Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Obstétrica e Ginecológica Portuguesa
versão impressa ISSN 1646-5830
Acta Obstet Ginecol Port vol.14 no.1 Coimbra mar. 2020
CASE REPORT/ CASO CLÍNICO
Solitary fibrous tumor of the uterine cervix - about a case
Tumor fibroso solitário do colo do útero - a propósito de um caso
Márcia Marinho1, Ana Maçães2, Evelin Pinto2, Elisa Paredes3, João Gonçalves3
Centro Hospitalar Gaia/Espinho
1 Interna de Formação Específica de Ginecologia e Obstetrícia, Serviço de Ginecologia/obstetrícia, Centro Hospitalar GaiaEspinho
2 Assistente Hospitalar, Serviço de Ginecologia e Obstetrícia, Centro Hospitalar GaiaEspinho
3 Assistente Hospitalar Graduado, Serviço de Ginecologia e Obstetrícia, Centro Hospitalar GaiaEspinho
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Solitary fibrous tumors are rare mesenchymal neoplasms. Although first reported in the pleura, they were described at extrapeural sites, but they are uncommon in the female genital tract (less than 30 cases reported).
We present a case of solitary fibrous tumor arising from uterine cervix with a benign course, as well as its histopathological and immunohistochemical features that helped establishing the diagnosis.
Keywords: Solitary fibrous tumor; Female; Genital neoplasms; Uterine cervix.
Introduction
Solitary fibrous tumors (SFTs) are uncommon mesenchymal neoplasms with an incidence rate of 2.8 per 100.0001.
Although originally reported for the first time in 1931 by Klemperer and Rabin in the pleura, extra pleural locations of these tumors have been described all over the years2. Nevertheless, their occurrence in the female genital tract is extremely rare (about 30 cases described in the literature)1,3.
In the past, STF have been given many different names including benign mesothelioma, localized mesothelioma, solitary fibrous mesothelioma and localized fibrous tumor4. Fortunately, the World Health Organization (WHO) classification of soft tissue sarcomas published in 2013, helped further differentiation within the sarcomas. As so, SFT are classified as fibroblastic/myofibroblastic tumors and sub classified as intermediate behavior (rarely metastasizing)5.
Due to the low incidence of STF, most data is provided by small series and case reports which made diagnostic and treatment strategies more difficult to stablish4.
We report one of the single cases described in the literature about STF of the uterine cervix.
An informed consent was obtained from the patient and approved by the Hospital Ethics Committee.
Case report
A 68-year-old, G3P2 white woman was referred to our institution for abnormal cervical cytology (ASC-US, atypical squamous cells of undetermined significance).
The patient had a history of hypertension, diabetes, hypercholesterolemia and an orthopedic hand prosthesis (due to traumatic amputation).
She denied any kind of abdominopelvic discomfort, dyspareunia, abnormal uterine bleeding or abnormal discharge.
The colposcopy was unsatisfactory due to atrophy and the high risk human papilloma virus (HPV) test was negative.
Physical examination revealed a bulky lesion with 4 cm that was palpable in the posterior surface of the cervix, protruding into the vaginal wall. This accidental lesion detectable during the vaginal touch was not visible neither during speculum examination nor during colposcopy.
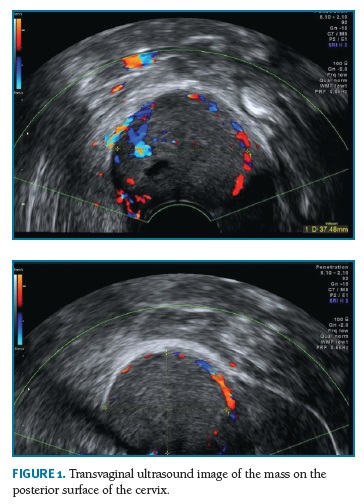
On vaginal ultrasound (Figure 1) a lobed solid lesion was identified, measuring 3.7 x 3.5 x 2.9 cm, with central and peripheral moderated vascularization, localized in the posterior surface of the uterine cervix. The lesion was regular and isoechoic when compared to the myometrium.
Laboratory data was unremarkable.
