Introduction
Keratoacanthoma is an epithelial tumor caused by an exacerbated production of keratin. Its clinical, cytological, and histopathological features are very similar to a well-differentiated squamous cell carcinoma (SCC).1 This lesion has a predilection for males, especially those over 45 years old. In 8% of cases, it occurs in the vermilion border of the lips, and 95% occur in areas of the body frequently exposed to the sun. Thus, sun exposure is presumed to play a role in its pathogenesis. However, the etiology of keratoacanthoma is still unclear.1
Clinically, keratoacanthoma appears as a well-defined sessile exophytic nodule with firm consistency, rough surface, and a central area of keratin. It has rapid evolution and spontaneous regression.2 Histologically, it manifests as mature neoplastic cells, abnormal keratin production, and corneal pearls similar to those found in well-differentiated SCC.2
In addition to exposure to unprotected sunlight, studies aiming to elucidate the pathogenesis of this enigmatic tumor have pointed out other causes, such as human papillomavirus (HPV) infection, trauma, previous hypertrophic lichen planus, and the use of BRAF gene inhibitors.3-6
Commonly, keratoacanthoma has three stages of evolution: growth, stabilization, and regression.7 Despite the delimitation of these three phases, the distinction from SCC is rather difficult in all. As a result, as well as to avoid large scars, it is advisable to surgically excise the lesion before spontaneous regression.1
Furthermore, a study reported that keratoacanthoma developed an aggressive behavior in some cases, and in 17.4%, there was a transformation into squamous cell carcinoma in individuals over 70 years old.8 Many authors still support the theory that keratoacanthoma is a malignant tumor - a subtype of SCC, as both are characterized by an abnormal and rapid growth of keratinocytes and have sun exposure as a risk factor.9 Since the histopathological pattern of the lesion presents characteristics similar to those of the SCC, surgical resection is justified because the behavior of the tumor next to the clinically normal epithelium could be more important than the appearance of the cells individually.1
Despite having been described by Sir Jonathan Hutchinson in 1888, keratoacanthoma is currently an enigma in epidemiological, etiological, clinical, histopathological, and prognostic aspects. Moreover, its treatment guidelines are still controversial.4
Keratoacanthoma diagnosis is challenging for health professionals due to the difficulty distinguishing it from SCC. Therefore, the development of scientific works focused on keratoacanthoma diagnosis becomes essential so that, in the future, it can be identified in a precise and safe way. This study aims to contribute to the scientific literature by publishing a case of this epithelial neoplasm and discussing its epidemiological and etiological data, clinical and histopathological characteristics, and treatment.
Case Report
The present case is part of the research project entitled “Clinical-pathological study of the lesions identified at the Reference Center for Oral Lesions (CRLB) of the State University of Feira de Santana (UEFS),” which was submitted to the Committee of Ethics in Research at UEFS and approved by it, registered under protocol number 015/2008, CAAE 0015.0.059.000-08.
A 69-year-old Caucasian male patient attended the Reference Center for Oral Lesions (CRLB) of UEFS, complaining of a darkened lesion on his lower lip with an evolution of approximately four months. He worked as a mason and reported not adopting sun protection measures.
The patient mentioned having previously undergone treatment with a dermatologist through three sessions of acid spray application to desquamate the tumor. As there was no regression or stabilization of the lesion, topical antibiotics and lip sunscreen were prescribed.
During the physical examination, an exophytic growth nodule measuring 10 mm was observed in the lower lip with the following features: well-delimited, circular shape, firm consistency, whitened pink color, and rough surface. The clinical suspicion was SCC.
Soon after the patient’s physical examination, laboratory tests were requested. He underwent an incisional biopsy to remove a small portion of the lesion. The wedge of tissue was carefully removed to include both normal-looking and abnormal- looking tissue and have adequate depth to include cells that characterized the base of the lesion.
The fragment was sent to the Laboratory of Surgical Pathology at UEFS. Microscopy revealed fragments of the oral mucosa lined by hyperparakeratinized stratified squamous epithelium, showing an area of central depression filled with keratin, numerous corneal pearls, pseudoepitheliomatous hyperplasia, and areas of epithelial dysplasia. Thus, it was concluded that the lesion on the patient’s lower lip was a keratoacanthoma. Based on the diagnosis, surgical resection of the lesion was scheduled (Figure 1).
The resection was prepared by an aseptic surgical technique followed by local anesthesia with 2% lidocaine with 1:100,000 epinephrine injected at four points around the lesion without direct infiltration. Afterward, the tissue was incised with a scalpel and number 15 blade. The incision started with a safety margin in healthy tissue at a 90º angle until it reached the connective tissue and was then adjusted to a 45º angle.
