Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.14 no.1 Coimbra mar. 2020
ORIGINAL STUDY/ESTUDO ORIGINAL
Early-stage cervical cancer in reproductive-aged women: 10 years of experience of a tertiary care center
Cancro do colo do útero em estadio inicial em idade reprodutiva: 10 anos de experiência de um centro terciário
Leonor Bivar1*, Vera Trocado2,3,4*, Daniel Fernandes5, Vanda Patrício6, Almerinda Petiz7
Instituto Português de Oncologia Francisco Gentil do Porto
* Both authors contributed equally to this manuscript
1 Interna de Formação Específica em Ginecologia e Obstetrícia. Serviço de Ginecologia e Obstetrícia, Hospital de Braga, Braga, Portugal
2 Interna de Formação Específica em Ginecologia e Obstetrícia. Serviço de Ginecologia e Obstetrícia, Unidade Local de Saúde do Alto Minho, Viana do Castelo, Portugal
3 Instituto de Ciências da Vida e da Saúde (ICVS), Escola de Medicina da Universidade do Minho, Braga, Portugal
4 Instituto de Investigação em Ciências da Vida e da Saúde/3B’s - Laboratório Associado do Governo Português, Braga/ Guimarães, Portugal
5 Assistente Hospitalar Graduado. Serviço de Ginecologia, Instituto Português de Oncologia Francisco Gentil - Porto (IPO-PORTO), Portugal
6 Assistente Hospitalar. Serviço de Ginecologia, Instituto Português de Oncologia Francisco Gentil - Porto (IPO-PORTO), Portugal
7 Diretor de Serviço. Serviço de Ginecologia, Instituto Português de Oncologia Francisco Gentil - Porto (IPO-PORTO), Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Overview and aims: Early-stage cervical cancer has a good prognosis, with survival rates at 5 years >90%. However, while offering the potential for disease cure, treatment often results in the loss of future fertility or impacts the ovarian function.
The aim of this study is to examine the characteristics, treatment and survival outcomes of reproductive-aged women with early-stage cervical cancer at a tertiary care center over a period of 10 years.
Study design, Population and Methods: Data from patients with early stage cervical cancer (< stage IB1< 2cm) aged 40 years and younger treated between 2008 and 2017 at that institute were collected. Variables selected included patient demographics, tumor information, treatment types, obstetrical outcomes and survival outcomes. Descriptive analysis and a binary logistic regression model were performed using SPSS v. 23.0.
Results: In 2008-2017 period, a total of 75 women with stage IA1IB1 (< 2 cm) cervical cancer and ≤40 years at diagnosis were treated. Sixty five percent (49) were squamous carcinomas and 29% (22) adenocarcinomas. Surgical treatment was the first-line option for all patients: 8% (6) cervical conization, 7% (5) trachelectomy with pelvic laparoscopic lymphadenectomy, 21% (16) simple extrafascial hysterectomy and 64% (48) radical hysterectomy. Overall, irrespective of the type of surgical treatment, 75% (56) had conservation of ovaries. In a multivariable analysis, squamous cell carcinoma histology was a predictor of ovarian conservation (adjusted OR 11.03, 95% CI 2.66-45,61, p 0.001) on radical hysterectomy. Three of the patients submitted to trachelectomy got pregnant, one of which had a preterm delivery. Recurrence of the disease was reported in 4% (3) of the cases, only one case of mortality was disease-related.
Conclusions: Despite the small case series, our study found a high proportion of reproductive-aged women with early-stage cervical cancer submitted to ovary-sparing surgical treatment, with promising results concerning to recurrence, mortality and pregnancy rates.
Keywords: Early stage cervical cancer; Reproductive-aged women; Trachelectomy.
Introduction
Worldwide, cervical cancer is the fourth most common cancer affecting females, after breast, colorectal and lung cancer1. In developed countries, over the last years, cervical cancer mortality has shown a decreasing rate, in parallel with the decrease in incidence, due to the compliance to organized screening programs2.
In fact, nearly 46% of women with cervical cancer are diagnosed at an early stage and more than 40% of women with early stages are affected during reproductive age3,4.
