Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.13 no.1 Coimbra mar. 2019
CASE REPORT/CASO CLÍNICO
Pregnancy after endometrial carcinoma: case report and literature review
Gravidez após carcinoma do endométrio: caso clínico e revisão da literatura
Mariana Rei*, Sofia Pedrosa**, Rita Sousa***, Sofia Raposo***, Luís Sá***
Serviço de Ginecologia, Instituto Português de Oncologia Francisco Gentil de Coimbra
*Serviço de Ginecologia e Obstetrícia, Centro Hospitalar Universitário de São João, EPE Porto
**Serviço de Ginecologia e Obstetrícia, Centro Hospitalar do Baixo Vouga, Aveiro
***Serviço de Ginecologia, Instituto Português de Oncologia Francisco Gentil de Coimbra
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Although endometrial cancer is primarily a postmenopausal disease, around 4 percent of patients are younger than 40 years and may desire fertility, requiring conservative treatment options. We describe a clinical case of a 34-year-old nulligesta diagnosed with early stage endometrial carcinoma who achieved a term pregnancy with live birth after conservative fertility sparing treatment with progestins. At two-year follow up, after childbearing and still preserving fertility, she remains in complete remission of the disease. An insight on conservative approaches is provided and potential risks are discussed.
Keywords: Endometrial carcinoma; Pregnancy; Fertility sparing; Conservative treatment; Progestins.
Introduction
Endometrial cancer represents the most common malignancy of the female genital tract in developed countries1. In Europe, the number of newly diagnosed cases exceeded 100,000 in 20121, with a cumulative risk of 1.71%2. Although more than 90% of cases of endometrial cancer occur in women over 50 years, around 4% are younger than 40 years, many of whom may desire to preserve fertility3. Moreover, its incidence may be increasing, due to an important increase of obesity rate and popularity of postpone delivery age4.
Endometrial intra-epithelial neoplasia (EIN), the pre-malignant lesion for type I endometrial carcinoma, encloses a continuum of estrogenic stimulation of the endometrium unopposed by progestins, proliferative glandular epithelial changes and consequently malignant transformation5. The risk factors enhancing this line-up are well known, and most patients typically display a clinical profile comprising high body mass index (BMI) with other components of metabolic syndrome. Other risk factors include unopposed estrogen therapy, estrogen-producing tumors, early menarche, late menopause, nulliparity and infertility, particularly due to polycystic ovarian syndrome, with almost 3-fold increased risk2,6.
Although the majority of endometrial cancers are diagnosed in early stages (80% in FIGO stage I), differences in epidemiological risk factors and histopathological features may impact both treatment and prognosis7.
A large body of evidence addresses the optimal surgical approach of endometrial cancer with hysterectomy and bilateral salpingo-oophorectomy with or without lymphadenectomy. Conservative management in women who desires preservation of fertility raises a therapeutic dilemma that imposes a multidisciplinary discussion and patient involvement.
We aim to review a case of a successful term pregnancy after conservative treatment of an early stage endometrial carcinoma. An insight on fertility sparing treatments and potential risks will be disclosed.
Case Report
We present a case of a 34-year-old nulligesta with the diagnosis of endometrial cancer. Previous medical history included a stable hypothyroidism; pituitary microadenoma controlled with bromocriptine; class II obesity, with a BMI of 37 Kg/m2. Concerning gynecologic history, first menses was at 11 years, with regular cycles and no current hormonal contraception. There was no history of smoking habits. Regarding family oncologic history, her mother had breast cancer at 40 years old.
She presented with uterine abnormal bleeding with a 9-months evolution, referring abundant and prolonged menses as well as intermenstrual bleeding. A pelvic ultrasound revealed a slightly enlarged uterus with heterogeneous endometrial thickening of 17 mm with small regular cystic areas. An hysteroscopy under anesthesia was performed, revealing a large multilobulated polypoid lesion with exuberant vascularization inserted in the fundus of the cavity and right uterine wall. This surgical procedure was finished with polypectomy with complete excision of the lesion. No peri or post-operative complications were registered.