Two elliptical-shaped incisions were performed, angled to converge at their base, producing a satisfactory specimen. The fragment was completely removed (Figure 2), stored in a container with a 10% formalin solution in properly identified packaging, and sent for histopathological analysis at the Laboratory of Surgical Pathology at UEFS.
The surgical wound was initially synthesized with a simple internal stitch for tissue stabilization. The external suture began with a simple stitch on the vermilion border of the lips, ensuring the alignment of this aesthetically important muco-cutaneous transition, and continued by completely uniting the edges of the wound (Figure 3).
At the end of the surgery, the patient received guidance on the necessary postoperative care. Toragesic 10 mg was prescribed as a non-steroidal anti-inflammatory drug to be taken sublingually every eight hours for three days to alleviate the symptoms of the typical inflammatory process of healing. Gingilone 10 g was prescribed for topical use in the suture line to control possible infection.
Histopathological analysis of the resected specimen revealed fragments of oral mucosa lined by hyperparakeratinized stratified squamous epithelium, showing an area of central depression filled with keratin, numerous corneal pearls, pseudo-epitheliomatous hyperplasia, and areas of epithelial dysplasia, confirming the diagnosis of keratoacanthoma (Figures 4 and 5).
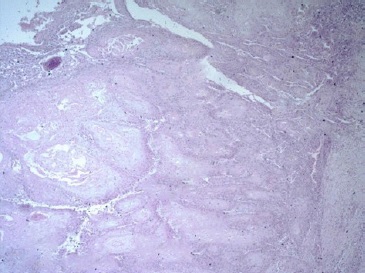
Figure 4 Histopathological section showing intense epithelial proliferation with marked dyskeratosis (keratin production by means of corneal pearls and keratinization of individual cells) (HE, 10X).
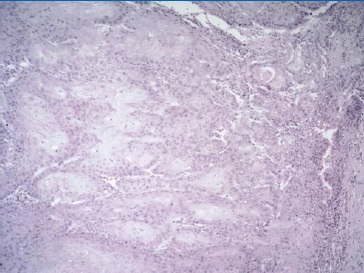
Figure 5 Histopathological section showing pseudoepitheliomatous hyperplasia, excessive production of keratin, and the presence of corneal pearls (HE, 20x).
During the 24-month follow-up, the lesion did not recur, and a discreet scar was formed, as seen in the postoperative images (Figure 6).
Discussion and Conclusions
The dangerous confusion between keratoacanthoma and SCC results from their similar clinical and histopathological characteristics, their similar causal factors, and the lack of a clearcut definition accepted as histological criteria for keratoacanthoma lesions. This situation is considered a critical enigma in pathology.7,10,11
It is routine at the CRLB service to carry out a thorough anamnesis to aid the development of a diagnostic suspicion and subsequent treatment plan. In the anamnesis, the patient revealed he had prolonged sun exposure due to his profession (mason) without using sun protective measures. Moreover, he lived in the outback of Bahia, a region affected by high-intensity ultraviolet radiation. The sun exposure factor is strongly mentioned in the literature as a risk factor for the development of lesions such as keratoacanthoma and SCC.2,9 Furthermore, the patient was male, Caucasian, and over 60 years old when diagnosed, corroborating the demographic data of the population affected by this type of injury already foreseen in the literature.1,2,11
In addition to sun exposure, other factors suggestive of causing these lesions are using BRAF gene inhibitors, tattoos, laser procedures, trauma, and chemical peelings, among others.6 However, none of these other hypotheses for cause fit with the information on the patient’s life history besides excessive exposure to the sun.
Neffa et al.,12 in a retrospective study, analyzed 162 patients diagnosed with keratoacanthoma, of which 56.80% were male, and the mean age was 71.23 years, corroborating the studies by Liang et al.,2 and agreeing with the epidemiological data of the patient in this report. In that study, 55% of keratoacanthoma cases were diagnosed and treated between the eighth and ninth decades of life, which differs from the age of diagnosis in the present case, which was in the sixth decade.
In that research, the face was the second region most affected by the lesion, representing about 27.7% of cases, following only the upper limbs, corresponding to 41.62%. The average size of the lesions was 1.07 cm, which is smaller than those of the lesion mentioned in our case, of approximately 1.80 cm.
One of the points worth mentioning from Neffa et al.’s study12 is that the preoperative diagnoses were wrong in 36.88% of the cases. This relevant number of misdiagnoses demonstrates the difficulty faced by health professionals in accurately diagnosing keratoacanthoma, which confirms the importance of developing studies like this one. In that study, 74 patients were also followed up for two years after surgical resection, and the lesion did not recur in any of the cases. The same happened with the patient in the present case, who has been followed up for 24 months and has not shown recurrence.