Early-stage cervical cancer has a good prognosis, with survival rates at 5 years of 95% for stage IA and 90% for IB. However, while offering the potential for disease cure, treatment often results in the loss of future fertility. Thus, treatment of cervical cancer at reproductive ages is a major challenge regarding the preservation of the reproductive function and the ovarian function4.
In 2017, the staging system for cervical cancer was revised by The International Federation of Gynecology and Obstetrics (FIGO). Major changes were that for stage IB disease, sub-stage increases with every 2 cm in tumor size: stage IB1 (<2 cm), stage IB2 disease (2-3.9 cm), and stage IB3 (≥4 cm). Early stages are therefore considered ≤ IB11.
The options for surgical treatment in early stages are total hysterectomy, radical hysterectomy and fertility-sparing procedures including conization or radical abdominal, vaginal, or laparoscopic trachelectomy with pelvic lymphadenectomy1.
In patients who don’t want to preserve fertility, conservation of the ovaries, may protect them from climacteric symptoms, which often seriously impairs their quality of life, and from menopause-related long-term complications such as osteoporosis and cardiovascular disease5,6.
However, the need for further radiation therapy can cause ovarian damage through a reduction in the primordial follicle pool. Therefore, it makes sense to perform an ovarian transposition at the time of the main procedure, taking the ovaries out of the pelvic irradiation field7,8.
The aim of this retrospective observational study is to examine the characteristics, treatment and survival outcomes of reproductive-aged women with early-stage cervical cancer at a tertiary care center over a period of 10 years.
Methods
Retrospective data collection was performed after approval from the institutional review board at a tertiary care center. Data from patients with early stage cervical cancer (stage IB1< 2cm) aged 40 years and younger treated between 2008 and 2017 at that institute were collected.
Variables selected included patient demographics, tumor information, treatment types, obstetrical outcomes and survival outcomes. Patient demographics included age, year at diagnosis and obstetrical history. Tumor information included cancer stage, histologic subtype, tumor size, and lymphovascular space involvement. Treatment types included surgical treatment (conization, trachelectomy, total hysterectomy or radical hysterectomy, along or not with lymphadenectomy and ovary transposition) and postoperative treatment (radiotherapy and chemotherapy). Obstetrical outcomes included attempted pregnancy and its result. Survival information included disease-specific survival and overall survival.
Patients, tumor and treatment characteristics were summarized by count and percentage or median, minimum, and maximum as appropriate. A binary logistic regression model was used to determine independent factors associated with ovary conservation at radical hysterectomy, and the magnitude of statistical significance was expressed as an adjusted odds ratio (AOR) with 95% confidence interval. Statistical analysis was performed using SPSS v. 23.0. P<0.05 was considered statistically significant.
Results
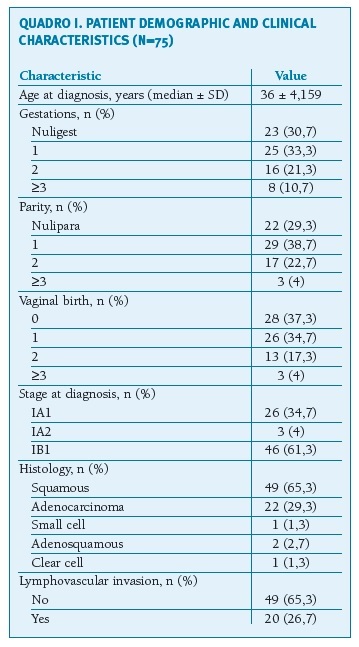
In 2008-2017 period, a total of 75 women with stage IA1IB1 (< 2 cm) cervical cancer and ≤40 years at the time of diagnosis were treated. Demographic and clinical characteristics are summarized in Table I.
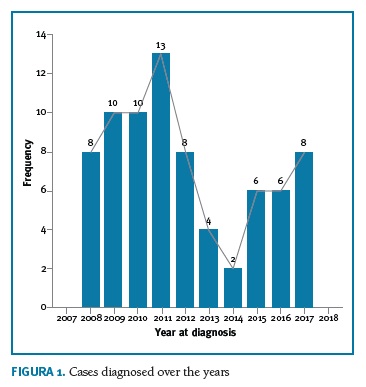
Sixty five percent (49) of the cases were diagnosed in the first 5 years of the study, with a reduction of 47% of the number of diagnosed cases of early cervical cancer in reproductive age women in the subsequent 5 years (Figure 1).
