Introduction
Infertility is a rising problem in our society, with an increasing prevalence in the past years1-3. It affects about 80 million people worldwide, estimating that one out of ten couples is affected by this problem2.
Although numerical translation of infertility is difficult to assess, European studies based on retrospective self-perceived assessments reveal prevalence amid 6,6% and 26.4%3. In Portugal, it is assumed there are between 10% and 15% of couples in this situation, making approximately 500 thousand infertile individuals in our country2.
The probability of pregnancy occurring in each menstrual cycle, called fecundability, is about 20% to 25% for women up to 33-35 years, with an average waiting time of 5 to 6 months1,3,4. After one year, approximately 80-85% of the couples will manage to conceive4. This proportion rises to 90% after two years2. About half of the couples who did not achieve results without contraception after a year will be able to get pregnant spontaneously in the next 36 months. The other half will possibly need medical intervention, as infertility will tend to persist4.
Nowadays we assist a greater demand for treatments due to an increasing awareness and acceptance of infertility by the population4. Besides, improved access to healthcare, diagnostic and treatment techniques have changed the infertility paradigm, allowing a notable growth in this area recently. Actually, 3% to 4% of births registered in Europe are a result of Assisted Reproductive Techniques (ART)3. However, there is still some stigma around the subject considering only half of the women who cannot get pregnant search for medical hel0p1,3.
However, the process inherent to infertility can be psychologically stressful and turns out to be a difficult experience for both couples and individuals4. It is a non-normative event that questions the universal and biological values of the continuation of species5. Therefore, infertility is more than a health condition. It is a circumstance with impact throughout life, with implications on the personal, social and relational extensions of the human being5. It is often associated with emotional changes such as anxiety, depression, anger, alienation and personal depreciation, which can potentiate pre-existing factors of infertility1,2,3. Due to these devastating effects in the emotional sphere with destabilization of the individuals’ personality, the couple's approach must always take this reality into account and anticipate/prevent the feelings and frustrations that may arise during the diagnosis and treatment of infertility2,6.
The importance of Psychology in the study of infertility is ruled by two models: one that assumes that psychological factors have an impact on its etiology (psychogenic model) and another one that values the impact of this negative experience on the emotional and relational adaptation of infertile couples. It is recognized that stress activates the hypothalamus-pituitary-adrenal axis, which can have hormonal and oxidative stress consequences, with long-term neuroendocrine changes. This may possibly affect reproductive capacity5,7. It is also consistent, within researchers, that stress can induce emotional perturbances that affect the womens’ behavior, leading to bad habits that can compromise fertility5. However, further research is needed to clarify and strengthen these associations5.
Nevertheless, the benefits of psychological intervention in couples undergoing infertility treatments are well documented. Several studies prove that this methodology shows improvement in outcomes and pregnancy rates5,7-9. This is integrated with the idea that if patients use their skills to learn how to deal with the dissatisfaction and failure that infertility brings, ART can be more successful. Studies have shown that stress, depression, anxiety and negative emotionality are higher in women who were unable to conceive. Also, quality of life decreases with infertility5,7,10,11. When comparing stress at the first evaluation with the one assessed within the treatment, it appears that the initial one has a greater impact on evaluated couples5.
Being infertility an interaction of multifactorial causes, with great demand and personal suffering, it is imperative to adopt an integrated view where physiology is intimately related to social and psychological processes6.
Therefore, the purpose of this study was to identify the factors within the psychosocial component that contribute to the effectiveness of infertility treatments and overall outcomes of pregnancy and birth.
Methods
This is a retrospective, descriptive and causal study. Our aim was to evaluate couples with infertility criteria (inability to obtain pregnancy after 12 months or more of regular sexual intercourse without using contraception12) that were referred to this hospital’s Reproductive Medicine Unit. A time gap of first evaluations was chosen from February of 2015 to December 2018, allowing a sample of 278 infertile couples.
The main objective was to make a descriptive analysis of the infertile couples and to cross clinical data with clinically relevant psychological symptoms. We compared treatment outcomes and questionnaires’ results, in order to assess the stress inherent to their condition. Questionnaires were applied and collected by a Clinical Psychologist to both members of the couple separately, in order to make a psychological assessment before starting the treatment, which is mandatory by law19 in our country. These data were analyzed and translated into symptons and problems through Brief Symptom Inventory (BSI)13-16 and Fertility Problem Inventory (FPI)17,18.
