Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.10 no.1 Coimbra mar. 2016
CASE REPORT/CASO CLÍNICO
Endometriosis implants after cesarean section: more than a scar - a case report
Implantes de endometriose após cesariana: mais do que uma cicatriz - caso clinico
Patrícia Goulart*, Sílvia Vieira*, Gonçalo Cardoso*, Patrícia Di Martino**, João Mairos***
Hospital das Forças Armadas, Pólo de Lisboa, Portugal
*Interna(o) Complementar de Ginecologia e Obstetrícia
**Assistente Hospitalar de Ginecologia e Obstetrícia
***Diretor de Serviço de Ginecologia e Obstetrícia
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Scar endometriosis after a cesarean section is characterized by the presence of endometrial glands implants at the incision site. It is an uncommon presentation of endometriosis. The diagnosis may be difficult, since it is based in non-specific symptoms, and it can be confused with other surgical conditions.
Case Report: The authors report a case of a 35-year-old woman with a cyclic painful nodule at the left side of a cesarean section scar and no previous history of endometriosis.
Conclusion: Management and preventive measures of this entity are discussed.
Keywords: Endometriosis; Scar; Cesarean section.
Introduction
First described by Rokitansky in 1860, endometriosis is a chronic gynecologic disorder, defined by the presence of functional endometrial tissue outside the uterine cavity1,2 that usually manifests itself with chronic pain or infertility and affects 6 to 10% of women in reproductive age3. Mostly found in the pelvic location, such as the ovaries, posterior cul-de-sac, utero-sacral ligaments, pelvic peritoneum and rectovaginal septum4. Extrapelvic endometriosis is less common, although can affect many sites, such as lungs, appendix, nose, umbilicus, peritoneum or even the intestinal wall. One extrapelvic form of endometriosis is cutaneous endometriosis, mainly in scars following obstetric or gynecologic surgery5,6.
Scar endometriosis after cesarean section is a rare complication, difficult to diagnose and should be considered in evaluation of painful abdominal masses in women4,7.8. It is often mistaken for a suture granuloma, incisional hernia, lipoma, abscess, cyst or a strange body. The symptoms are non-specific, typically described as cyclic abdominal wall pain around the incision site at the time of menstruation9. With an average incidence rate of 0.50% - worldwide rates range from 0,03-3,5%, is probably an underestimated entity5,10.
Case Presentation
A 35-year-old female patient presented with a cyclic painful right inguinal node, with size increase during the menstruation. On retrospective questioning, the patient gave history of menarche at 13 years old, regular cycles, with 4-days menses, associated with dysmenorrhea and premenstrual syndrome. Present contraception with vaginal ring. She had a cesarean delivery for failed induction of labor, two years before. The patient had no previous history of endometriosis.
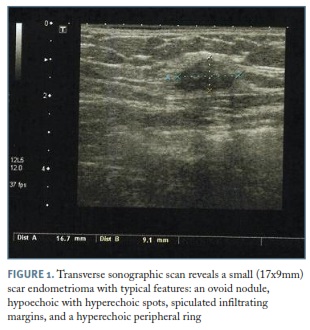
Physical examination revealed a fibrotic nodule on the right side of the cesarean section scar - Pfannenstiel incision, with less than 2cm. All other findings were normal at pelvic observation. Ultrasound of abdominal soft tissues was performed and showed an oval nodule with 17x9mm, suggestive of endometriosis focus (Figure 1).
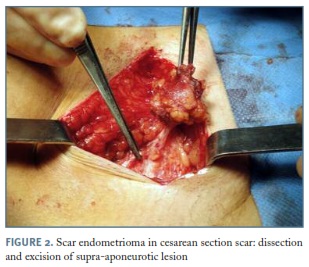
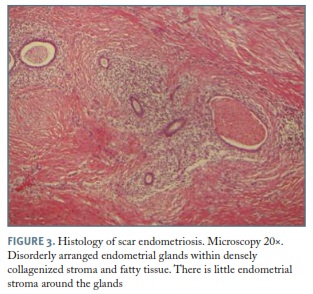
The patient was proposed to surgery and excision of a supra-aponeurotic nodule, with approximately 5x2cm, was performed (Figure 2). The pathological findings showed fragment 6x1,5 cm, variable consistency between elastic and firm, with abundant adipose tissue, recognizing endometrial glands and stroma (Figure 3). Therefore, histopathology of the excised mass had confirmed the scar endometriosis diagnosis. No recurrence was observed after excision in first year follow-up.