The median age at diagnosis was 36 years, with 63% (47) of the patients in the group 35-40 years. There were no statistically significant differences in the average age of diagnosis in the first and second 5 years of the study (35.06 vs 34.81; p=0.794).
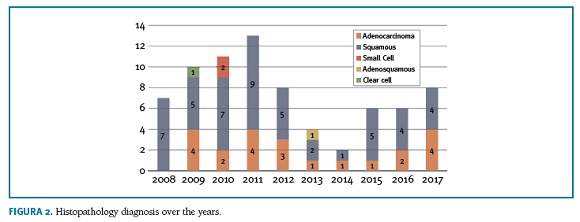
With respect to obstetrical history, 29.3% (22) were nullipara and 26.7% (20) with ≥ 2 deliveries. Sixty five percent (49) were squamous carcinomas, 29% (22) adenocarcinomas and 5% (4) of other histopathologic types (adenosquamous carcinoma (2), clear cell adenocarcinoma (1), small cell carcinoma (1)). From 2008 to 2017, there was an increase in the proportion of cases of adenocarcinoma of the cervix among women ≤ 40 years, with 26.5% in 2008-2012 and 35% in 2013-2017 period. Most of the cases (61%) were diagnosis at stage IB1 (Figure 2).
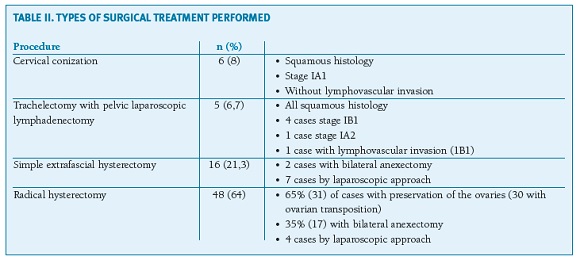
Surgical treatment was the first-line option for all the patients: 8% (6) cases of cervical conization, 7% (5) vaginal trachelectomy with pelvic laparoscopic lymphadenectomy, 21% (16) simple extrafascial hysterectomy and 64% (48) radical hysterectomy (Table II).
Overall, irrespective of the type of surgical treatment, 75% (56) had conservation of ovaries and 25% (19) had not. Ovary-sparing surgical treatment was performed in 45% (10) of cases with adenocarcinoma histology, 83% (24) of stage IA and 70% (32) of stage IB1 disease.
The cases of cervical conization were all squamous histology, stage IA1, without lymphovascular invasion. Two of them had term vaginal deliveries after the procedure, and 1 is pregnant at the time of the investigation. No cases of evidence of recurrence of the disease were detected.
Vaginal trachelectomy with pelvic laparoscopic lymphadenectomy was the selected procedure in 5 cases. Four cases were stage IB1 tumors and 1 case was stage IA2; all squamous cell carcinoma and 1 with lymphovascular invasion. There was one infected lymphocele, drained by radiologic-guided puncture. All of them had no evidence of recurrence of the disease. Three women got pregnant, one of which had a preterm delivery, another a cesarean section at term of pregnancy and one has, at the time of the investigation, a multiple spontaneous pregnancy in the second trimester.
Simple extrafascial hysterectomy was performed in 16 cases, 2 of them with bilateral salpingo-oophorectomy, and 7 by laparoscopic approach. Radical hysterectomy with pelvic lymphadenectomy was performed in 48 cases, 65% (31) with preservation of the ovaries (30 with ovarian transposition) and 35% (17) with bilateral salpingo-oophorectomy. Four cases were performed by laparoscopic approach in the last 2 years of the study. Morbidity was reported in 2 cases: ligation of the right ureter and lymphocele above the external iliac vessels.
