly needed in mandibular partial dentures. Shakir et al.16 quantified several causes for PMMA denture fractures and found that accidental fractures covered 56% of the analyzed cases, poor denture fit 35%, heavy masticatory load 13.8%, fracture due to single complete denture opposed by natural teeth 12%, and acrylic resin breakage with age 5%. Naik17 demonstrated that denture fractures caused by the impact of an accidental dropping were the most frequent for both upper (25%) and lower dentures (53%). Therefore, further improvements in the mechanical properties of PMMA are desired, particularly their impact strength, flexural strength, hardness, and wear resistance.
Extensive research has been done to improve PMMA mechanical properties by changing its chemical structure and reinforcing the material using fibers or fillers of different types, sizes, shapes, and concentrations.18 Many additives, such as glass or carbon fibers, metal fillers, and nanotubes, have been incorporated into PMMA as reinforcements.19-21 Progress in nanosciences and nanotechnologies led to the development of new nanomaterials with properties different from those of the original material, whose use, for example, as additives, can improve the characteristics of the obtained materials.22,23 Studies showed that adding nanofillers is more efficient than microfillers in improving the properties of composites.24
PMMA-based materials should have specific desired properties depending on their biological application. Therefore, the PMMA used for denture-base materials should be biocompatible and not cause irritation, toxicity, or mutagenicity to the oral tissues.25,26 Chemically, PMMA needs to be highly insoluble in saliva and oral fluids and non-reactive to nutrients but should bond to artificial teeth.27 Additionally, it should have good mechanical properties to withstand the forces of mastication without failure. The current increased dependence on high flexural strength PMMA in prosthesis fabrication in dentistry led to searching for a suitable nanofiller that could provide increased flexural strength without compromising the remaining physical and mechanical properties and biocompatibility.28
Graphene is an atomically thin, two-dimensional sheet of sp2-bonded carbon atoms arranged in a honeycomb structure. It has shown many desirable properties, such as high mechanical strength.29 In fact, a single layer of graphene with a 1.0-TPa Young’s modulus and 130-GPa tensile strength is the strongest material ever discovered.30 In its pristine form, graphene is incompatible and lacks homogeneity. Thus, graphene oxide (GO) and reduced graphene oxide (rGO), derivates of graphene, enhance its matrix compatibility.31 Since its discovery in 2004 by Novoselov, graphene has aroused the interest of researchers due to its unique and exceptional mechanical, thermal, and electrical properties.32-34 These interesting attributes make graphene a better outcome than conventional nanofillers.35
Recently, nano-graphene and graphene-based nanocomposites have attracted attention in biomedical applications because of their unique and highly enriched physical and chemical properties.36,37 One of the disadvantages of graphene, which can be a limitation in prosthodontics, is its black color, despite the final color depending on its concentration in the resin.36
Although graphene is a very promising material for dental and biomedical applications,38 it is important to understand
the mechanical behavior of the new restorative materials reinforced with graphene to anticipate clinical performance and risks of failure. Thus, this systematic review focused on the effect of graphene-reinforced PMMA used in dentistry on mechanical properties.
Material and methods
This systematic review was conducted and reported according to the PRISMA guidelines39 (Preferred Reporting Items for Systematic Reviews and Meta-Analysis). The research protocol is registered in PROSPERO (International Prospective Register of Systematic Reviews) database (ID CRD42022308389) organized by the Center for Reviews and Dissemination (University of York, National Institute for Health Research, United Kingdom).
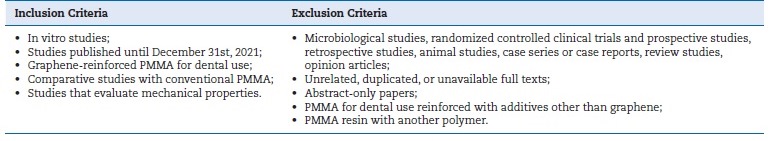
The research question “In dentistry, does graphene-reinforced PMMA offer better mechanical properties than conventional PMMA?” was formulated according to the PICO model, where the population (“P”) is PMMA for dental use, the intervention group (“I”) is graphene-reinforced PMMA, the comparison group (“C”) is conventional PMMA, and the outcome (“O”) is mechanical properties.40 The predefined list of inclusion and exclusion criteria used for this systematic review is detailed in Table 1.
