Introduction
Establishing and maintaining the apical limit during the root canal preparation is essential for safe and effective instrumentation.1,2The narrowest apical diameter of the canal might be located at 0.5-1 mm from the major foramen and has been established as the landmark to the working length (WL), the ideal point to end the instrumentation and obturation.1 However, establishing the WL with conventional radiographic methods is difficult because of distortions, anatomical variations, and interferences of anatomical structures.3,4
Electronic apex locators (EALs) were introduced in Endodontics with the objective of determining more precisely the WL or the apical constriction of the canal.5 Since their introduction, their working principles have suffered modifications to provide more accurate measurements, and thus, they have gained popularity.5,6 Recent EALs are based on alternating current impedance measurement with the use and processing of two or more different frequencies.5 The Mini Apex Locator (SybronEndo, Glendora, USA) is a compact EAL that operates as a two-frequency-based measurement system emitting an all-digital signal, which results in major precision.7 In turn, the Root ZX mini (J. Morita Corp., Tokyo, Japan) is a modified version of the Root ZX that measures the impedance of two frequencies simultaneously.8,9 This device is compact and has automatic calibration, three programmable memory settings, and shock resistance.10 On the other hand, the Propex II (Dentsply-Maillefer, Ballaigues,
Switzerland), while also using impedance at two diferente frequencies to determine the WL, unlike most EALs, measures the energy of the signal with multi-signal frequencies rather than its amplitude.3
Aiming to facilitate the insertion of instruments into the apical portion of the root canals11,12 and reduce the number of microorganisms that may be pushed to the periapical region,13 cervical dentin projections should be removed during endodontic instrumentation by preflaring. This maneuver can be executed with manual and/or rotary instrumentation techniques with different instruments such as Hedström files, LA Axxess (SybronEndo, Orange, USA), gattes-glidden, or orifice shapers as S1 and Sx ProTaper instruments (Dentsply-Maillefer, Tulsa, USA).13 Studies have shown that preflaring of the canal’s cervical and middle thirds could enhance the tactile sense of the apical constriction. On the other hand, determining the WL without preflaring increased the number of cases where the file could not reach the apical limit of the root canal preparation or surpassed it.13,14 To date, few studies have evaluated the effect of cervical preflaring in EAL measurements, and the results suggest an increase in the accuracy of some devices after preflaring.11,12,15
The fact that pre-cervical enlargement increases the precision of EAL measurements highlights the need for new studies to clarify the role of different enlarged instruments on the precision of some widespread devices.3,7,8,12 Therefore, the objective of this study was to evaluate the influence of preflaring using the LA Axxess and S1 and Sx ProTaper instruments on the accuracy of the following EALs: Root ZX mini, Mini Apex Locator, and Propex II.
Material and methods
After Ethics approval (Protocol #165.374), sample size and power analyses were calculated using G*Power (Heinrich Heine, Universität Düsseldorf, Düsseldorf, Germany) by applying the Wilcoxon-Mann Whitney t-test . Thus, after a radiographic examination, 30 single-rooted mandibular incisor teeth were selected for this study. This sample was separated into two groups of 15 teeth each, the ideal size required, considering the alpha types error of 0.05, beta powers of 0.8, and a ratio of N2/N1 of 1.
The teeth selected showed well-preserved coronal and radicular structures, mature apexes, Vertucci’s type I canal configurations, and no evidence of calcification, resorption, fractures, root canal treatments, or metallic restorations. Tissue and debris were removed from the root surfaces with hand curettes. The teeth were stored in saline solution at 5 °C prior to use.
The incisal edges were flattened using a polishing machine under refrigeration (APL-4; Arotec, Cotia, Brazil) to obtain a stable reference point for the root canal length measurements. The teeth were then numbered, and the cavity was prepared with a #1012 diamond bur (S.S. White Dental Products, Rio de Janeiro, Brazil) at high speed. Debris in the pulp chamber and pulp tissue remnants were removed with a size #10 K-file (Dentsply-Maillefer, Ballaigues, Switzerland) and irrigation with 1% sodium hypochlorite solution (NaOCl) using a disposable plastic syringe attached to a 23-gauge needle.