In a multivariable analysis of factors associated with ovarian conservation on radical hysterectomy, among the histologic subtypes, those with squamous cell carcinoma histology were more likely to have ovarian conservation (adjusted OR 11.03, 95% CI 2.66-45,61, p 0.001) compared with non-squamous subtypes, after adjusting for other confounding factors such as patient age, year of diagnosis and FIGO staging.
Twelve patients had done adjuvant treatment: 5 radiotherapy, 3 radiotherapy plus brachytherapy and 4 chemoradiotherapy.
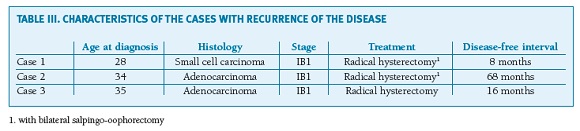
Recurrence of the disease and survival outcomes were analyzed in 74 cases, as one of the cases was lost in follow-up (on average 5 years). Recurrence was reported in 4% (3) of the cases, 2 adenocarcinomas and a small cell carcinoma, submitted to radical hysterectomy, 2 of them with bilateral salpingo-oophorectomy (Table III). There was one case of mortality related to the disease (small cell carcinoma), and another related to alcohol abuse.
Discussion
In this study, the number of cases of early cervical cancer was lower in the second half of the study, according to the trend to reduce the incidence of cases in developed countries, probably due to the implementation of organized screening programs.
Moreover, we found a slightly higher proportion of adenocarcinoma histology than the described in the literature (29% vs 15-25%) and a mild tendency to increase the proportion of adenocarcinoma histology over the years9. As well described, in developed countries, an increase in the proportion of adenocarcinoma in the last years is probably not only a consequence of the reduction of epidermoid carcinomas as a result of screening programs, but also due to the greater difficulty in diagnosis of pre-invasive glandular lesions.
Although few trachelectomies were performed in our study, the proportion of women who underwent this procedure is significant (7%), considering some large studies reporting rates of 1.2 - 4.5%10. Previous studies have shown that vaginal trachelectomy is a safe procedure with a a good prognosis for women with stage IA2-IB1 lesions11. A systematic review in 485 women from 29 studies confirmed the safety of trachelectomy, as only 3.8% of women experienced recurrence and 0.4% died after a median follow-up of 31.6 months12. In our population, although the few cases of recurrence and mortality, this procedure seems to be not inferior to hysterectomy. Further studies are needed to compare cause-specific survival and overall survival among young women with early-stage cervical cancer who underwent fertility-sparing procedures or hysterectomy. We also cannot draw conclusions about the obstetric outcome after trachelectomy as it was the treatment in only 5 cases.
Ovarian preservation in young women has many advantages, including reducing the risk of osteoporosis, providing protection against cardiovascular disease and conservation of the reproductive potential, with possible use of surrogacy5. There are also recent population-based studies supporting the association of early oophorectomy and increased mortality13,14. It is now well established that the risk of occult ovarian metastasis is low and conservation of the ovaries is safe in surgical treatment of early-stage cervical cancer15,16.
The rates of ovary-sparing surgery are higher comparing to data found in the literature, with 83% vs 60% for stage IA disease and 70% vs 40% for stage IB disease5,6. Multiple studies report a higher risk of ovarian metastasis with adenocarcinoma histology compared with squamous histology, that may prevent teams to plan an ovary-sparing surgical treatment5. In our study there is also a lower proportion of cases with ovarian conservation (45%) in the subgroup of adenocarcinoma histology, possibly due to the evidence reported by the older studies. Moreover, exploring the factors that may be associated with ovarian conservation on radical hysterectomy, in our study, squamous histology was found a predictor of ovarian conservation, adjusting for other possible confounders. However, more recently many large prospective cohort studies had found that ovarian conservation even in early-stage adenocarcinoma is a safe procedure17,18,5,19.
Ovarian transposition is now established as a simple procedure with very low rates of morbidity. A recent systematic review showed that ovarian transposition is highly associated with preservation of ovarian function, and with a low risk of metastases in the transposed ovaries7,8. In this study, ovarian transposition was performed in almost all cases (30) of radical hysterectomy with conservation of the ovaries, although data was lacking about the function of the transposed ovaries.