Regarding the couples’ anamnesis and clinical evaluation, data were collected on their age, history and cause of infertility, the treatments performed, and records of pregnancy and birth. These variables were obtained through clinical records analysis of the present unit, where anonymity was guaranteed. Gender comparisons will be made in order to understand if there are significant differences in the way the elements of the couple see and face infertility.
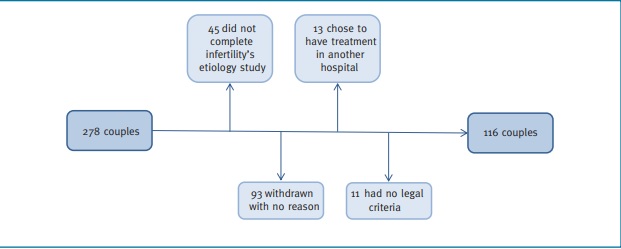
Since the patients were seen in several appointments by the assistant doctor throughout infertility work up, some of them didn't move on to the second phase of the study: treatments and ART. From that first sample of interviewed couples (N=278), 45 didn't complete full clinical evaluation due to withdraw, so etiology of infertility could not be determined. Moreover, 93 couples withdraw before the treatment, 13 chose to have treatment in another hospital and 11 had no legal criteria to benefit from treatment at a public hospital, mainly due to age issues. That means only 116 couples proceeded to treatment in this hospital. Visual representation of the sample’s evolution can be found in Figure 1. Only intrauterine insemination (IUI), in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) were registered as a possible treatment. Since ovarian stimulation was performed in every woman to optimize the remaining techniques, this was not considered a treatment.
The cause of infertility was classified as feminine, masculine, both genders or idiopathic. Recurrent miscarriage and spontaneous pregnancy were classified as idiopathic when the etiology could not be found. Pregnancy was considered positive when a positive value of βhCG was obtained (βhCG >5 IU) because, although patients are aware of the possibility of biochemical pregnancy, it gives them hope regarding clinical pregnancy.
This project was approved by the Ethics Committee for Health of this hospital, and authorized by the Administrative Council (study n.º 34/2019). Restricted rules were maintained and international ethical standards were applied throughout the investigation, with emphasis on anonymity.
Statistical analysis20,21 was performed using SPSS v.25.0. For BSI and FPI scales, a value greater than the reference values, presented in brackets in Table I for BSI16 and the value of “3” for FPI18, allow to admit the presence of psychopathological symptoms and assess the stress associated with infertility. Wilcoxon’s Sign (Z) was used to analyze the differences between the prevalence of symptoms and fertility issues in both genders. Psychometric quality, through Cronbach's Alpha, used to verify internal consistency and scale validity was also used for BSI and FPI22-25. For the final results, Odds Ratio (OR) enabled the analysis of a relationship between two events to prove if some characteristics would make it more likely to get pregnant or have a child26,27. A level of statistical significance was established for p<0.05.
Throughout the research, there were some limitations. There was no control group since it was not possible to apply BSI and FPI to non-infertile couples. The original sample got smaller due to a lot of withdraws, so the comparison between BSI and FPI and outcomes of pregnancy and birth after treatment had fewer statistically significant results. Besides that, full characterization of tf1he sample was still possible when it comes to age, infertility history, etiology (with 45 omitted cases) and application of the scales.
Results
Between 3rd of February 2015 and 16th December 2018, 278 couples resorted to infertility consultation to make their first clinical and psychological evaluation.
The mean age for men was significantly supe-
rior compared to women (34.5 vs. 32.8 years;
t(277) = -6.120; p<0.001). Also, in both genders the most prevalent age range was 30-34 years (39.9% in women; 31.7% in men).
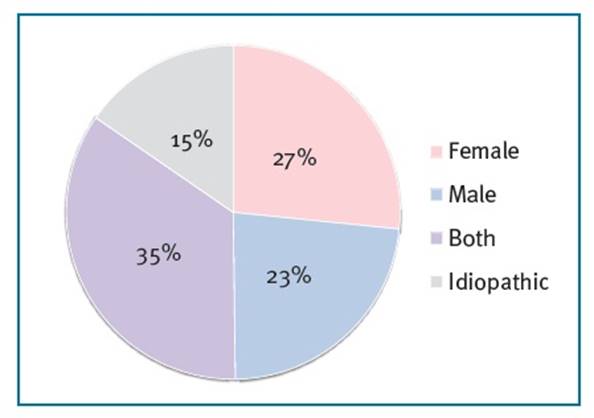
Most women had primary infertility (66.3%). From the 233 couples who completed their infertility study, feminine etiology (27%) was slightly more frequent than masculine (23%), while in 15% of the cases the cause could not be found. Causes of infertility can be found in Figure 2.