The root canal length up to the apical foramen was determined by introducing a size #10 K-file into the canals until the instrument’s tip reached the apical foramen. The silicone stop was then adjusted at the incisal edge of the tooth. This procedure was performed with the aid of a stereomicroscope (Carl Zeiss, Jena, Germany) at 50X magnification. The file was removed, and the root canal length (from coronal reference to major apical foramen) was determined with a digital caliper (0.001 mm; Mitutoyo, Suzano, Brazil). All measurements performed during the study were obtained three times, and the resulting mean was recorded as the final result.
The specimens were randomly assigned into two treatment groups, according to the preflaring preparation (n=15) (Figure 1):
- Protocol #1: preflaring with S1 and Sx ProTaper instrument files using the X-Smart electric motor (Dentsply-Maillefer, Ballaigues, Switzerland) at 300 rpm and a torque of 3 N. The S1 instrument was inserted into the canal 3 mm short of the root canal length previously determined. Subsequently, the Sx instrument was used with a brushing motion up to 5 mm short of the root canal length.
- Protocol #2: preflaring with an LA Axxess nº 1 (20/.06) bur at low speed. The LA Axxess was used 5 mm short of the root canal length. Before preflaring procedures, the teeth were immersed in a plastic box containing fresh alginate (Jeltrate II; Dentsply, Petropolis, Brazil) for the electronic measurements of the root canal length.
The lip electrode was immersed in alginate laterally to the tooth. The root canals were irrigated with 1% NaOCl solution, and the excess was removed from the pulp chamber. A K-file sized as large as necessary to apically adapt to each canal was then connected to the other electrode for the electronic measurement and gently inserted into the root canal until “0.0” or ‘‘APEX’’ signals were observed on the LED or display screens of the EALs. The measurement was considered conclusive after the EALs presented 5 s of stability. All the devices measured the entire sample (i.e., both preflaring protocols) electronically. The silicon stop was then carefully adjusted to the reference level, and the distance between the stop and the file tip was determined. After measurements were executed three times, the preflaring preparation was performed for each group as previously described, and the new root canal length measurements were performed with the EALs.
The EALs were classified as accurate if the measurements differed from the apical foramen by ≤ 0.5 mm and inaccurate if they differed by > 0.5 mm or surpassed the root canal length. Differences between the same locator before and after preflaring with the LA Axxess and S1 and Sx ProTaper files were detected by using McNemar´s chi-square test. The Cochran’s Q test was applied to detect differences between all the EAL measurements in the same condition before and after preflaring. The level of significance was set at p<0.05.
Results
Table 1 shows the number of teeth with accurate and inaccurate measurements and the percentage of accurate values for each EAL before and after each preflaring. Cochran’s Q test did not identify significant differences between the EALs’ precision in the same condition, namely before and after each preflaring.
Table 1 Number of canals with accurate (≤0.5 mm) and inaccurate (>0.05 mm) measurements, and percentage (%) of accurate values for each electronic apex locators before and after preflaring with LA-Axxess nº 1 bur and S1 and Sx ProTaper instruments.
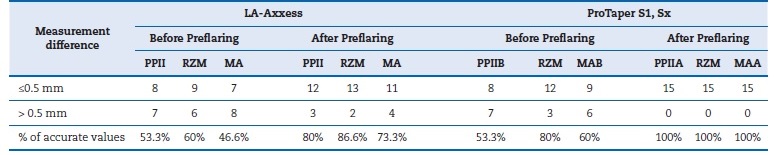
PPII= Propex II; RZM= Root ZX mini; MA= Mini Apex.
McNemar’s chi-square test, p<.05: Different uppercase letters indicate differences between the same locator before and after each type of preflaring.
Cochran’s Q test, p= 0.22.