In this retrospective study, laparoscopic approach was used in 8% of the cases of radical hysterectomy. This is a procedure with a very steep learning curve, and a recently published prospective randomized trial caused some entropy in the field, as it demonstrated that this minimal invasive approach was associated with worse outcomes, as lower rates of overall survival and disease-free survival, comparative to open abdominal radical hysterectomy20. Two other recent reports came to question the therapeutic equivalency of minimal invasive vs open approaches21,22. As the size of the tumor is an important factor in the outcome of these procedures, the new FIGO 2018 staging system of uterine cervix support and complement these results, as survival was evaluated in FIGO stage IB1 (<4cm), but without applying the new 2018 FIGO staging system (IB1 - <2 cm)23. Further studies restricting the size of the tumors, considering this new staging system, may have different results. Probably safe selection of the best candidates to minimal invasive approach, based on the presence or absence of risk factors, may help to overcome this question. For now, based on the actual evidence, the European Society of Gynaecological Oncology (ESGO) issued a statement reinforcing that “open approach is the gold standard”24.
Despite the small case series, our study found a high proportion of reproductive-aged women with early-stage cervical cancer submitted to ovary-sparing surgical treatment, with promising results concerning to recurrence, mortality and pregnancy rates. These rates were, as expected, very low in this study, which prevents us to do a survival analysis comparing different surgical types.
REFERENCES
1. Bhatla N, Denny L. FIGO Cancer Report 2018. Int J Gynecol Obstet. 2018;143:2-3. DOI: 10.1002/ijgo.12608. [ Links ]
2. Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. Lancet. 2019;393(10167):169-182. DOI: 10.1016/S0140-6736(18)32470-X. [ Links ]
3. American Cancer Society. Cancer Facts & Figures 2018.; 2018. https://www.cancer.org/content/dam/cancer-org/research/ cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/ cancer-facts-and-figures-2018.pdf. Accessed January 28, 2019.
4. Marth C, Landoni F, Mahner S, Mccormack M, Gonzalez-Martin A, Colombo & N. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up . Ann Oncol. 2017;28:72-83. DOI: 10.1093/annonc/mdx220. [ Links ]
5. Matsuo K, Machida H, Shoupe D, et al. Ovarian Conservation and Overall Survival in Young Women With Early-Stage Cervical Cancer. Obstet Gynecol. 2017;129(1):139-151. DOI: 10.1097/AOG.0000000000001754. [ Links ]
6. Matsuo K, Shimada M, Mikami M. Ovarian conservation for young women with clinical stage IB-IIB cervical cancer in Japan. J Gynecol Oncol. 2017;28(4):e60. DOI: 10.3802/jgo.2017.28.e60. [ Links ]
7. Pahisa j, Martínez-román S, Martínez-zamora MA, et al. Laparoscopic ovarian transposition in patients with early cervical cancer. Int J Gynecol Cancer. 2008;18(3):584-589. DOI: 10.1111/j.1525-1438.2007.01054.x. [ Links ]
8. Gubbala K, Laios A, Gallos I, Pathiraja P, Haldar K, Ind T. Outcomes of ovarian transposition in gynaecological cancers; a systematic review and meta-analysis. J Ovarian Res. 2014;7:69. DOI: 10.1186/1757-2215-7-69. [ Links ]
9. Petignat P, Roy M. Diagnosis and management of cervical cancer. BMJ. 2007;335(7623):765-768. DOI: 10.1136/bmj.39337.615197.80. [ Links ]