The pelvic magnetic resonance imaging (MRI) showed a vascularized mass, hyper intense in T2, with 4 x 4.7 cm, from the cervix and protruding into the posterior vaginal wall (Figure 2) .There was no significant additional findings and no evidence of extra-pelvic neoplastic sites nor metastasis.
A biopsy was performed and revealed a mesenchymal tumor without cytological atypia. An immunohistochemical panel analysis was done and showed positivity for CD 34, CD 99 and vimentin; and negativity for estrogen receptors, EMA (epithelial membrane antigen) and desmin. As so, these histological and immunohistochemical features suggested a benign SFT of the uterine cervix.
After discussing the case it was decided to propose a total hysterectomy with bilateral adnexectomy to the patient, which was accepted.
On macroscopic examination of the tumor it was possible to identify a well delimited, elastic mass with 4.5 x 4.4 x3.5 cm. Microscopically, the neoplasm was characterized by spindle cells on a myxoid stroma without cytological atypia and with a low mitotic rate. Hemangiopericytoma-like vessels were also described and the surgical margins were free of tumor.
Currently the patient is being followed-up and continues asymptomatic (13 months after the surgery). Imagological data shows no evidence of disease, neither the physical exam.
Discussion
STF are tumors with a mesenchymal origin, but their etiology is unknown4.
They have an equal gender distribution and may be diagnosed in all ages, although commonly presenting between 20 and 70 years4,6.
These tumors could be found in almost any site of the body, with intra-thoracic being the most common primary location4,7.
On the other side, the most common extra pleural location overall is the abdominopelvic cavity. These tumors generally present with a palpable mass or with local symptoms resulting from compression of adjacent structures due to an enlarging mass. They also could be diagnosed as a coincidental finding on imaging7.
Tumor size at presentation is variable and associated with location, with a range from 1 to 40 cm already been described4.
About 4-10% of STF presents with paraneoplastic syndromes, the most commonly described being non-islet cell hypoglycemia (DoegePotter syndrome) due to hormonal factors like insulin-like growth factors secreted by the tumor cells1,3,4,7.
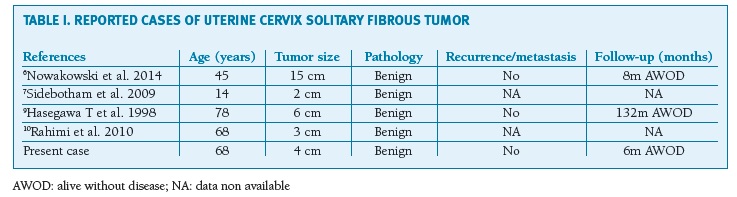
STF is extremely rare in the female reproductive system1,8. Only four cases of STFs in the uterine cervix were described (Table I), none of them malignant6,7,9,10.
(clique para ampliar ! click to enlarge)
When symptomatic, female genital SFT manifestations include abnormal uterine bleeding, flank pain or pelvic fullness8. But, as in our case report, most tumors are asymptomatic and noticed incidentally on imaging or physical examination3.
The diagnosis of SFT is similar to many other soft tissue masses. Contrast enhanced computed tomography (CT) will demonstrate a well-circumscribed, lobulated and hypervascular tumor. T2-weighted MRI typically reveal a well-defined mass that is markedly inhomogeneous with large areas of bright signaling reflecting extensive areas of necrosis4.
Laboratory findings of SFTs are usually unremarkable1.
The differential diagnoses for SFTs of the uterine cervix includes smooth muscle and endometrial stromal neoplasms. They closely mimic leiomyomas which makes the diagnosis harder8,11,12.
The definitive diagnosis is confirmed trough the pathology analysis. STF are composed of spindle to ovoid cells, alternating hypercellular and hypocellular regions with higher percentage of stromal collagen4,8 .
The immunohistochemic panel will show strong positivity for CD34 (present up to 95% of the cases, being one of the most consistent conventional markers) and negativity for EMA, desmin, S-100 protein and actin1,10. Many other markers are variably expressed in SFT such as vimentin, CD99, BCL2 and nuclear â-catenin.