Discussion
Scar endometriosis is an unusual phenomenon and should be considered in the differential diagnosis of abdominal wall masses in women. Is commonly confined to the superficial layers of the abdominal wall, although it can also infiltrate deeper layers11,12. The incidence is below 1.0%, nevertheless some authors considerate this entity a non-rare complication of a cesarean section. Furthermore, a higher incidence may be expected if the rate of abdominal delivery increases7,13. These lesions also result from other gynecologic or obstetric procedures, such as, hysterectomy, laparoscopy, amniocentesis, surgery for ectopic pregnancy and episiotomy4,14. The simultaneous occurrence of pelvic endometriosis with scar endometriosis has been reported to be from 14.3% to 26%15,16.
The most likely explanation is iatrogenic transportation of endometrial glands to the wound edge during the procedure. These implants should subsequently be stimulated by estrogen to produce endometriomas in an appropriate hormonal status13,17. In our case report, the patient had a previous cesarean section and no history of endometriosis, which supports the transplantation theory. Early diagnosis is crucial to prevent repair problems during surgery or need of meshes. Detail surgical and gynecological histories, as well as a meticulous examination and appropriate imaging techniques, often lead to the correct diagnosis18.
In the present case, the diagnosis of scar endometriosis was based on a palpable mass on the cesarean section scar, with cyclic pain during menses. Some authors consider this almost pathognomonic15. Differential diagnosis of scar endometriosis may include other surgical conditions like hematoma, incisional hernia, granuloma, abscess, cheloids, lipoma, sebaceous cyst, as well as neoplastic tissue or metastatic carcinoma8,12,16. Ultrasonography is a useful tool and the most commonly used diagnostic procedure to detect this entity in an early stage. Like in this case report, abdominal wall ultrasound usually reveals a solid, hypoechogenic and vascularized nodule, with eventually cyst components of mixed echogenicity. However it is non-specific and the accuracy is reduced in obese patients10,16. Additionally, resonance imaging (MRI), power Doppler ultrasonography may be helpful for accurate determination of the disease extension in the preoperative assessment. The MRI highly specific resolution allows the identification of smaller lesions and better characterization of the relation between those lesions and abdominal wall layers. This approach enables total surgical excision12,13. The use of fine needle aspiration cytology (FNAC) for cytological diagnosis is controversial since it may increase the risk of new endometriosis implants. Likewise, laparoscopic procedures are recommended only for patients with any symptoms that suggests pelvic spread9,10. The definitive diagnosis is made by histology. Endometrial glands, stromal cells, and hemosiderin pigments are usual findings13,16.
For scar endometriosis, total surgical excision is considered to be the gold standard for treatment. Resection must be complete, with at least a 1 cm margin, to prevent recurrence. Larger and deeper lesions are more difficult to excise completely. In these cases, a synthetic mesh placement or tissue transfer for closure, after resection, may be necessary. Surgical excision allows histopathological exclusion of malignancy4,13,16,18.
Previous studies evaluating the use of medical management have shown minimal success. Medical therapy with oral contraceptives, progestagens or gonadotropin-releasing hormone agonists can reduce symptoms temporarily, however recurrence is frequent after therapy discontinuation. Moreover, due to side effects, especially of agonist therapy, compliance is unlikely. Nevertheless, medical treatment may be used for decreasing tumor size and therefore allowing a better surgical outcome in larger lesions. Other possible indications are the situations of relapse or in relation to pelvic endometriosis10,16.
Good technique and proper care during cesarean section may help in preventing endometriosis. Like intraoperative contamination of the surrounding tissue with endometrial cells is a probable cause of scar endometriosis, sweeping the uterus with gauze, during a caesarean delivery, should be limited. Therefore, some authors advocate removing decidual tissue from the wound before closing and irrigated vigorously with normal saline solution, as a prophylactic measure. Other authors have reported continuous use of progestagens in order to decrease the occurrence of endometriosis at the surgical site, during the first six months after hysterotomy. Failure to close the parietal and visceral peritoneum in the cesarean section may be related to greater rates of scar endometrioma. It is recommended not to use the same surgical material and the same instruments as used in hysterorraphy, when suturing other abdominal wall layers. To summarize, we believe that embracing sensible care during the surgical procedures is highly recommendable, even though there are no well-controlled published clinical trials that can strengthen this topic through better evidence4,10,16,19. Furthermore, the highlight of this case is the diagnosis of endometriosis de novo in a woman with no previous history of that disease.
Follow-up of these patients is required, preferable with a gynecologist, due to the high risk of recurrence and, therefore, of re-excision. In case of frequent recurrence, malignant degeneration of the tumor should be excluded. It is rare, occurring in 0.3-1% of scar endometriomas, yet it obligates to a long clinical follow-up in all cases9. The interval between the onset of scar endometriosis and its malignant transformation might vary from a few months to over 40 years. Clear-cell carcinoma is the most common histological subtype, followed by endometrioid carcinoma. Treatment is a radical surgical resection with prosthetic abdominal wall repair. In the literature, 20-month survival rate reaches only 57%20. Hence, compared with endometriosis-associated ovarian carcinoma, the prognosis of abdominal scar complication is poor.