The preflaring procedure increased the number of precise measurements for all the EALs evaluated. The use of LA Axxess increased the precision of EALs from 53.3% to 80% (PPII), 60% to 86.6% (RZM), and 46.6% to 73.3% (MA), respectively. After using the S1 and Sx ProTaper instruments, none of the devices tested presented inaccurate measurements. The McNemar’s chi-square test identified differences in the Propex II (p=0.01) and Mini Apex Locator (p=0.03) with a significant increase in accuracy after preflaring by the ProTaper. This difference was not found for the Root ZX mini (p=0.25), the EAL that had the greatest number of teeth with accurate measurements for all analyses. No significant differences were found for the LA Axxess (p>0.05).
Discussion
Cervical preflaring is an important procedure advocated to remove dentin interferences in root canal entrances, allowing the file to easily reach the apical constriction.11,13,14 However, because of the small number of studies published, it is still nuclear whether preflared root canals might affect the precision of the EALs and whether the type of EAL has any influence.
In this study, the cervical preflaring with the LA Axxess and ProTaper orifice shapers improved the number of accurate readings of all EALs tested, with statistically significant diferences for the Propex II and Mini Apex Locator after using ProTaper instruments. The Root ZX mini had the greatest number of accurate measurements in all analyses, and no statistical diferences were found in its precision. These increases in correct measurements after preflaring agree with previous studies.11,12,15 One reason for these findings is that files with a larger diameter will fit more tightly in the apex,16 and the metallic surface will be less exposed to the surrounding electrolyte, which allows a more effective impedance reading of this region.8 Another aspect was the better interpretation of the capacitive aspect of the impedance when adjusted files were used.16 Considering the different preflaring protocols, the slightly better results provided by the ProTaper instruments could be attributed to their deeper penetration, facilitated by their composition in NiTi alloy and smaller tips. The endodontic community has been intensively discussing the relationship between the size of coronal access preparation cavities and the amount of excised dentin and fracture strength.17 The same relationship could be considered for cervical dentin, which may be an área of resistance against root canal fractures. Therefore, considering these points, the preflaring protocol with NiTi instruments should be preferred over the use of stainless-steel instruments.
EALs were classified as accurate if the difference between the real measurements and the values obtained by them was ≤ 0.5 mm, which is considered highly precise.7 The percentages of accurate measurements before preflaring were 46.6% - 80% and increased to 73.3%-100% after preflaring, with no statistically significant differences in precision between EALs in the same condition. The adopted tolerance range indicated that after preflaring, the devices analyzed showed high accuracy; thus, the results of this investigation agree with previous studies.12,15,18 In addition, no cases of overextension were observed, which is consistent with the findings of Brito-Júnior.15
The selection of the major foramen (0.0 mm) as the level for the EALs’ accuracy evaluation was based on previous investigations that had excellent results using this landmark and showed that the more distant the file tip was from this reference point, the greater were the differences to the real measurement values.7,16,19 The use of the device has been suggested until the APEX mark or 0.0 mm and then subtracting 1 mm from this measurement to perform the endodontic treatment to prevent overestimation of the WL.3
The experimental models used in ex-vivo research on the accuracy of EALs should simulate the clinical situation, reproducing the impedance values of human tissues.3,20 In the presente study, the teeth were embedded in alginate for the electronic measurements because this protocol provides ease of preparation, offers a high degree of stability and accurate readings, and has been reported as more reliable and reproducible.20
Among the limitations of the present study, clinical observation only with an optical microscope stands out since the alternative microcomputed tomography (Micro-CT) 21 can provide reliable data in three dimensions. This tool reproduces the internal and external anatomy with great detail visualization and would be of great value in confirming the results obtained in this study.
Therefore, new studies based on more reliable analyses, such as Micro-CT, relating the accuracy of EALs to cervical preparation must be proposed.
Conclusions
The results of this study demonstrated a numerical increase in the EALs’ accuracy after the cervical preflaring of single-rooted mandibular incisor teeth, with a statistical difference for the Propex II and Mini Apex Locator when the preflaring was performed with S1 and Sx ProTaper instruments. The EALs tested showed similar accuracy when compared within the same condition.