Regarding the 116 couples who had ART, most couples had more than one cycle performed. IVF (N=93) and ICSI (N=91) were the most frequently performed treatments, followed by intrauterine insemination (N=47). In almost half of the cases (48.2%) the treatment was successfull, so pregnancy occurred, and 68.6% of these pregnancies led to childbirth. When we calculate the percentage of success per cycle of ART performed, IVF is the most successful one. When it comes to pregnancy, IVF had 27.9%, IUI 27.7% and ICSI 26.4% pregnancies per cycle. The percentage of births per cycle is also higher in IVF (19.6%), followed by IUI (17.4%) and finally ICSI (6.3%), with statistically significant differences (p<0.05).
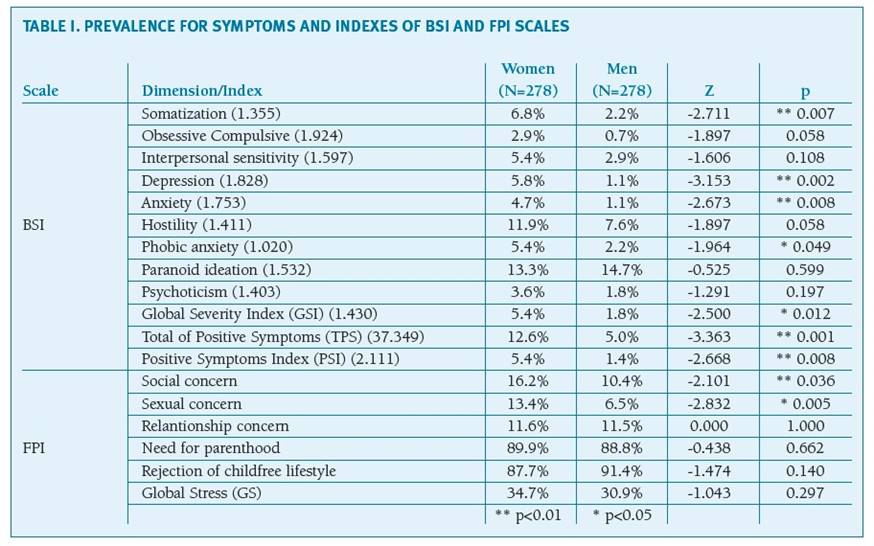
The prevalence of clinically relevant psychological symptoms (BSI) and fertility problems (FPI) can be analyzed in Table I. It can be seen that Somatization, Depression, Anxiety, Phobic anxiety, as well as Global Severity Index (GSI), Total of Positive Symptoms (TPS) and Positive Symptoms Index (PSI) are always significantly higher (p<0.05) for women. Social and sexual concerns are also significantly superior (p<0.05) in women, while Rejection of a childfree lifestyle (91.4%) is bigger in men. Need for parenthood and Rejection of childfree lifestyle are extremely prevalent in both sexes.
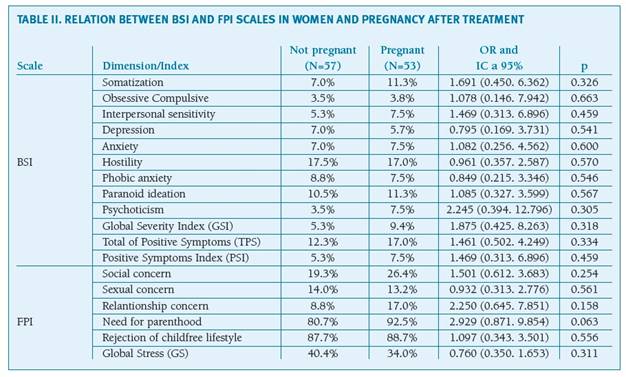
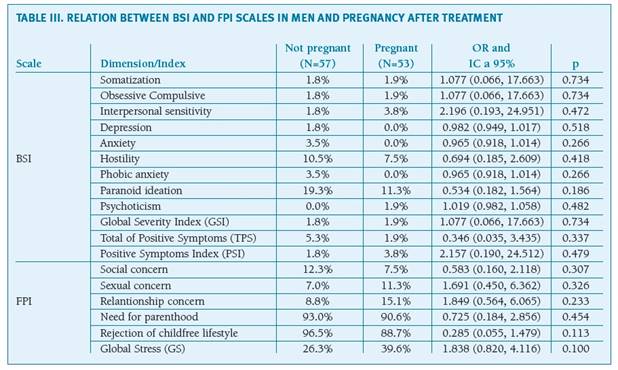
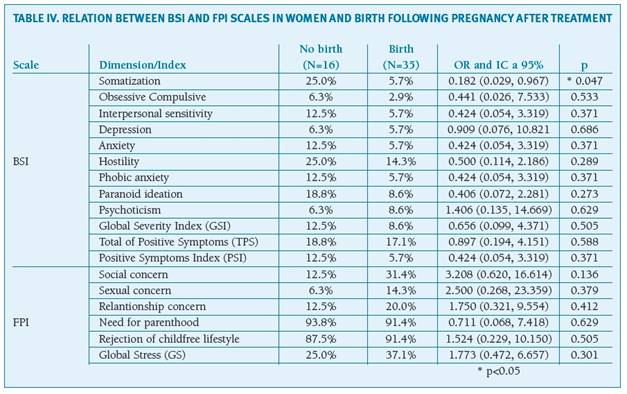
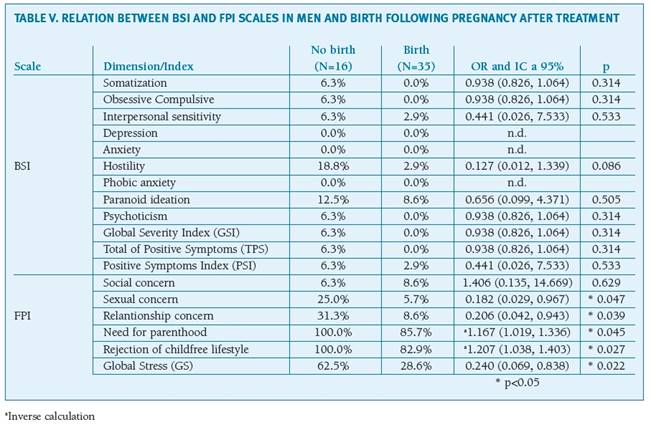
When comparing BSI and FPI scales with pregnancy and birth rates, only couples who had treatment were considered. Relationship between psychopathological symptoms, infertility problems and treatment success, regardless the ART performed, can be found in Tables II to V and will be further analyzed in the following Discussion.
Discussion
According to the Human Fertilization and Embryology Authority in 2006, male and female factors of infertility have a similar proportion of 32.5%, whereas mixed factors, which affect both sexes, make up 10.8%. Idiopathic or unexplained infertility is around 23%3. Despite the differences found, it is consensual within the literature that male and female factors contribute in a very similar way1-3,28, as found in this study. It is also described that in 10% to 20% of the cases, the main factor of infertility cannot be identified3 which makes the 15% of idiopathic cause in the present study well represented.