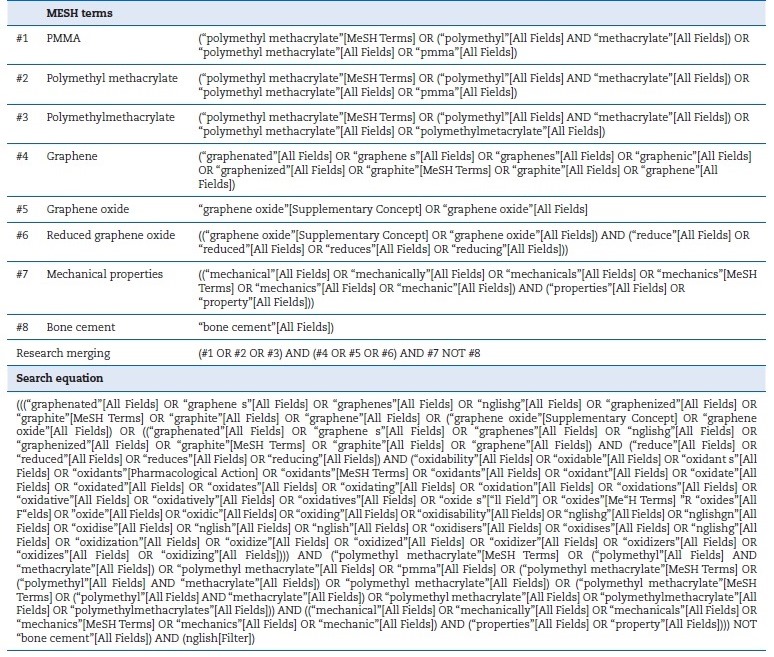
A systematic search in online electronic databases (Pubmed/Medline®, Web of Science®, and Embase®) was conducted using a combination of MeSH terms and unspecific freetext words with Boolean operators AND, OR, and NOT, without year restrictions. A gray literature search was also performed to ensure a maximum pool of relevant studies. In addition, the references of selected studies were also searched and included when applicable. No further searches were performed after the last update on December 31st, 2021. After some rounds of trial and refinement, the final search terms defined were “polymethylmethacrylate,” “graphene,” “graphene oxide,” “reduced graphene oxide,” and “mechanical properties.” The search strategy combined the different terms according to Table 2.
Two independent investigators selected the articles according to the PRISMA flowchart and later analyzed and evaluated them according to the established inclusion and exclusion criteria. The agreement was evaluated by Cohen’s Kappa coefficient.41 Disagreements, when present, were resolved through a consensus meeting. After the initial screening by title and abstract, the selected articles were obtained in full text. The selected full-text articles were examined, and their data were tabulated in a standardized Excel software spreadsheet.
The following information was extracted from each article: first author’s name, year of publication, brand names, manufacturers, sample size, specimen dimensions, mechanical tests, study objectives, and outcome.
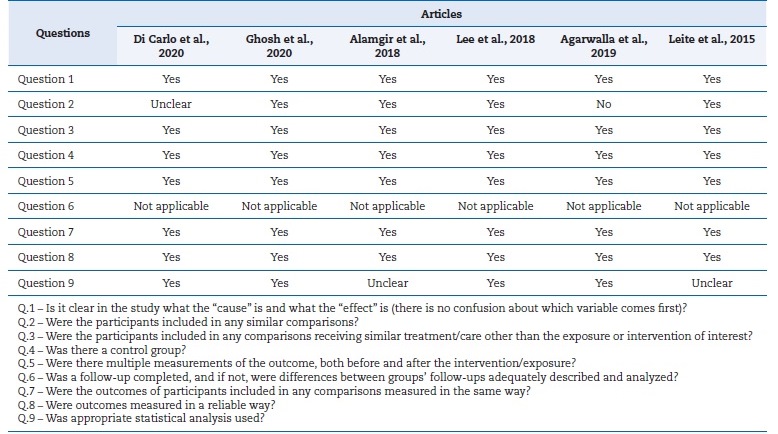
The criteria used to evaluate the quality of the selected prospective studies followed Joanna Briggs Institute Critical Appraisal Checklist for Quasi-experimental Studies (non-randomized experimental studies), which analyzes the methodological quality of the selected studies by answering nine questions with options “yes,” “no,” “not clear,” or “not applicable,” based on the characteristics of each study.42 Two independent reviewers (H.S. and P.F.) evaluated the quality of the selected studies, and any disagreement was resolved by a third author (P.M.).