SFT has recently been associated with a NAB2-STAT6 gene fusion product that has proven to be highly specific and sensitive for the tumor4,12.
Due to the paucity of randomized control trials there is no established protocols to guide treatment strategy. As a result, SFT should be approached in a manner similar to other soft tissue sarcomas4.
The standard treatment of localized disease is complete surgical resection with negative margins4,13. Surgical approach in pelvic SFT could be either by laparoscopy or laparotomy depending on tumor location in the female genital tract, size of the tumor and team experience regarding the technique1.
The use of radiation therapy is limited by lack of data. Given the relatively good outcomes and indolent nature of this tumor, radiation therapy is not currently recommended after complete resection with negative margins. The role of adjuvant radiation in cases of positive margins or recurrent tumors has been debated but remains undetermined4.
Since recurrent and metastatic disease are rare, there have been no prospective trials regarding the efficacy of chemotherapy in these settings, and evidence from retrospective analyses has been limited due to small sample sizes. Conventional cytotoxic chemotherapy (multiple regimens described using doxorubicin, ifosfamide, paclitaxel and cisplatin) has modest response rates4,14,15.
The most important biological feature of SFT is its high expression of vascular endothelial growth factor receptor (VEGFR) and platelet-derived growth factor receptor (PDGFR). Several molecular targeted drugs against the signaling pathways of these proteins (as bevacizumab, sorafenib, sunitinib, regorafenib, axitinib and pazopanib) have been reported to show efficacy in SFT treatment. These antiangiogenic drugs could be a promising treatment strategy for SFT4,15.
SFT mostly have an indolent course and benign behavior. But even those tumors considered histologically benign may aggressively recur.
Obtaining adequate negative margins has been shown to decrease the rate local disease recurrence and improve survival (10-year survival rate of 89%). Long-term follow-up in small case series have demonstrated local recurrence as low as 8% after complete resection, however, true recurrence rates may be higher as recurrence has been already reported to occur 17 years following resection4,15,16.
Nevertheless in 10-20% of patients occurs local recurrence or metastasis, with risk factors including positive surgical margins and tumor size greater than 10 cm, as well as malignant features such as more than 4 mitoses per 10 high-power fields, increased nuclear pleomorphism, increased cellularity, and presence of necrosis13,15,17. Some investigators also described older age (≥55 years), paraneoplastic syndrome, and incomplete tumor resection as indicators of poor outcome1,18.
The scarce cases of pelvic SFTs results in absence of a well-defined follow-up protocol. Therefore, close long-term follow-up is recommended with three monthly clinical examination, ultrasound and a yearly cross-sectional MRI or CT scans imaging or as indicated by the clinical symptoms1,3,7,18.
Thus we present a rare tumor with a rarer location, which imposed a clinical challenge, since SFT of the female genital tract has only been subject of a few reports, possibly being under-recognized. It could be easily mistaken with fibroid, but the biopsy performed helped in the differential diagnosis previous to the treatment and also helped planning the surgical approach.
This is the 5th case of SFT of the uterine cervix reported in the literature.
REFERENCES
1. Chen S, Zheng Y, Chen L, Yi Q. A broad ligament solitary fibrous tumor with Doege-Potter syndrome. Medicine (Baltimore). 2018;97(39). DOI: 10.1097/MD.0000000000012564.
2. Klemperer P, Rabin CB. Primary Neoplasms of the pleura. A report of five cases. Am J Ind Med. 1992;22(1):4-31. DOI: 10.1002/ajim.4700220103. [ Links ]
3. Meena M, Jindal T, Duggal R, Gupta A. Solitary fibrous tumor of the ovary. J Obstet Gynaecol Res. 2018;44(6):1177-1180. DOI: 10.1111/jog.13627. [ Links ]
4. Davanzo B, Emerson RE, Lisy M, Koniaris LG, Kays JK. Solitary fibrous tumor. Transl Gastroenterol Hepatol. 2018;3:94-94. DOI: 10.21037/tgh.2018.11.02. [ Links ]
5. Doyle LA. Sarcoma classification: An update based on the 2013 World Health Organization Classification of Tumors of Soft Tissue and Bone: WHO Update of Sarcoma Classification. Cancer. 2014;120(12):1763-1774. DOI: 10.1002/cncr.28657. [ Links ]
6. Nowakowski A, Kozłowski W, Włodarczyk D, Szajnik-Szczepański M, Baranowski W. A case of a large solitary fibrous tumour of the uterine cervix. BMC Womens Health. 2014;14:3. DOI: 10.1186/1472-6874-14-3.
