A 30-year-old nulliparous woman was admitted to our labor ward in spontaneous labor at 40 weeks plus 1 day of gestation. She was healthy and the pregnancy was uneventful. The third trimester ultrasound reported a fetus growing on the 25th centile and a non-previa placenta. Rupture of membranes occurred spontaneously during the latent phase of labor and the patient had a normal vaginal delivery. The newborn girl weighed 2975g and the APGAR score was 10/10 at the first and fifth minutes, respectively. After a natural and seemingly complete placental delivery an oxytocic perfusion was started, according to the protocol of our unit. The uterus contracted normally and blood loss was considered normal. Surprisingly, during placental inspection after delivery, we noticed a lone blood vessel diverging from the placenta with no cotyledon attached to it, and succenturiate placenta was suspected (Figure 1). An ultrasound examination was performed, which showed a probable placental remnant identified in the uterine fundus. We performed a manual revision of the uterine cavity and extracted the accessory cotyledon (Figure 2). Afterwards, the ultrasound revealed a thin endometrial line. The patient was discharged at the second day postpartum.
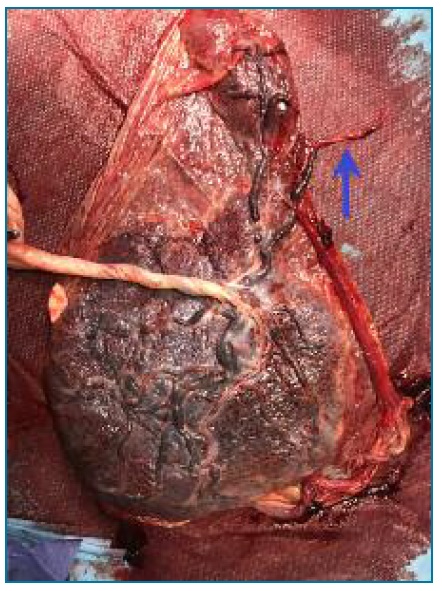
FIGURE 1 Succenturiate placenta with a blood vessel coursing through the membranes with no cotyledon attached (blue arrow).
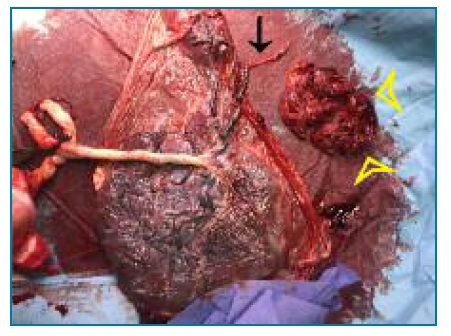
FIGURE 2 Succenturiate placenta and a blood vessel with no cotyledon attached to it (black arrow). Placental remnant recovered after manual revision of the uterine cavity (yellow marks).
Succenturiate placenta is a placental morphologic variant in which there is an abnormal development of one or more accessory cotyledons in the membranes. These accessory lobes are usually connected to the main body of the placenta through fetal vessels that course in the membranes. (1
The reported incidence of succenturiate placenta is 5%.2 The risk of this anomaly increases with advanced maternal age, infertility and in vitro fertilization, pelvic infection, preeclampsia, and implantation over leiomyomas, in areas of previous surgery, in the cornu or over the cervical os. (2), (3
The antenatal diagnosis of this condition can be made by ultrasound, particularly color Doppler. (4 A previous diagnosis facilitates obstetric management as this condition increases the risk of vasa previa, postpartum hemorrhage and retained placenta and might contribute to maternal morbidity and even mortality. A study showed that when the diagnosis of succenturiate lobe was made the frequency of vasa previa was 2,1% and a 4.29-fold increase in poor obstetrical outcomes occured. (5 Additionally, it is associated with prematurity, impaired fetal growth and cesarean delivery. (3
With these images, we aim to raise awareness of the importance of a thorough gross placental examination after delivery. This can help diagnosing other obstetric issues besides succenturiate placenta, such as placental abruption, retained placental lobe, placentomegaly, infeccious disease or umbilical cord complications like single umbilical artery or velamentous insertion. We also highlight the importance of an antenatal diagnosis by routine obstetric ultrasound, as this alerts the obstetric team for possible labor complications.














