Introduction
Tooth injuries are considered a public health problem due to their high prevalence in children and adolescents.1 A systematic review and meta-analysis study with a sample of 40,194 children and teenagers in Brazil revealed a dental trauma prevalence of 21% in permanent teeth and 35% in primary teeth.2
Globally, its estimated prevalence is 15.2% in permanent dentition and 22.7% in primary dentition, which makes tooth injuries one of the five most frequent dental injuries globally.3
Managing dental trauma is always unique and challenging for caregivers and dentists. It is crucial to initiate emergency management from the moment of injury rather than when the patient initially visits the dentist, as this significantly influences the recovery process.1
Tooth avulsion, a notable occurrence in clinical dentistry, manifests in approximately 0.5-16% of dental trauma incidents.4 Avulsion stands out as a particularly severe dental injury that harms the surrounding periodontal structures.5 Although replantation emerges as the optimal course of action in such cases, it presents significant challenges, notably root resorption.6 The clinical aspects of replantation, periodontal ligament viability, root maturity, the intensity of the inflammatory reaction triggered by avulsion, and the presence of bacteria will determine the prognosis of the replanted tooth.7
Root resorption poses a formidable obstacle primarily due to the total or partial loss of the periodontal ligament, compromising the cementoblast layer and the patient’s inflammatory response.8-10 This occurrence can lead to the development of inflammatory root resorption, ankylosis, replacement root resorption, and even loss of the replanted tooth, adversely affecting the affected individual’s aesthetic, functional, and psychological well-being.11 On the other hand, when an immature tooth does not present any clinical signs, such as color change, root development arrest, fistula, ankylosis, and pain, the tooth may have a good prognosis.6
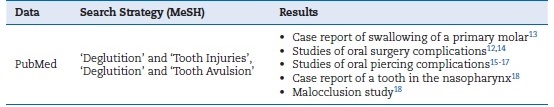
This report aims to present a case involving the avulsion and subsequent replantation of a permanent left maxillary central incisor (tooth 21) that was accidentally swallowed. Two searches were conducted in the National Library of Medicine (PubMed) on February 29, 2024, using the medical subject headings ‘Deglutition’ and ‘Tooth Injuries,’ ‘Deglutition’ and ‘Tooth Avulsion.’ Eight manuscripts were found,12-19 of which none reported a case of tooth replantation after swallowing (Table 1).
These results indicate that this study may represent one of the first case reports documenting permanent tooth avulsion where the tooth was accidentally swallowed and replanted.
Case report
On March 24, 2018, a six-year-and-eight-month-old boy suffered dental trauma during a birthday celebration. The child’s arms became fatigued after reaching the top of a climbing wall, and he gripped the holds with his teeth. At that exact moment, the supervisor pulled the rope to ensure the child’s safety, leading to tooth avulsion and acidental swallowing of his left maxillary central incisor (21).
The patient’s parents contacted their dentist, who advised them to retrieve the tooth by gastrointestinal endoscopy. When the patient reached the hospital, an abdominal X-ray revealed that the tooth was in the stomach, surrounded by food. The potential waiting time for an endoscopy was six hours, risking it being already in the intestine. According to the doctors, rescuing the tooth would be an invasive maneuver with minimal success given the unfavorable conditions.
However, after a six-hour wait, a subsequent abdominal X-ray confirmed that the fecal material had passed into the intestine while the tooth remained lodged in the stomach mucosa. Thus, the doctor and the family agreed to proceed with a gastrointestinal endoscopy to retrieve the tooth (Figure 1).

Figure 1 Upper gastrointestinal endoscopy image (esophagogastroduodenoscopy) showing the tooth lodged in the stomach mucosa.
Gastrointestinal endoscopy was performed under deep sedation with propofol. The tooth was successfully recovered using tweezers and preserved in a saline solution. The patient recovered cognitive function after 15 minutes, and 10 minutes later, he arrived at the private dental office with his parents.
On intraoral examination at the dental office, tooth 21 was missing, and the marginal gingiva was lacerated. On inspection and palpation of the anterior maxillary segment, dentoalveolar fracture was ruled out. The patient had no relevant medical history.
The patient’s parents were informed about a possible poor outcome of the replantation of the avulsed tooth (e.g., root resorption, ankylosis, tooth discoloration, or tooth loss), which had endured an extraoral time of approximately seven hours. Even so, the parents decided to replant the tooth and signed an informed consent.