Results
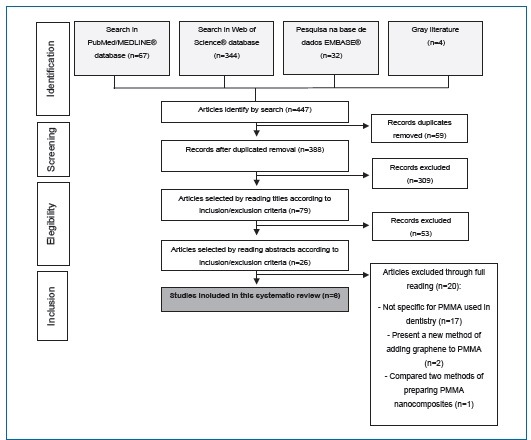
Figure 1 shows the flow chart of the identification and selection of the studies and the reasons for exclusion. The search strategy provided 443 articles, of which 388 were selected for further analysis after removing duplications. Title and abstract reading resulted in the selection of 26 articles for fulltext reading, of which 20 were excluded and six remained. A qualitative synthesis of the six final articles was carried out through a complete reading.
A Cohen’s Kappa test was performed to assess the level of inter-examiner agreement in the search for articles. The K value calculated was 0.96 for the first selection stage and 0.89 for the second one, representing a high degree of agreement between the two independent researchers. The disagreements were resolved through a consensus meeting.
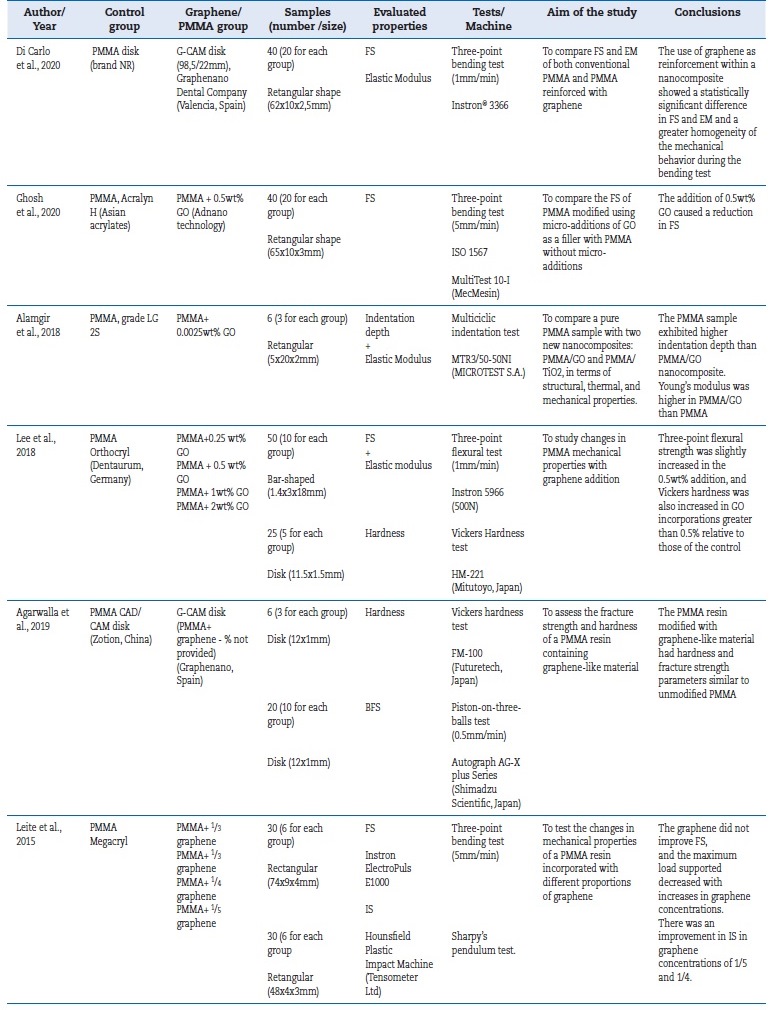
Table 3 shows the study description of each article. All the studies43-48 were conducted in vitro and included a total of 247 specimens, of which 81 were made of non-reinforced PMMA resin and 166 of graphene-reinforced PMMA resin. The mechanical properties evaluated were: flexural strength (FS), flexural modulus (FM), hardness, biaxial flexural strength (BFS), and impact strength (IS).