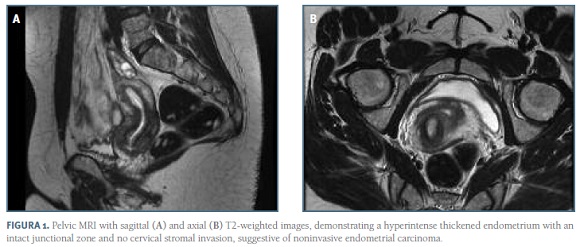
The histology revealed EIN and grade 2 endometrioid adenocarcinoma with estrogen and progesterone receptor positivity. The patient was then referred to our oncologic centre in order to evaluate the need for further treatments. A pelvic magnetic resonance imaging (MRI) was performed, revealing endometrial thickness of 10 mm suggestive of an early stage endometrial neoplasia confined to the endometrium and no cervical stromal invasion - FIGO stage IA (Figure 1A and 1B). Serum tumor markers Ca 125 and HE4 were within the normal range and the cervical cytology was normal. The thoracoabdominal computed tomography (CT) excluded distant dissemination.
After considering the strong desire to preserve fertility and discussing all the pros and cons of a fertility sparing option, the patient engaged with a conservative medical treatment with close follow-up; megestrol acetate (MA) on a single oral dose of 160 mg daily was initiated and maintained for the following 7 months.
At six-months follow-up after initiation of medical treatment, an heterogeneous endometrial thickening of 11 mm was still observed in the pelvic ultrasound. The patient underwent hysteroscopic control under anesthesia, which showed an enlarged cavity with multiple polypoid lesions near the right tubal ostium. Polypectomy of these lesions with bipolar energy system was performed, and the histology was compatible with hyperprogestagenic pseudo-polypoip endometrium and absence of malignancy. As complete remission was confirmed, the progestin was discontinued and conception was encouraged. Three months later she conceived spontaneously, resulting in an uneventful pregnancy with live born term delivery. A male neonate weighing 4400g was born at 39 weeks by cesarian section due to fetal macrosomia. Pathological examination of the placenta revealed no tumor infiltration.
At three-month postpartum consultation, she was asymptomatic with no uterine abnormal bleeding, under oral desogestrel in a daily dose of 0,075 mg. Serum tumor markers and pelvic ultrasound were normal, revealing a linear endometrial contour. Considering that the patient still desired to maintain fertility, a 52 mg levonorgestrel intrauterine device (LNG-IUD) was inserted. At six-month postpartum follow up, clinical, serological and ultrasound evaluation remained normal, and the endometrial biopsy confirmed oncologic remission. Furthermore, counselling regarding risk reduction was provided, particularly focusing on weight loss and nutritional coaching. A close follow-up every six months with tumor markers, ultrasound and serial endometrial biopsies has been maintained in our oncologic centre, and at two-year follow up she remains in complete remission of the disease.
Discussion
The mainstay of treatment for endometrial cancer includes surgical staging, with extrafascial total hysterectomy with bilateral salpingo-oophorectomy without vaginal cuff. Assessment of the nodal status by lymphadenectomy should be performed in intermediate and high risk patients for staging purposes and allows tailoring of adjuvant therapy2,8.
Although this diagnosis is rare in childbearing age women, it may occur in 4% of patients under 40 years old3, imposing the need for fertility preservation strategies. Younger and premenopausal women seem to have a better prognosis, frequently displaying early stage well-differentiated and low-graded tumors, enabling conservative treatment9. Despite of being a highly effective treatment, with five-year survival rates over 95% in this setting, the standard surgical approach results in a permanent loss of reproductive potential, which might be of upmost importance to these women2.