Regarding the inventory of psychopathological symptoms (BSI), it is unmistakably verifiable that women have a higher prevalence of symptoms than their partners. This is consistent with the results from a compilation of studies from Moura-Ramos5. These findings reflect a role that women shouldn't have in nowadays' society. Despite the feminine empowerment in modern societies, women still suffer a bigger social stigma10,11, since men’s satisfaction with life in the future does not depend so much on having children5.
Although infertility should be seen as a problem for both elements of the couple, several studies prove that women suffer more from infertility6 and tend to react with higher intensity to adverse situations29. Besides that, it is proven that stress is more prevalent in infertile women when compared to control groups5,7,29.
Some studies defend that the tardiness and complexity of infertility’s diagnosis and treatment can precipitate psychopathological symptoms in 25% to 60% of infertile people29, with a greater emphasis on depression and anxiety6, besides frustration, social isolation and sexual difficulties29. Nevertheless, it is necessary to rethink the idea that infertility is exclusively the cause of psychological stress6 and adopt a holistic view where it can be a cyclical, cause-effect process.
For FPI scale, which analyzes the global stress inherent to fertility problems, we can conclude that, for these couples, there is a parenthood pursuit interdicted by infertility. This is predominant in both elements of the couple. Need for parenthood (89.9%) is slightly higher in women10,30, whereas Rejection of childfree lifestyle is more prevalent in men (91.4%). Although the remaining problems are less prevailing, once again we observe they are significantly more present (p<0.05) for women30 when it comes to Social (16.2%)5,10 and Sexual concern (13.4%)10. The Global Stress Index is also higher in women (34.7%), similar to other studies5,10.
