Introduction
Since its emergence in 2019, COVID-19 has rapidly spread to create a global, socioeconomic, political, and public health threat.1 On March 11, 2020, the World Health Organization declared COVID-19 a global pandemic.2 By April 1, 2020, over 500 million positive cases and 6 million deaths had been reported worldwide.3
The pandemic has left numerous repercussions on society’s psychological well-being. Healthcare workers (HCWs) have dealt with great stress due to demanding work conditions.2,4-7Direct contact with infected patients, use of personal protective equipment, long working hours, and working under extreme pressures have predisposed this workgroup to mood disorders such as depression, anxiety, and stress.2,8-10These conditions are intricately related to other pathologies, from coronary heart disease to temporomandibular disorders (TMDs) and headaches.11
TMDs encompass a broad range of conditions of the temporomandibular joint, masticatory muscles, or associated structures.11 They are characterized by symptoms such as orofacial pain, joint noises, jaw locking, and headache.11-13
Although the etiology of TMD is still a matter of debate, current literature points to a multifactorial origin, including age, sex, stress, malocclusion, physical trauma, or underlying pathologies such as fibromyalgia.11
In 2014, Schiffman et al.14 proposed the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for clinical and research use. Its taxonomic classification for TMDs is divided into four main categories: (I) Temporomandibular joint disorders (TMJDs), (II) masticatory muscle disorders, (III) headache, and (IV) associated structures. The most common TMJDs are disk displacement and hypermobility disorders (luxation and subluxation).14 The International Classification of Headache Disorders (ICHD-3) recognizes TMD-associated headaches under the secondary headache category, with TMJDs as common pain generators.15
Although the existing literature has demonstrated increased stress levels among Portuguese HCWs during the pandemic, it has yet to show its influence on headache and TMD development.2,4,6,7 The authors hypothesized that the increased stress levels may have led to a higher TMD and headache prevalence among HCWs and that TMDs and headaches may have had a comorbid nature in this population.
Therefore, this study aimed to evaluate the overlap between emotional changes, TMDs, and headaches in healthcare professionals in a post-COVID-19 pandemic setting.
Material and methods
This cross-sectional web-based study examined Portuguese HCWs after the COVID-19 pandemic outbreak. A study protocol was sent to the Ethics Committee for Health of the Faculty of Dental Medicine of the University of Lisbon. This committee stated that, according to the Clinical Research Law (Law no. 21/2014) and Decree-Law no. 80/2018, this study did not require any ethical approval.
A survey was created using Google Forms and distributed via social networks through the non-probabilistic chain-referral sampling technique in February 2022. Written informed consent was obtained from all participants prior to participation through the first question in the questionnaire. Nonconsenting participants could not proceed with the questionnaire.
As inclusion criteria, all participants needed (1) to be healthcare professionals working in mainland Portugal, namely physicians, nurses, medical assistants, or senior diagnostic and therapeutic technicians; and (2) to work in hospital settings throughout the pandemic. Moreover, any worker with under three years of practice was excluded.
The survey comprised 52 questions regarding demographic data, emotional status, headaches, and TMJD symptoms. Demographic variables included age, sex, occupation, years of experience, academic qualifications, history of COVID-19 infection, displacement from regular residence, frontline involvement, work in the emergency department, average daily hours of mask usage, and average daily working hours. Headaches were addressed with questions based on the ICHD-3. For TMJD-symptom assessment, the authors selected a set of questions from the DC/TMD symptom questionnaire regarding jaw joint noise, closed jaw locking, and open jaw locking. The validated Portuguese translation for the 21-item Depression, Anxiety, and Stress Scale (DASS-21) was applied to assess symptom severity for each parameter. The DASS-21 measures the negative emotional states of depression, anxiety, and stress, through a 21-item 4-point Likert questionnaire. Each subscale was subsequently classified as “normal,” “light,” “moderate,” “severe,” or “extremely severe.” For descriptive purposes, any above-normal level was considered a positive diagnosis for that parameter. Statistical analysis was conducted using SPSS® Statistics (version 28.0, IBM®, Armonk, NY, USA). Because all variables were categorical, descriptive analyses were performed using absolute and relative frequencies. Regarding inferential statistics, p values under 0.05 were considered significant. For nominal variables, the phi coefficient was used for 2×2 contingency tables and Crammer’s V for tables over 2×2. Inferential analysis between two ordinal variables was conducted using the gamma coefficient.