The avulsed tooth had an intact crown and a two-thirds formed root with a wide-opened apex. The dentist seized the tooth from the saline solution, holding it by the crown and not touching the root surface, and gently rinsed it with 0.12% chlorhexidine. Local anesthesia (2% lidocaine hydrochloride with 1:100000 epinephrine vasoconstrictor) was administered through labial and palatal infiltration in the affected area. The alveolar socket was gently rinsed with saline solution. The avulsed tooth was restored into the socket with slight digital pressure, ensuring its correct position. The replanted tooth was splinted with a 0.4-mm stainless steel orthodontic wire and brackets, placed on the left deciduous canine (63), the right maxillary central incisor (11), and the right deciduous canine (53) (Figure 2). The brackets were fixed away from the gingival tissues and proximal areas after etching the crown surfasse with 37% phosphoric acid for 20 seconds, rinsing with water, air drying, and applying a bonding agent and a composite resin.
The dental apex was wide open, and the crown changed color slightly. The dentist checked the occlusion and prescribed oral anti-inflammatory and antibiotic medications: ibuprofen 100 mg/mL, 20 drops twice daily, and amoxicillin 400 mg/potassium clavulanate 57 mg per 5 mL, twice daily for ten days. Homeopathic remedies were also prescribed: Symphytum CH5 associated with Marigold CH3 30 mL 5% alcohol, eight drops thrice daily for 30 days. The patient had recently received an unnecessary tetanus booster vaccine. He was advised to maintain a soft diet for 15 days and use a soft-bristled toothbrush and 0.12% chlorhexidine mouth rinse twice daily for oral hygiene maintenance.
After one week, periapical radiography revealed the correct positioning of the tooth and a regular aspect of the root surfasse (Figure 3). Fifteen days after replantation, the splint was removed.

Figure 3 Periapical radiograph one week after the trauma, with the left maxillary central incisor (21) showing a regular root surface aspect.
The tooth did not respond to the cold test (1,1,1,2-tetrafluoroethane-Endo Ice). All the other signs and symptoms were normal. Seven weeks after replantation, the color of the tooth crown appeared normal, suggesting potential pulp revascularization despite the negative response to the cold test.
The periapical radiograph revealed no evidence of root resorption or periapical lesion.
After 3 months of follow-up, the tooth presented a slight metallic sound to the percussion test, and the crown’s color was normal. No signs of ankylosis were observed in the periapical radiograph (Figure 4), and the tooth continued non-responsive to the cold test. In the fourth month of follow-up, the tooth exhibited slight mobility, but no other signs or symptoms were observed. Six months after the trauma, a positive response to the sensibility test was verified. After 9 months, the percussion test suggested ankylosis. The color of the tooth remained stable (Figure 5). A cone beam computed tomography (CBCT) suggested a formation of calcified tissue in the root’s apical third (Figure 6). At the 1-year follow-up, a periapical radiograph showed external root resorption in the cervical third of 21 (Figure 7). The patient did not exhibit fistula, gingivitis, pain, or any change in tooth color. The tooth was in infra-occlusion, and the clinical crown was 7 mm long.

Figure 4 Periapical radiograph three months after the trauma showing no signs of ankylosis or root resorption.
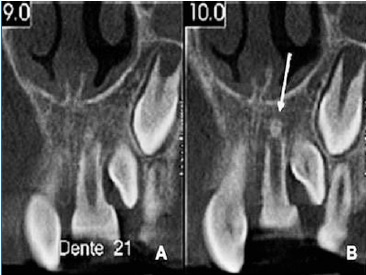
Figure 6 CBCT images 9 months post-replantation. A - Left maxillary central incisor (21). B - Arrow shows calcified tissue in the periapical region of tooth 21.

Figure 7 Periapical radiograph twelve months after the trauma. Left maxillary central incisor (21) showing external root resorption in the cervical third.
Fifteen months after the trauma, maxillary expansion using the Hass appliance was performed to address potential pressure exerted on tooth 21 from the eruption of tooth 22 (maxillary left lateral incisor). The clinical crown was 8 mm long, suggesting a possible spontaneous re-eruption. After 3 months of Hass appliance use, the expected outcome of the maxillary expansion was not attained.
At 18 months of follow-up, the tooth presented an advanced stage of external root resorption (Figure 8). After 21 months since the trauma, a ulotomy was performed for tooth 22 eruption. The periapical radiograph exhibited cervical external root resorption (Figure 9).