Progestins such as medroxyprogesterone acetate (MPA, 400 - 600 mg/day) and MA (160 - 320 mg/day), have been used as a fertility-sparing approach in this subset of patients, with different dose regimens of cyclic (14 days every month) or continuous therapy successfully used. Other conservative options include local surgical excision with hysteroscopy in one to three steps, with or without subsequent progesterone treatment; recurrent dilation and curettage (D&C); LNG-IUD, frequently in combination with gonadotrophin-releasing hormone agonists10-12. A recent meta-analysis of 54 studies showed that hysteroscopic resection followed by progestogens achieved a higher pooled regression and live birth rate and a lower recurrence rate compared with oral progestogens alone, as well as a significantly higher pooled live birth rate comparing to LNG-IUD alone13. However, there is still no consensus regarding the optimal treatment approach, dose and duration.
A proper assessment of tumor pathological features is a critical issue in patient selection; a conservative approach may be considered in cases of grade 1 endometrial carcinoma histology or premalignant disease as EIN9. Although D&C seems to be the optimal method to obtain the histopathology specimen for diagnosis, reflecting FIGO tumor grade with higher accuracy comparing to office endometrial sampling, hysteroscopy remains the gold standard for an oriented diagnosis14,15.
While conservative management presents high response rates of around 75%, recurrence still occur in 30 to 40% of cases16-18. Therefore, a new D&C and imaging should be performed at 6 months to confirm therapy response. Pregnancy seems to reduce cancer recurrence due to the progesterone environment17 and should be encouraged as soon as remission is achieved and before eventual recurrence. Recent meta-analysis have shown a pooled live birth rate of 28 to 39% after fertility-sparing treatments19,20. Parlakgumus et al retrospectively reviewed nine cases of early stage endometrial carcinoma with desire for fertility preservation; among the 5 patients who preferred medical treatment, there was a case of ovarian carcinoma during the follow-up; one case of cancer recurrence diagnosed on D&C for spontaneous miscarriage; only one reported term pregnancy with live birth20.
We report a case of a 34-year-old women presenting with persistent abnormal uterine bleeding for more than 6 months with relevant risk factors for endometrial cancer, who was diagnosed with grade 2 endometrioid adenocarcinoma after hysteroscopic polypectomy. After six months of medical treatment with daily MA, she achieved complete remission. At this point, if complete response is achieved, conception must be encouraged and referral to a fertility clinic is adequate. In case of no response or disease recurrence after an initial response, standard surgical treatment should be recommended. Furthermore, after childbearing or the age of potencial pregnancy is completed, hysterectomy and eventual salpingo-oophorectomy remains the standard treatment, given the significantly high recurrence rate. Since our patient still desired to maintain fertility in view of a further pregnancy, she will be kept in close monitoring every six month as far as complete remission is warranted.
The subset of younger patients with endometrial carcinoma are frequently nulligravid with a history of infertility, which may raise a therapeutic dilemma. Conservative treatment of endometrial carcinoma seems a safe approach in selected cases of early stages and low grade endometrioid histology. Although many studies have revealed its safety in this subset of patients, there is still no standard treatment algorithm. Patients who desire fertility-sparing options or ovarian preservation should be counseled of the pros and cons and accept close follow-up, regarding the high potential for recurrence and coexisting synchronous ovarian malignancy20.
REFERÊNCIAS BIBLIOGRÁFICAS
1. Ferlay J, Soerjomataram I, Ervik M, et al; International Agency for Research on Cancer. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. globocan.iarc.fr. Accessed April 15, 2017. [ Links ]
2. Colombo N, Creutzberg C, Amant F, et al. ESMO-ESGO-ESTRO Endometrial Consensus Conference Working Group. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: diagnosis, treatment and follow-up. Ann Oncol 2016; 27(1):16-41. [ Links ]
3. Lee NK, Cheung MK, Shin JY, et al. Prognostic factors for uterine cancer in reproductive-aged women. Obstet Gynecol 2007; 109:655Y662. [ Links ]
4. Wise MR, Jordan V, Lagas A, et al. Obesity and endometrial hyperplasia and cancer in premenopausal women: A systematic review. Am J Obstet Gynecol. 2016 Jun;214(6):689.e1-689.e17.