Results
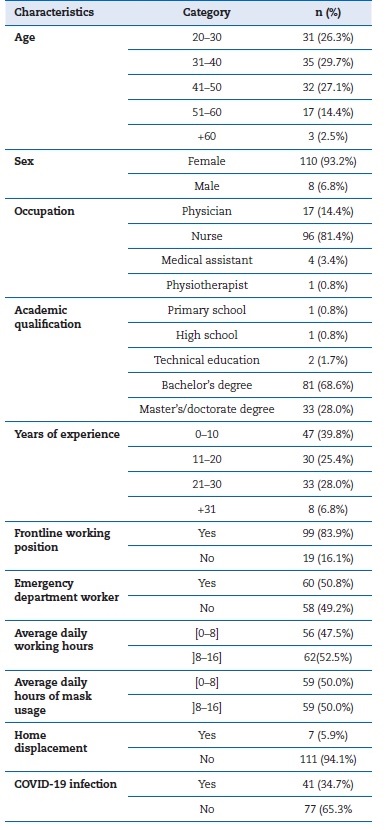
A total of 153 individuals participated in the study. However, as 31 began their professional practice halfway through the pandemic and three were not HCWs, only 118 were included in the final sample. As seen in Table 1, the sample included mainly nurses (81.4%), women (93.2%), and 31- to 40-year-old individuals (29.7%). DASS-21 results indicated that 58.5% of the sample had at least one positive parameter. The most prevalent negative emotional state was anxiety (51.7%), followed by stress (39.8%) and depression (38.1%). Moreover, moderate-to-severe symptoms were found in 38.1% of the sample for anxiety, 26.3% for depression, and 25.5% for stress (Table 2). Although stress levels fell predominantly in the “normal” category, an increase in this parameter was reported by 78% of the sample.
Table 2 Sample characterization according to depression, anxiety, and stress levels, headache, and TMJDs
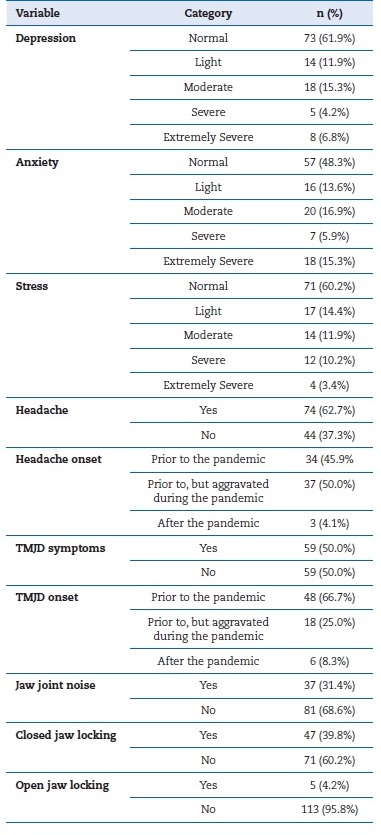
Regarding headaches, the sample showed a three-month prevalence of 62.7%. Whereas, for TMJD symptoms, 50% of the sample had at least one, and the most frequent was closed jaw locking, followed by jaw joint noises. The participants reported a high incidence and aggravation of these symptoms (Table 2).
Emotional subscales and demographic variables showed statistical significance (Table 3). Correlation values were interpreted according to their sign value (positive or negative) and magnitude (weak, 0-0.3; moderate, 0.3-0.7; and strong, >0.7). Depressive symptoms were significantly more severe in younger ages (p=0.003), lower school levels (p=0.026), and fewer years of professional practice (p=0.003). Greater anxiety levels were observed in younger individuals (p=0.039), nurses (p=0.047), individuals with lower academic qualifications (p=0.018), and individuals with fewer years of experience (p=0.047). Stress levels were significantly greater within younger ages (p<0.001), lower school levels (p=0.026), and fewer years of experience (p<0.001).