Figure 8 Periapical radiograph eighteen months after the trauma. Left maxillary central incisor (21) showing advanced stage of external root resorption.

Figure 9 Periapical radiograph twenty-one months after the trauma. Left maxillary central incisor (21) showing advanced stage of external root resorption.
Twenty-four months after the trauma, there was a pink spot in the cervical third of the crown, indicating the advanced stage of root resorption. Orthodontic brackets were bonded for traction on tooth 22, which was on a collision course with the crown of tooth 21. No bracket was bonded to 21. At 27 months after the trauma, the enamel in the cervical region of 21 was fragile, and the color change was more evident.
Thirty months after the trauma, with a large part of the tooth root resorbed and replaced by bone, the crown of 21 was extracted (Figure 10). Thirty-three months after replantation, an aesthetic-functional tube-bar-type space maintainer was made and installed. Twenty-three months later (four years and eight months after trauma), another aesthetic-functional space maintainer was installed to promote transverse growth of the maxilla, given that the patient was 11 years and 4 months old. Similar to the previous one, this maintainer was secured onto teeth 16 and 26 (right and left maxillary first molars, respectively).
Discussion and conclusions
Tooth avulsion is a severe traumatic injury whose prognosis depends on prompt action following the accident. The preferred treatment is the immediate replantation of the tooth in its socket. Parents, teachers, and general practitioners may need more knowledge for appropriate emergency care after tooth avulsion. Otherwise, replantation might be delayed, carrying an unfavorable prognosis due to extended extra-alveolar time, defined as more than one hour of dry exposure.6,20,21
Replanted tooth management relies on two critical criteria: the stage of root development and the status of the periodontal ligament cells.6,20 The former is crucial because na immature tooth has the potential for pulp revascularization following avulsion and replantation. This process enables the ongoing development of the root, eliminating the need for endodontic treatment.6 The time the tooth spends outside its socket and the medium used to store it influence the viability of periodontal ligament cells, which is crucial for tooth replantation success.6,20 Ideally, the tooth should be repositioned into its socket immediately or within 15 minutes after the accident, maximizing the chances of viable ligament cells and a successful replantation. When immediate replantation is not feasible, transporting the avulsed tooth to the dental emergency service in a liquid storage medium to preserve root surface cells becomes essential.6 The latest guidelines from the International Association of Dental Traumatology (IADT) recommend milk and Hanks’ balanced salt solution, prioritized over water and saliva, as storage media.6 Even when impaired, ligament cells can maintain viability if the tooth is stored appropriately for an extra-alveolar period of less than 60 minutes.6 However, the prognosis becomes unfavorable after 60 minutes of extra-alveolar time, according to the IADT.6
In the present case, an immature tooth was in contact with gastric juice for approximately 6 hours. Acid and digestive enzymes secreted in the stomach impact food softening and nutrient hydrolysis. Namely, pepsin is the main enzyme of the gastric juice components involved in protein digestion, breaking down proteins into smaller peptides and amino acids easily absorbed in the small intestine.22 Consequently, the gastric juice may have dissolved the pulp and periodontal tissue and effectively cleansed the interior of the root canal. Given the widely open apex, this process likely extended to the fibers of the periodontal ligament, leading to protein denaturation and facilitating the removal of necrotic remnants by primary immune cells.
Tooth avulsion results in the rupture of the vascular-nervous bundle, requiring endodontic treatment in some instances. Before recommending endodontic intervention, na evaluation of root development is essential. Immature teeth have more potential for spontaneous pulpal revascularization due to more substantial pulpal-periodontal contact.21
Apical closure may be possible due to the development of new connective tissue.6 Indeed, the apical papilla serves as a reservoir for a distinct type of mesenchymal stem cells, known as stem cells of the apical papilla (SCAPs). These SCAPs play a crucial role in natural root development and might aid in additional root growth.23 The formation of a healthy dentin-pulp complex relies not only on the viability of SCAPs but also on the presence of epithelial cells originating from the Hertwig’s epithelial root sheath (HERS) or its remnants as epithelial cell rests of Malassez (ERM). These cells facilitate crucial interactions between themselves, thus recapitulating the initial stages of tooth development.24 Clinical, radiographic, and histological evidence support the persistence and ongoing ability of the apical papilla and HERS/ERM to differentiate, even after endodontic infection. This evidence demonstrates that a distinct root tip can develop autonomously from the main root, continuing its maturation and eventually reuniting with the coronal portion.25 In the present case, the observed apical mineralization may indicate the survival of SCAPs following the avulsion trauma. This finding holds significant importance in understanding and managing such cases.
