A subchorionic placental cyst (also denominated “placental surface cyst”, “chorionic cyst”, and “membranous cyst”) is a cystic mass arising from the placenta surface. It has an estimated prevalence of 2-7% and is generally simple and small1. Rarely, the subchorionic placental cyst may impact on the pregnancy outcome2.
The images presented concern to a 34-year-old gravida 2 para 1 (normal vaginal delivery) referred to our maternal-fetal unit due to a placental cystic mass in the third-trimester ultrasound. Previous ultrasound examinations in the first and second semesters showed normal findings. Her personal and obstetrical history was unremarkable. She had no risk factors for fetal or placental conditions.
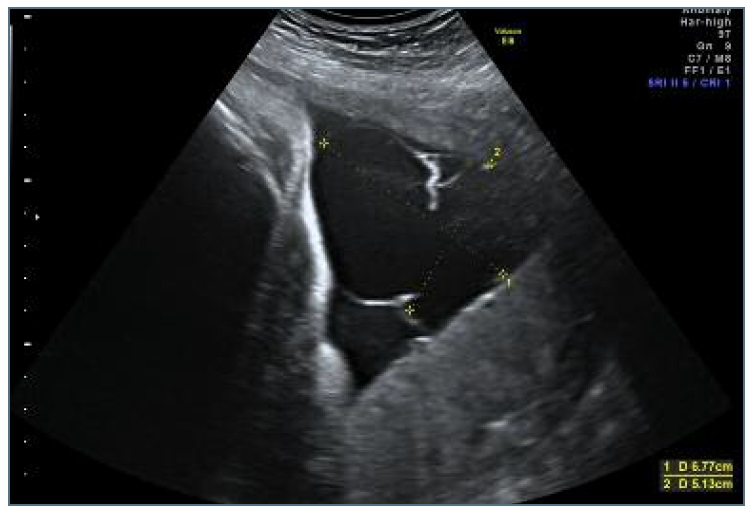
At 36 weeks of pregnancy, the ultrasound exam performed in our unit confirmed the presence of a complex placental cystic mass, composed of three anechogenic cysts. It measured 6.7 x 5.1 cm and was placed near the umbilical cord insertion (Figure 1). Color flow Doppler ruled out any vascular involvement. There were no cord anomalies, and the placenta was posterior high. The estimated fetal weight was of 2045 grams, being at the 2.3 centile according to the Yudkin chart. Doppler examination of the fetal middle cerebral arteries and umbilical arteries (including cerebroplacental ratio) were normal. The remaining ultrasonographic findings were normal.
It was decided to perform an elective cesarean section at 37 weeks to avoid the risk of intrapartum cystic rupture. A female newborn was delivered with an APGAR score of 9 and 10, weighing 2135 grams (3.3 centile). Arterial cord pH was 7,26 and neonatal hemoglobin was 15,1 g/dL.
The placenta weighed 500 grams (25th percentil). The macroscopic examination shown various cysts on the fetal surface adjacent to the cord insertion, with diameters between 6 and 65 mm, and a large sub-chorionic hematoma with 10x11x1,3 cm (30% of placental volume), also called Breus’ mole. (Figure 2) Within the cysts, blood clots and fibrin deposits were observed, as well as a focal separation of the amnion and chorion. The umbilical cord was trivascular with velamentous insertion. The histological examination revealed signs of inadequate blood perfusion.
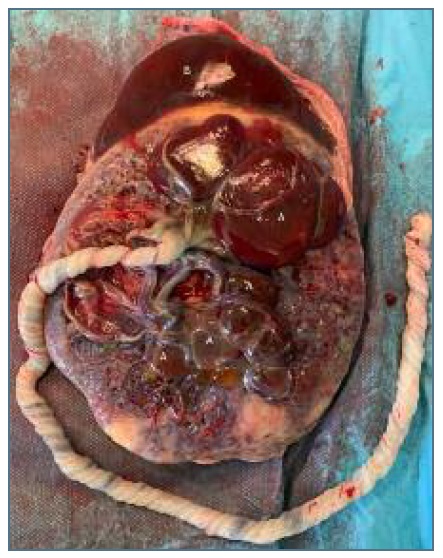
Figure 2 Macroscopic appearance of multiple placental cysts (A) near the umbilical cord insertion after cesarean delivery. A large hematoma (B) called Breus' mole can also be seen.
The subchorionic placental cysts may be simple or complex, and their walls are composed of amnion, chorion, intermediate trophoblasts, and fibrin strands. On the ultrasound, they are usually hypoechoic with swirling echoes and demonstrate low-velocity laminar flow at B-mode or Doppler imaging.
Although the cysts can already be present in the first trimester3, they are usually diagnosed in the late second trimester or third trimester2. The dimensions of the cyst tend to remain stable throughout pregnancy.
In general, small placental cysts are associated with good neonatal outcomes4. On the other hand, large subchorionic cysts (>4cm), in special if they arise near the umbilical cord insertion or within the cord, or if they are more than 3 in number can be associated with fetal growth restriction and fetal distress2), (4), (5. The physiological mechanisms proposed for this association include cord compression, weakening of adjacent chorionic surface, extensive fibrin deposition and placental infarction. Stolla et al. stated that chorionic cyst fluid has prothrombotic properties, which may explain our findings of fibrin deposits and infarction5.
It is essential to consider the diagnosis of placental cysts during the differential diagnosis of cystic lesions in pregnancy, which includes subchorionic and subamniotic hematoma, chorioangioma, fibrin deposits, placental lakes and cord cysts.
In summary, the clinical relevance of placental cysts remains unclear. Generally, when cysts are small, the pregnancy outcome is normal. Nevertheless, in the presence of subchorionic cysts is important to characterized their size, location and relation to umbilical cord insertion. The fetal growth and fetal dopplers should be evaluated more frequently if the cysts are attached near umbilical cord insertion due to risk of fetal growth restriction and fetal distress. The remaining obstetric surveillance must be conducted according to the presence, or not, of fetal growth restriction4.