7. Sidebotham EL, DeLair D, Comerci JT, Kayton ML, Abu-Rustum NR. Pediatric radical abdominal trachelectomy for solitary fibrous tumor of the uterine cervix. Gynecol Oncol. 2009;115(2):302-305. DOI: 10.1016/j.ygyno.2009.07.006. [ Links ]
8. Casanova J, Vizcaíno JR, Pinto F, Cunha A, Madureira G. Abdominal mass mimicking a leiomyoma: Malignant uterine solitary fibrous tumor. Gynecol Oncol Case Rep. 2012;2(4):143-145. DOI: 10.1016/j.gynor.2012.09.002. [ Links ]
9. Hasegawa T, Matsuno Y, Shimoda T, Hirohashi S, Hirose T, Sano T. Frequent Expression of bcl-2 Protein in Solitary Fibrous Tumors. Jpn J Clin Oncol. 1998;28(2):86-91. DOI: 10.1093/jjco/28.2.86. [ Links ]
10. Rahimi K, Shaw PA, Chetty R. Solitary fibrous tumor of the uterine cervix. Int J Gynecol Pathol Off J Int Soc Gynecol Pathol. 2010;29(2):189-192. DOI: 10.1097/PGP.0b013e3181b91a6d. [ Links ]
11. Yang EJ, Howitt BE, Fletcher CDM, Nucci MR. Solitary fibrous tumour of the female genital tract: a clinicopathological analysis of 25 cases. Histopathology. 2018;72(5):749-759. DOI: 10.1111/his.13430. [ Links ]
12. Vogels RJC, Vlenterie M, Versleijen-Jonkers YMH, et al. Solitary fibrous tumor - clinicopathologic, immunohistochemical and molecular analysis of 28 cases. Diagn Pathol. 2014;9:224. DOI: 10.1186/s13000-014-0224-6. [ Links ]
13. Demicco EG, Park MS, Araujo DM, et al. Solitary fibrous tumor: a clinicopathological study of 110 cases and proposed risk assessment model. Mod Pathol Off J U S Can Acad Pathol Inc. 2012;25(9):1298-1306. DOI: 10.1038/modpathol.2012.83. [ Links ]
14. Sueblinvong T, Judson PL, Jr LSD, Argenta PA. Solitary Fibrous Tumors Arising From the Female Pelvis. 2011;118(2):5. [ Links ]
15. Ebata T, Shimoi T, Bun S, et al. Efficacy and Safety of Pazopanib for Recurrent or Metastatic Solitary Fibrous Tumor. Oncology. 2018;94(6):340-344. DOI: 10.1159/000486623. [ Links ]
16. Hasegawa T. Extrathoracic solitary fibrous tumors: Their histological variability and potentially aggressive behavior. Hum Pathol. 1999;30(12):1464-1473. DOI: 10.1016/S0046-8177(99)90169-7. [ Links ]
17. Doyle LA, Fletcher CDM. Predicting Behavior of Solitary Fibrous Tumor: Are We Getting Closer to More Accurate Risk Assessment? Ann Surg Oncol. 2013;20(13):4055-4056. DOI: 10.1245/s10434-013-3243-8. [ Links ]
18. Zubor P, Kajo K, Szunyogh N, Galo S, Danko J. A solitary fibrous tumor in the broad ligament of the uterus. Pathol - Res Pract. 2007;203(7):555-560. DOI: 10.1016/j.prp.2007.02.005. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Marcia Marinho
Centro Hospitalar de Vila Nova de Gaia Espinho EPE
Porto, PORTUGAL
E-Mail: marciasilvamarinho@gmail.com
Recebido em: 14/09/2019
Aceite para publicação: 27/02/2020