The authors report the case of a 64-year-old woman, referred to the gynecology consultation by her family doctor due to a vulvar nodule noticed in the previous month. She underwent hysterectomy and bilateral adnexectomy 20 years before, due to uterine leiomyomas, and used hormone replacement therapy for one year.
On gynaecological examination, a 2 cm unpigmented lesion was observed on the internal surface of the left hemivulva, at the left labia minora (Figure 1 a)). The lesion was lateral and had no relation with the urethral meatus. No macroscopic lesions were identified in the vaginal mucosa and vault. The lesion was interpreted as a benign cystic lesion, and was proposed for an excisional biopsy. On the day of the surgery, one month later, the lesion was slightly increased and ulcerated (Figure 1 b)). Histology revealed a vulvar malignant melanoma, epithelioid, with a maximal thickness of 1.9 cm; no signs of tumor lymphovascular invasion or satellite nodules were identified.
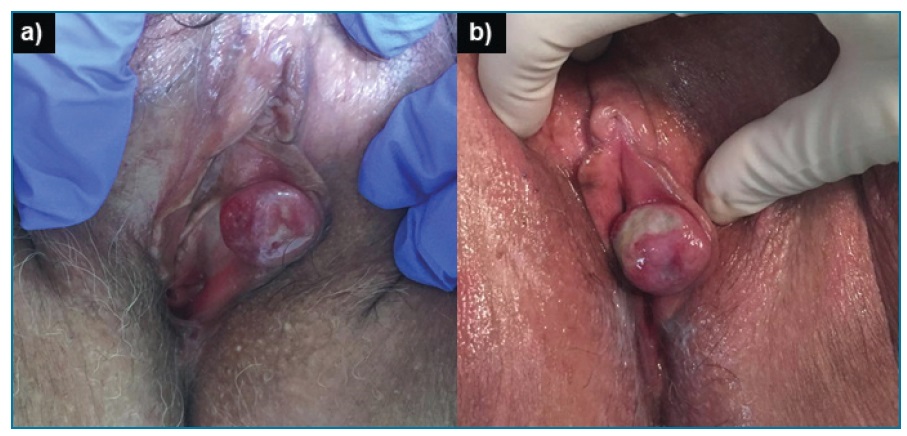
Figure 1 2 cm lesion was observed on the internal surface of the left hemivulva, at the left labia minora. The lesion was nodular and unpigmented, lateral and had no relation with the urethral meatus. It was interpreted as a benign cystic lesion. Histology revealed a vulvar malignant melanoma. a) The lesion at the day of the first consultation. b) One month later on the day of the surgery. The lesion was slightly increased and ulcerated.
The patient was proposed for simple surgical margins extension and sentinel node detection and biopsy. Two homolateral nodes emitting radiation and methylene blue stained were identified. Several palpable nodes were also identified, although not emitting radiation and not stained, and were therefore excised. Histology revealed no residual tumor on the vulva; six lymph nodes were identified, one of them (not the sentinel) having a 17 mm metastasis, with 3 mm extracapsular extension. Thoraco-abdomino-pelvic computed tomography showed no signs of pelvic adenopathies nor distant metastasis. The final staging was T1bN2cM0 (FIGO IIIC). Radiotherapy (RT) was performed on the left inguinal region (60Gy/30fr/6 weeks), complicated by radiodermatitis. The patient completed one year of follow-up, free of disease.
Vulvar malignant melanoma is a rare type of tumor, accounting for 5% of all vulvar malignancies, with an incidence of 1.36 cases per million women per year1. The mean age at diagnosis is 62 years1. Patients present a vulvar lesion; other presenting symptoms are pain, bleeding, pruritus, usually occurring at advanced stages, so diagnostic delay is common2. Clinical assessment of pigmented lesions is difficult and VMM can be macroscopically amelanotic in 27% of cases3. The final diagnosis is histological2.
The prognosis is poor, with reported 5-year survival rates between 10 and 63% and high recurrence rates between 42 and 70%2. This is explained by biological aggressiveness but also unfavourable characteristics at presentation. Prognostic factors are higher age, advanced Breslow thickness and lymph node involvement2,4,5.
Surgery is the cornerstone for the treatment of primary VMM2,4,5, being wide local excision preferred to radical vulvectomy (similar survival rates with lower morbidity)2. The role of sentinel lymph node biopsy is still under evaluation but systematic elective lymph node resection (ELND) is not recommended2,4. Nonetheless, ELND in case of palpable nodal involvement may prolong disease-free survival2. RT and chemotherapy as adjuvant treatment do not show survival benefit2,5. RT of the groin has not been studied in VMM2. Post-operative RT can be considered in case of positive nodes2.