The main goal of this investigation was to understand whether psychosocial factors had an influence on the effectiveness of infertility treatments, in order to improve psychological interventions and therapies and acknowledge them as an intrinsic process of the treatment itself. However, to be successful it is not enough to just conceive. It is desirable that the pregnancy reaches term so the couple can meet their wishes of having a child. For this, the influence on both pregnancy and childbirth was studied.
When analyzing the relationship between the problems of BSI scale and pregnancy’s occurrence, we found that Depression, Hostility and Phobic anxiety were higher for women who did not become pregnant after treatment5,29. In men, these symptoms are also higher when pregnancy did not occur, adding up Anxiety and Paranoid ideation to the list. On the other hand, curiously Psychoticism (OR=2.2) and Somatization (OR=1.7) were more prevalent in woman who did got pregnant. Although there are differences between outcomes, these correlations are not statistically significant.
Now stress is unequivocally associated with a decrease in quality of life and it is unanimously documented that infertility has a negative impact on it5,6. According to Palomba et al, besides the fact that negative symptoms, such as depression and anxiety, are higher in infertile women compared to fertile ones, they are also associated with lower pregnancy rates and lower outcomes in Reproductive Medicine (including ovarian reserve, fertilization, pregnancy and childbirth)7. Lower quality of life is also related to age, female gender and longer duration of infertility5.
Although these results regarding BSI, FPI and pregnancy rates are a bit heterogenous, we can acknowledge that some symptoms that bring negativity to the couple's life are related to worse pregnancy rates in both genders. Some studies indicate that the more negatively the couple feels their infertility (greater emotional reactivity), the greater stress it can bring to their lives5. Some more recent studies even claim that psychological intervention has the potential to lower the stress inherent to infertility and is associated with significant increases in pregnancy rates8,9.
When we tried to understand which factors had an impact on the follow up of pregnancy and which couples carried out pregnancy until the end, the results were way more enlightening. It was possible to observe that Somatization in women (p<0.05) was clearly related to abortions, as well as most symptoms of BSI scale. There were found no differences between genders, as men also have a higher prevalence of psychopathological symptoms when childbirth does not occur, even though Depression, Anxiety and Phobic anxiety were not positive for males. The only symptom that seems to differ from this pattern, interestingly, is psychoticism in women (it is associated with higher birth rates, as well as pregnancy, as seen before).
When we analyze infertility problems through FPI scale, we see that the probability of becoming pregnant after treatment is 2.9 times higher for women in need for motherhood (OR=2.9). Although this is not statistically significant, once again, this makes us feel like the experience of infertility is somewhat shaped by social context, where the meaning of parenting in the life of these individuals plays a fundamental role5,11.
For men, there is a significant relationship between the Need for parenthood and delivery. Since it is calculated in an inversed way, the probability of abortion is on average 1.2 times higher (OR=1.2; p<0.05) for those who have this characteristic. Sexual and relationship concerns also play an important role in men, as they are negatively correlated with childbirth (p<0.05). The probability of pregnancy reaching term is 0.18 times lower for men with concerns about their sexuality (OR=0.18) and 0.2 for men who have relationship issues (OR=0.2).
This may mean that stress related to the inability of conceiving and the frustration inherent to that situation can probably make men feel incapable or less confident when it comes to sexual and reproductive performances. Besides that, Sexual concern is significantly superior (p=0.026) in male etiology. It may also be thought that their biological role might be taken into risk. We must not forget that erectile dysfunctions with clinical repercussions are statistically higher in infertile men, when compared to fertile groups5.
Sexual concern (OR=0.9) is also associated with lower pregnancy rates in woman. As for Global Stress, in men they are associated with miscarriage (OR=0.3) and, in women, with lower successful rates in ART (OR=0.7).
In this investigation it was found that the couple's psychosocial component has an influence on the infertility treatment process, with an impact on its outcome. Psychopathological symptoms were higher in couples with negative outcomes after treatment, especially regarding childbirth, the ultimate goal of fertility treatments. Therefore negativism was associated with unfavorable results in both sexes.
That being said, it is imperative to adopt an integrated view of infertility, from an individual and familiar perspective. Social and emotional dimensions as well as surrounding environment cannot be excluded, in order to advocate the couples’ adaptation process5,6. Psychology could and should have a more active and interventional role here, as an essential part of the treatment. The purpose would be not only for the psychological support needed, but also for the preponderant role that psychosocial interventions can have in the treatment outcomes5,7-9. In this way, we hope this study can open doors for a fundamental convergence between Psychology and Reproductive Medicine, with a potential improvement of infertility treatments combined with psychoanalysis and psychotherapy.