The clinical presentation of the case as an exophytic nodule with a firm consistency, sessile base, rough surface, crateriform aspect, and keratotic center reinforces the clinical appearance of keratoacanthoma advocated in the literature.8,11,13-15 Keratoacanthoma may present histopathological characteristics very similar to SCC initial lesions, such as perineural invasion, infiltrative growth, and cellular atypia. Therefore, combining all clinical data to enable a differential diagnosis is extremely important since each type of lesion is treated differently, with SCC being treated much more radically.11 Even with many similarities, there are findings specific to SCC, such as marked abnormal mitotic activity, intense cellular atypia, and deep dermal and subcutaneous invasion, that make it possible to distinguish the histological aspect of keratoacanthoma.13,14
Histological features that favor a diagnosis of keratoacanthoma over SCC include a central keratin-filled crater, which enlarges with the maturation and evolution of the lesion. Another key feature is the lipping (also known as buttressing) of the edges of the lesion, which overlap the central crater, giving it a symmetrical appearance. Trans-epidermal elimination of elastic fibers damaged by sun exposure can also be observed.
Moreover, there is a mixed infiltrate of inflammatory cells in the adjacent dermis, which is sometimes moderately heavy. Eosinophils and neutrophils may be prominent and extend into the epithelial nests to form small microabscesses. There is no stromal desmoplasia except in late involuting lesions.16
The microscopic findings of the lesion in the present case agree with the histopathological characterization of keratoacanthoma, mainly the central depression filled with keratin in an abnormal production.
In order to facilitate the diagnosis of this lesion, many studies focus on seeking alternative means to identify this tumor. One of the methods currently being tested is immunohistochemistry.17-19 A recent systematic review showed that some biomarkers, including CD10, COX-2, and elastic fibers, have a high capability of differentiating between SCC lesions and keratoacanthoma in cases with a difficult diagnosis. IMP-3, P53, and angiotensin II receptor type 1 (AT1R) could also be utilized in this manner; however, more investigation is required.20
The chosen treatment was surgical resection with a small safety margin in order not to compromise the patient’s aesthetics.
Despite about 50% of these lesions undergoing spontaneous involution, this regression can generate atrophic, pigmented, and unsightly scars. On the other hand, resection confirms the diagnosis, as in the present case. Thus, the current literature advocates surgical resection as the first choice for treating keratoacanthoma. 2-4,11,12
Another very successful alternative treatment technique is Mohs micrographic surgery, which consists of removing the lesion in layers and microscopically examining each one during surgery until the specimen is completely removed, preserving tissue and minimizing the surgical defect. Despite being a very refined technique and having a lower recurrence rate, that procedure was not applicable in the case reported because the CRLB service does not have the necessary structure.
Therefore, we opted for resection with a small safety margin, which proved to be quite effective and without harm to the patient.15,21
Surgical wounds on the lips require special management during the suturing phase because, as in the present case, they often involve the lips’ vermilion border, which is an importante transition region between the mucous and cutaneous tissues.
The external suture should start with a simple single stitch in the mucocutaneous line to mark this transition. The closure of the surgical wound in the present case was oriented satisfactorily since a discreet scar was formed.21
Liang et al.2 reported a case of keratoacanthoma located in the upper lip, in which the patient refused surgical resection for fear of scarring after surgery. Because of this, his treatment was performed using photodynamic therapy (PDT), with successful results. Conversely, in our case, the lesion was located in the lower lip, and the patient consented to the decision of surgical resection as the treatment of choice. The therapeutic effect of PDT is still uncertain and controversial. While studies have shown the success of treatment with PDT,2,22,23 others have mentioned the rapid increase in lesion size after the sessions and the eventual need to treat the lesion with surgical resection.24,25
A reliable distinction between keratoacanthoma and SCC would change the management strategies for these lesions to less invasive techniques since, unlike SCC, keratoacanthoma has an excellent prognosis. This change would save the patient from psychological distress and reduce related costs for both the patient and health services.10
Keratoacanthoma affects more males aged over 45 years. Clinically, it appears as a nodule with exophytic growth, firm consistency, a sessile base, and a rough surface. Histopathology is characterized by mature neoplastic cells, a crater filled by excessive keratin production, and corneal pearls. The main etiology is sun exposure without protection. The most recommended treatment is surgical resection.



