Therefore, only immature teeth with clinical or radiographic evidence of pulpal necrosis, such as pain, color change, fistula, or periapical lesion, shall receive endodontic treatment.6 Studies show that immature teeth have a lower risk of developing ankylosis after various periods of dry storage before replantation.5Despite the extra-alveolar time of more than 6 hours and the exposure to gastric acid, replantation was the preferred treatment in the present case. The follow-up revealed positive outcomes, including crown color improvement, fistula absence, and no mobility or pain. The calcified tissue in the apical third of the root observed in the CBCT scan indicated ongoing root development and potential for pulpal revascularization.
As a result, non-endodontic intervention was made despite the lack of pulp response to the cold pulp test. After two years of tooth avulsion and replantation, external cervical resorption was observed, and its rapid progression resulted in tooth extraction.
Various factors may have contributed to the external root resorption and tooth loss, including prolonged extra-alveolar time, exposure of the tooth to gastric acid, and the pressure applied by endoscopic forceps during the tooth’s retrieval from the stomach. External root resorption initiates in the cervical third of the tooth root and can spread throughout the entire tooth in a coronal, apical, or horizontal direction.26,27 The etiology of this type of resorption remains uncertain. One theory suggests that an inflammatory response induced by external pressure can activate clast cells that resorb hard tissue.27 Another theory hypothesizes that endotoxins from microorganisms in the gingival sulcus or dental pulp can stimulate clast cells, causing resorption, combined with other etiological factors.27 Furthermore, the presence of a defect in the enamel/cementum junction, creating a dentin gap, can contribute to resorption progression.26,27 It is worth noting that the cementoenamel junction can exhibit three morphological types. The first and most common is the enamel overlapping the cementum, the second is the enamel and cementum meeting top to top, and the third, which is the least common and less favorable, is when a gap exists between the enamel and cementum, exposing the dentin.28
In the advanced stages of external cervical root resorption, the tooth’s crown exhibits a pink stain due to granulation tissue visible through the damaged dental hard tissue covering the resorption cavity.26,27 Some patients may report gingival bleeding, and upon probing, the granulation tissue may bleed profusely.27 Tooth mobility can also be observed.27 Radiographically, the lesions can be symmetrical or asymmetrical, and their margins can vary from well-defined and smooth to poorly defined and rough or with no clear limits,29 as observed in this case report.
In this case, external replacement root resorption was observed, where cementum and dentin are resorbed and replaced by bone. This phenomenon typically follows a severe injury to the periodontal ligament or the root’s outer surface. It is commonly associated with severe dislocation injuries such as extrusion, intrusion, avulsion, and replantation.
Ligament cells’ necrosis and subsequent tissue loss lead to ankylosis, as the dominant bone healing response occurs. Consequently, the tooth loses the protective influence of the periodontal ligament cells, allowing adjacente bone clastic cells to resorb the dentin. Thus, osteoblasts deposit bone tissue at the site of tooth resorption. The root loses its natural mobility throughout this process, often producing a metallic sound during the percussion examination.
External replacement root resorption ultimately leads to tooth loss.26,30
The main limitation of this clinical case, which at the same time is its uniqueness, is the lack of information about the repercussions of exposing the avulsed tooth to gastric acid before replantation. Both the involved professionals and the child’s parents were aware of this case’s unfavorable prognosis, considering the tooth remained outside the socket for more than one hour. Nevertheless, everyone supported the attempt to save the tooth. Despite the tooth loss, the procedures allowed its maintenance for over two years. It defied the initially unfavorable scenario, temporarily restoring aesthetics and function. It provided valuable time for psychological adaptation for both the patient and parents, facilitating future dental planning and preserving the alveolar bone, contributing to the patient’s unimpeded facial development.
The present study reports an uncommon case of tooth 21 avulsed, accidentally swallowed, retrieved from the stomach, and replanted. Despite tooth loss, the procedures enabled its preservation for over two years. The observed apical mineralization may indicate the survival of SCAPs following the avulsion trauma depicted in this case. This finding holds significant importance in understanding and managing such cases.
The report emphasizes the importance of dental replantation, since it temporarily restores aesthetics and function and gives the patient and parents psychological adaptation time for future dental planning.