FS and FM were evaluated in most studies43,44,46,49 by a three-point bending test, performed using universal testing machines. Leite et al.48 found that graphene does not improve FS and that the maximum load supported decreases with increased graphene concentrations. However, graphene changed the ductility of the material. Di Carlo et al.43 compared the FS and FM of PMMA and PMMA reinforced with GO used in dental prostheses and verified that the mean values of both properties increased in the presence of graphene: FS from 96.32 MPa to 113.03 MPa and FM from 2.88 GPa to 2.96 GPa. Gosh et al.44 verified similar results in FS between the conventional PMMA resin (31.55 MPa) and the graphene-reinforced PMMA resin (29.72 MPa).
Lee et al.46 also studied the variations in FS and FM of a PMMA resin reinforced with different graphene concentrations and verified a statistically significant increase (p<0.05) of both properties in the 0.5wt% concentration. Agarwalla et al.47 evaluated BFS using the Piston-on-three-balls test and found it increased in the graphene-reinforced PMMA resin. The same study detected similar hardness mean values in the two types of resin, even though the reinforced resin had higher hardness.
In turn, Lee et al.46 found statistically significant differences in hardness between the non-reinforced resin and the resin with graphene concentrations equal to or higher than 0.5wt%. Alamgir et al.45 studied the micromechanical properties of PMMA and graphene-reinforced PMMA in a concentration of 0.0025wt% by multicyclic micro indentations and verified that reinforced PMMA was more resistant to localized deformation and had the highest Young’s modulus.
The risk of bias analysis in the studies showed low risk because most of the items questioned were evaluated as “yes,” which increased the reliability of the included studies (Table 4). The question regarding the follow-up period was answered as “not applicable” to the selected studies because the properties were evaluated a single time and not over time.
Discussion
PMMA gained popularity for various dental applications due to its unique properties, including its low density, aesthetics, cost-effectiveness, ease of manipulation, and tailorable physical and mechanical properties.49 However, there are several concerns associated with using PMMA, such as denture fracture due to water sorption and poor impact and flexural strengths. Thus, ongoing research has introduced several modifications to overcome and further improve its properties (such as its conductivity, water sorption, solubility, and impact and flexural strengths).50
Adding graphene and graphene derivative nanoparticles to polymer matrixes is a strategy for developing new materials.
However, little investigation has been done to understand the real influence of this nanomaterial in the mechanical performance of PMMA for dental use. Hardness, flexural properties, and IS are clinically relevant in the evaluation of materials for prosthodontics devices.51 Thus, this systematic review evaluated in vitro studies to compare the mechanical properties of PMMA and graphene-reinforced PMMA resins used in dentistry.
Hardness indicates the extent of resistance of a material to plastic deformation.52 The hardness of the acrylic resin suggests the risk of degradation of the polymer matrix: when hardness is reduced, the matrix degrades, increasing the material’s risk of fracture and, consequently, decreasing the useful life of the prosthesis.49 Lee et al. and Agarwalla et al.46,47evaluated this mechanical property and detected that adding grapheme increased the resin’s hardness, but only the first authors46 found statistically significant differences. This discrepancy in results can be explained by the unknown graphene wt% in the PMMA resin studied by Agarwalla et al.,47 as it may be too low to produce modifications in hardness. In fact, both Raman spectroscopy analysis and translucency parameter values obtained in that study suggest that the graphene-like material in the G-CAM disk was likely in the lower range of possible concentrations.