5. Committee on Gynecologic Practice Society of Gynecologic Oncology, The American College of Obstetricians and Gynecologists and Society of Gynecology Oncology. Committee Opinion Endometrial Intraepithelial Neoplasia. Obstet Gynecol, 2015 (reaffirmed 2017). Number 631, Vol. 125, No. 5. [ Links ]
6. Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014; 20:748Y758. [ Links ]
7. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix and endometrium. Int J Gynecol Obstet 2009; 105(2):103-104 (34). [ Links ]
8. DiSaia PJ, Creasman WT. Adenocarcinoma of the uterus. In: DiSaia PJ, Creasman WT (eds). Clinical Gynecologic Oncology, 5th edn. St. Louis, MO: Mosby, 1997; 134-168. [ Links ]
9. Duska LR, Garrett A, Rueda BR, et al. Endometrial cancer in women 40 years old or younger. Gynecol Oncol. 2001; 83: 388Y393. [ Links ]
10. Perri T, Korach J, Gotlieb WH et al. Prolonged conservative treatment of endometrial cancer patients: More than 1 pregnancy can be achieved. Int J Gynecol Cancer 2011; 21: 72-78. [ Links ]
11. Mazzon I, Corrado G, Masciullo V, et al. Conservative surgical management of stage IA endometrial carcinoma for fertility preservation. Fertil Steril 2010; 93: 1286-1289. [ Links ]
12. Minig L, Franchi D, Boveri S, et al. Progestin intrauterine device and GnRH analogue for uterus-sparing treatment of endometrial precancers and well- differentiated early endometrial carcinoma in young women. Ann Oncol 2011; 22: 643-649. [ Links ]
12. Zhang Q, Qi G, Kanis MJ, et al. Comparison among fertility-sparing therapies for well differentiated early-stage endometrial carcinoma and complex atypical hyperplasia. Oncotarget 2017; 8(34):57642-57653.
13. Rodolakis A, Biliatis I, Morice P, et al. European Society of Gynecological Oncology Task Force for Fertility Preservation: Clinical Recommendations for Fertility-Sparing Management in Young Endometrial Cancer Patients. Int J Gynecol Cancer 2015; 25:1258Y1265.
14. Leitao MM Jr, Kehoe S, Barakat RR, et al. Comparison of D&C and office endometrial biopsy accuracy in patients with FIGO grade 1 endometrial adenocarcinoma. Gynecol Oncol. 2009;113:105Y108.
15. Gallos ID, Yap J, Rajkhowa M, et al. Regression, relapse, and live birth rates with fertility-sparing therapy for endometrial cancer and atypical complex endometrial hyperplasia: a systematic review and metaanalysis. Am J Obstet Gynecol 2012; 207:266. e1Ye12.
16. Park JY, Kim DY, Kim JH, et al. Long-term oncologic outcomes after fertility-sparing management using oral progestin for young women with endometrial cancer (KGOG 2002). Eur J Cancer 2013; 49:868Y874.
17. Erkanli S, Ayhan A. Fertility-sparing therapy in young women with endometrial cancer: 2010 update. Int J Gynecol Cancer 2010; 20:1170Y1187.
18. Koskas M, Uzan J, Luton D, et al. Prognostic factors of oncologic and reproductive outcomes in fertility- sparing management of endometrial atypical hyperplasia and adenocarcinoma: systematic review and meta- analysis. Fertil Steril. 2014;101:785Y794.
19. Parlakgumus HA, Kilicdag EB, Simsek E, et al. Fertility outcomes of patients with early stage endometrial carcinoma. J Obstet Gynaecol Res 2014; 40:102-108.
Endereço para correspondência | Dirección para correspondencia | Correspondence
Mariana Rei
E-mail: marianarei@hotmail.com
Recebido em: 03/06/2018
Aceite para publicação: 10/07/2018