10. Machida H, Mandelbaum RS, Mikami M, et al. Characteristics and outcomes of reproductive-aged women with early-stage cervical cancer: trachelectomy vs hysterectomy. Am J Obstet Gynecol. 2018;219(5):461.e1-461.e18. DOI: 10.1016/j.ajog.2018.08.020. [ Links ]
11. Bentivegna E, Gouy S, Maulard A, Chargari C, Leary A, Morice P. Oncological outcomes after fertility-sparing surgery for cervical cancer: a systematic review. Lancet Oncol. 2016;17(6):e240-e253. DOI: 10.1016/S1470-2045(16)30032-8. [ Links ]
12. Pareja R, Rendón GJ, Sanz-Lomana CM, Monzón O, Ramirez PT. Surgical, oncological, and obstetrical outcomes after abdominal radical trachelectomy - A systematic literature review. Gynecol Oncol. 2013;131(1):77-82. DOI: 10.1016/j.ygyno.2013.06.010. [ Links ]
13. Rocca WA, Grossardt BR, de Andrade M, Malkasian GD, Melton LJ. Survival patterns after oophorectomy in premenopausal women: a population-based cohort study. Lancet Oncol. 2006;7(10):821-828. DOI: 10.1016/S1470-2045(06)70869-5. [ Links ]
14. Parker WH, Feskanich D, Broder MS, et al. Long-Term Mortality Associated With Oophorectomy Compared With Ovarian Conservation in the Nursesʼ Health Study. Obstet Gynecol. 2013;121(4):709-716. DOI: 10.1097/AOG.0b013e3182864350. [ Links ]
15. Shimada M, Kigawa J, Nishimura R, et al. Ovarian metastasis in carcinoma of the uterine cervix. Gynecol Oncol. 2006;101(2):234-237. DOI: 10.1016/j.ygyno.2005.10.004. [ Links ]
16. Landoni F, Zanagnolo V, Lovato-Diaz L, et al. Ovarian metastases in early-stage cervical cancer (IA2-IIA): a multicenter retrospective study of 1965 patients (a Cooperative Task Force study). Int J Gynecol Cancer. 2007;17(3):623-628. DOI: 10.1111/j.1525-1438.2006.00854.x. [ Links ]
17. Touhami O, Plante M, Plante M, Marie P. Should ovaries be removed or not in (early-stage) adenocarcinoma of the uterine cervix: A review. Gynecol Oncol. 2015;136(2):384-388. DOI: 10.1016/j.ygyno.2014.12.011. [ Links ]
18. Jiao X-B, Hu J, Zhu L-R. The Safety of Ovarian Preservation in Early-Stage Adenocarcinoma Compared With Squamous Cell Carcinoma of Uterine Cervix. Int J Gynecol Cancer. 2016;26(8): 1510-1514. DOI: 10.1097/IGC.0000000000000780. [ Links ]
19. Hu T, Wu L, Xing H, et al. Development of Criteria for Ovarian Preservation in Cervical Cancer Patients Treated with Radical Surgery With or Without Neoadjuvant Chemotherapy: A Multicenter Retrospective Study and Meta-analysis. Ann Surg Oncol. 2013;20(3):881-890. DOI: 10.1245/s10434-012-2632-8. [ Links ]
20. Ramirez PT, Frumovitz M, Pareja R, et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N Engl J Med. 2018;379(20):1895-1904. DOI: 10.1056/NEJMoa1806395. [ Links ]
21. Melamed A, Margul DJ, Chen L, et al. Survival after Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. N Engl J Med. 2018;379(20):1905-1914. DOI: 10.1056/NEJMoa1804923. [ Links ]
22. Margul DJ, Yang J, Seagle BL, Kocherginsky M, Shahabi S. Outcomes and costs of open, robotic, and laparoscopic radical hysterectomy for stage IB1 cervical cancer. J Clin Oncol. 2018;36(15_suppl):5502-5502. DOI: 10.1200/JCO.2018.36.15_suppl.5502. [ Links ]
23. Matsuo K, Machida H, Mandelbaum RS, Konishi I, Mikami M. Validation of the 2018 FIGO cervical cancer staging system. Gynecol Oncol. 2019;152(1):87-93. DOI: 10.1016/j.ygyno.2018.10.026. [ Links ]
24. Querleu D, Cibula D, Concin N, et al. Laparoscopic radical hysterectomy: A European Society of Gynaecological Oncology (ESGO) statement. Int J Gynecol Cancer. 2020;30(1):15. DOI: 10.1136/ijgc-2019-000775. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Leonor Bivar
E-Mail: leonorbivar@gmail.com
Recebido em: 09/12/2019
Aceite para publicação: 09/02/2020