Table 3 Correlational analyses between the DASS-21 subscales and demographic variables (correlation value; p value)
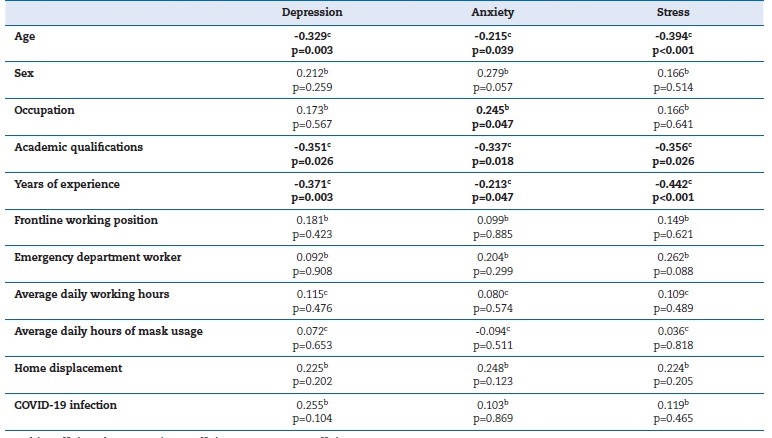
a - phi coefficient; b - Cramer’s V coefficient; c - gamma coeficiente
Bold p values indicate a significance value under 0.05
As seen in Table 4, the data analysis found statistical diferences between headaches and demographic variables, indicating higher prevalence rates among non-emergency department workers (p=0.012) and individuals displaced from their usual residence during the pandemic (p=0.035). The inferential analysis found no significant differences between the presence of at least one TMJD symptom and the demographic variables. However, it showed that jaw joint sounds were more frequent among younger individuals (p=0.001), women (p=0.048), individuals with fewer years of experience (p<0.001), and individuals with more working hours (Table 4).
Table 4 Correlational analyses between headaches and TMJD symptoms and demographic variables (correlation value; p value)
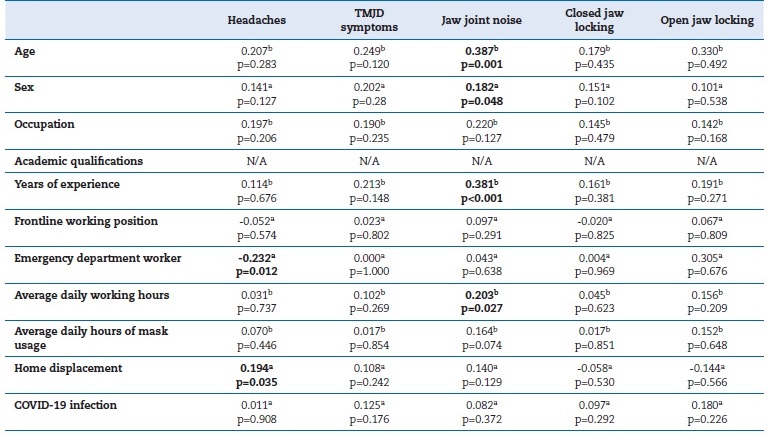
a - phi coefficient; b - Cramer’s V coefficient
Bold p values indicate a significance value under 0.05
Table 5 displays the comparative analysis between all main variables. Headaches were significantly more frequent among individuals with higher stress levels (p=0.034), with at least one TMJD symptom (p=0.004), and with jaw joint noises (p=0.001). Prevalence rates for TMJD symptoms were higher in individuals with greater levels of depression (p=0.009), anxiety (p=0.003), and stress (p=0.014). Joint noise frequency was significantly higher in participants with more severe levels of depression (p=0.027), anxiety (p=0.013), and stress (p<0.001). Closed jaw locking was significantly more frequent in individuals with increased anxiety levels (p=0.004).
Discussion
The pandemic has created unprecedented challenges, posing a threat to Portuguese HCWs’ mental health.2,4,6,7The presente study corroborates these findings, given the sample’s high degrees of depression, anxiety, and stress.