On the other hand, even though the hardness test performed in the two studies was the same, the machine used was different, which can also influence the results. Alamgir et al.45 investigated the characteristics of a graphene-reinforced PMMA nanocomposite for dental applications.
The authors performed a micro indentation test to analyze flexural properties. The results showed that the nanocomposite was more resistant to deformation and had a higher Young’s modulus than PMMA. The graphene was used to reinforce the PMMA resin at a concentration of 0.0025wt%, which is extremely low. Some studies have shown that the mechanical properties of polymers improved more with low graphene concentrations.53,54 An et al.53 even demonstrated that FS was degraded when the concentrations of GO were greater than 0.1wt%. Accordingly, Alamgir et al.45 used a very low concentration of GO and agreed that the presence of graphene might be positive in the reinforcement of polymers but only at low concentrations.
The flexural behavior can be considered one of the most important mechanical properties of the acrylic prosthesis. FM is related to a material’s stiffness and extent of deformation, and FS is a material’s capability to resist high functional loads.
The study of bending properties is a useful tool to compare materials usually subjected to masticatory stress.55 The studies that conducted the three-point bending test43,44,46,48 to evaluate FS and FM showed different results. Two investigations44,48 verified that graphene did not improve the resin’s flexural properties, and one of those, Leite et al.,48 determined that the increase in graphene concentration decreased the maximum load supported. However, this finding may result from the use of pristine graphene to reinforce PMMA resin since, in its pristine form, graphene is problematic to disperse in the polymer matrix and may aggregate due to high specific surface area.56
However, graphene has been shown to change the material’s ductility.48 Ductility represents the ability of a material to sustain a large permanent deformation under a tensile load before it fractures. This property is preferred in most design situations because ductile materials demonstrate extensive plastic deformation and energy absorption (“toughness”) before fracture.57
Gosh et al.44 observed that 0.5wt% of GO reduced FS compared to the control. This finding might result from the aggregation of graphene sheets, causing them to behave like micrometer-size fillers with a low surface area that tend to restrict the flow of polymer into the solution, resulting in the formation of voids that introduce stress within the matrix, making it susceptible to fracture.58 Conversely, Lee et al.46 reported that incorporating only 0.5wt% of nGO significantly enhanced FS and FM. Nevertheless, higher nGO concentrations (1wt% and 2wt%) showed decreased FS values (lower than the control). These contradictory results can be explained by differences between the two studies in the processes of grapheme addition to resin and oral-environment stimulation before the bending tests. Gosh et al.,44 kept the samples in water at 37ºC for two weeks, while Lee et al.46 kept them for only 48h. Di Carlo et al.43 also observed a significantly higher FS and FM in G-CAM resin compared to PMMA resin; however, the % of graphene in G-CAM resin in that study is unknown and may explain the difference in results. Agarwalla et al.47 evaluated the BFS to characterize the mechanical strength and reliability of the materials and verified a higher BFS in graphene resin, although without statistical significance. Once again, the absence of information regarding the % of graphene contained in the resin makes it difficult to interpret and compare the results with other studies.
The IS of a material is defined as its capability to resist a sudden applied load or force. In prosthodontics, it is an important predicting factor of clinical performance. Leite et al.48 verified an improvement of IS in the specimens with a lower % of graphene (1/5 and 1/4) compared to those without graphene. Once again, the lower graphene concentrations showed to be the most efficient in improving the mechanical properties of the resin. This finding agrees with Alamgir et al.45 results, despite having evaluated different mechanical properties.
Limitations of this systematic review include obtaining reduced and heterogeneous articles after the selection process. However, the inclusion criteria aimed to establish the greatest possible similarity between the included in vitro studies.
Conclusions
Considering the limitations and the diversified findings of this systematic review, we can draw the following conclusions: 1) Studies on graphene-reinforced dental resins’ mechanical properties are still in their initial stages, and more comparative studies are required; 2) Graphene offers important qualities to meet the desirable features in the confection of a dental prosthesis. However, no single graphene synthesis method yields a material with all mechanical properties improved; 3) Further studies are necessary to understand the ideal graphene concentration to improve resin’s performance.