To conclude, with this clinical case we want to emphasize that scar endometriosis, although uncommon, can be a complication of cesarean section. The lack of awareness may represent a major factor explaining why clinicians and radiologists frequently overlook the correct diagnosis. To improve the detection rate of scar endometriosis, more attention to medical history and physical examination is mandatory. For a better understanding of the mechanisms involved, as well as prophylactic measures, further research is necessary given the magnitude of cesarean sections performed.
REFERENCES
1. Brosens I, Benagiano G. Endometriosis, a modern syndrome. The Indian Journal of Medical Research. 2011; 133(6):581-593. [ Links ]
2. Benagiano G, Brosens I. Who identified endometriosis? Fertil Steril. 2011; 95:13-16. [ Links ]
3. Giudice LC, Kao LC. Endometriosis. Lancet 2004; 364: 1789-1799. [ Links ]
4. Adriaanse, B, Natté, R, Hellebrekers, B. Scar endometriosis after a caesarean section: a perhaps underestimated complication. Gynecological Surgery, 2013, 10(4), 279-284. [ Links ]
5. Mascaretti G, Di Berardino C, Mastrocola N, Patacchiola F. Endometriosis: rare localizations in two cases. Clin Exp Obstet Gynecol2007; 34:123-5. [ Links ]
6. Taff L, Jones S. Cesarean scar endometriosis. A report of two cases. J Reprod Med 2002; 47:50-52. [ Links ]
7. Danielpour PJ, Layke JC, Durie N, Glickman LT. Scar endometriosis - a rare cause for a painful scar: A case report and review of the literature. Can J plast Surg 2010;18(1):19-20. [ Links ]
8. Francica G. Reliable clinical and sonographic findings in the diagnosis of abdominal wall endometriosis near cesarean section scar. World Journal of Radiology. 2012;4(4):135-140. [ Links ]
9. Mistrangelo M, Gilbo N, Cassoni P, Micalef S, Faletti R, Miglietta C, Brustia R, Bonnet G, Gregori G, Morino M. Surgical scar endometriosis. Surg Today. 2014; 44: 767-772. [ Links ]
10. Leite G, Carvalho L, Korkes H, Guazzelli T, Kenj G, Viana A. Scar endometrioma following obstetric surgical incisions: retrospective study on 33 cases and review of the literature. São Paulo Med J, 2009:127:270-277. [ Links ]
11. Celik M., Bülbüloglu E., Büyükbese M. A., Cetinkaya A. Abdominal Wall Endometrioma: Localizing in Rectus Abdominus Sheath. Turk J Med Sci. 2004; 34:341-343. [ Links ]
12. Pados G, Tympanidis J, Zafrakas M, Athanatos D, Bontis J. Ultrasound and MR-imaging in preoperative evaluation of two rare cases of scar endometriosis. Cases Journal. 2008; 1:97. [ Links ]
13. Çift, Tayfur. Case Report: Surgical Scar Endometriosis Following Caesarean Section. British Journal of Medicine & Medical Research, 2014, 4(17). [ Links ]
14. Francica G, Scarano F. Delayed diagnosis is associated with changes in the clinical and ultrasound features of subcutaneous endometriosis near cesarean section scars. Journal of Ultrasound. 2009; 12(3): 101-106. [ Links ]
15. A Thapa, A Kumar, S Gupta. Abdominal Wall Endometriosis: Report Of A Case And How Much We Know About It? The Internet Journal of Surgery. 2006 Volume 9 Number 2.
16. Uzunçakmak C, Güldaş A, Özçam H, Dinç K. Scar Endometriosis: A Case Report of This Uncommon Entity and Review of the Literature. Case Reports in Obstetrics and Gynecology. 2013; 2013: 386783.
17. Minaglia S, Mishell D, Ballard C. Incisional endometriomas after Cesarean section: a case series. J Reprod Med. 2007; 52: 630-634. [ Links ]
18. Biswas BK, Gupta N, Magon N. Incisional endometriosis: A rare cause for a painful scar - A report and commentary. Nigerian Medical Journal : Journal of the Nigeria Medical Association. 2012;53(4):257-259 [ Links ]
19. Wasfie T, Gomez E, Seon S, Zado B. Abdominal wall endometrioma after cesarean section: a preventable complication. Int Surg 2002; 87:175-177. [ Links ]
20. Leng J, Lang J, Guo L, Li H, Liu Z. Carcinosarcoma arising from atypical endometriosis in a cesarean section scar. Int J Gynecol Cancer. 2006;16(1):432-435. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Patrícia Goulart
E-mail: patcardoso@gmail.com
Conflict of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Recebido em: 27-05-2015
Aceite para publicação: 18-11-2015