Our sample reflects the population under study, mainly comprised of nurses and female HCWs.16 However, our sample seems to overrepresent these groups. As such, inferential analysis regarding these variables may be biased.
The authors found that nurses, younger individuals, professionals with fewer years of experience, and professionals with lower academic qualifications were associated with higher depression, anxiety, and stress scores. A previous study on Portuguese physicians also found that younger individuals were prone to increased emotional stress during the COVID-19 pandemic.2 This tendency could be due to a lower capacity to adjust to the pandemic. Previous studies have reported that women and frontline HCWs were at higher risk for psychological disorders.2,7,17,18 However, our study found no significant differences among these groups, which may be due to the sample size and the underrepresentation of the male sex.
The authors found a 62.7% three-month prevalence of headache, which was higher than the global headache prevalence in adults (46%), as determined by Stovner et al.19 Current evidence lacks consensus on the relationship between headache disorders and age or sex in healthcare professionals during the COVID-19 pandemic.20-22 Some studies report no association between these variables, as found in the presente study.20,21On the other hand, Ramirez-Moreno et al.22 contradicted these studies by finding a predisposition for de novo headaches in women and younger individuals. In 2021, Romero et al.23 published a narrative review on the impact of the pandemic on the presence of headache disorders in healthcare professionals, where they recognized the influence of personal protective equipment and face masks on headache incidence.
This finding may justify the emergence of de novo headache disorders and the aggravation of pre-existing conditions in this sample.
Half of the sample had at least one TMJD symptom. Although this prevalence has not yet been studied in this population, it is higher than the one (37%) Hayek et al.24 found in Saudi Arabian physicians before the pandemic outbreak. Studies state that joint noises and facial pain are the most common TMJD symptoms.24-26 However, our study did not corroborate these studies, given the preponderance of closed jaw locking among its participants. This symptom is not exclusively consequente to TMJD, as it may be associated with infections, trauma, and neoplasms, among others.27 Thus, the lack of a clinical examination and the small sample size may have led to overestimating said symptom. Data shows that women were at higher risk for joint noises, supporting other epidemiological studies.11,12,28 Similarly, younger individuals showed higher rates of this symptom. A study by Manfredini et al.29 also showed a predominance of disk displacement among this group, supporting this investigation’s findings.
The authors found a significant association between higher depression, anxiety, and stress scores and TMJD symptoms.
With researchers being aware of this association, they have frequently observed it among at-risk populations such as HCWs.24,30 Comparably, other vulnerable populations, such as students, seem to follow this trend.22-33 Studies have also shown a positive association between headache disorders and depression, anxiety, and stress scores.34,35 The present study observed this relationship, albeit solely for stress levels.
The relationship between headaches and TMJD is still a matter of debate. A positive association has been shown in previous studies, with disk displacements, degenerative joint disease, and hypermobility disorders being common pain generators.15,36 The present study found significant differences in headache prevalence among individuals with TMJD symptoms, supporting that these are comorbid disorders.
Despite its significant findings, this study does not come without limitations. The chain-referral-sampling technique is not free of putative bias due to the participants’ interest in responding to the survey. Moreover, its online nature might have limited the accessibility to the survey by certain groups.
As a cross-sectional study, the variables’ temporal evaluation was not entirely possible. Other sociodemographic variables could have been considered, such as the main sector of practice (public or private). Finally, the absence of a clinical evaluation of these symptoms might have led to a wrong estimation of their presence.
The literature in this field is still scarce regarding healthcare workers in a post-pandemic setting. As such, the authors suggest expanding this issue, accounting for risk factors within the population and temporal evaluation of these symptoms.
Conclusions
Consistent with other findings, a comorbid nature between mood disorders, headaches, and TMJD seems to exist. TMJD symptoms seem to be significantly associated with higher depression,
anxiety, and stress levels, whereas headaches appear to be significantly associated with stress alone. Moreover, the pandemic appears to have impacted HCWs, leading to a higher prevalence of these conditions.