Introduction
Maternal mortality ratio (MMR - number of maternal deaths per 100 000 live births) dropped about 38% worldwide between 2000 and 20171. At that point, global MMR was estimated in 211 per 100 000 live births. However, MMR is 40 times higher in world’s least developed countries in comparison to Europe1: the vast majority of maternal deaths (94%) occurs in low and medium-income countries, and most cases are preventable2), (3. As a result, the World Health Organization (WHO) and partners intend to reduce global MMR to less than 70 per 100 000 live births in 2030, by stopping preventable maternal mortality2. Concerningly, in Portugal MMR slightly increased in the past few years. In 2018 it reached 17,2 per 100 000 live births, whereas from 1995 to 2016 it was consistently under 94.
A significant proportion of maternal deaths in developed countries is related to massive blood loss or hypertensive disorders, which are manageable in adult Intensive Care Units (ICU), with expected survival5. ICU admission may be considered an objective marker of severe maternal morbidity (SMM) (6), (7, however, approximately two-thirds of cases could be missed being this the only criterion8. Surprisingly, according to Mengistu et al, the reduction in MMR in high income countries (HIC) is associated with a paradoxical increase in SMM, driven by a combination of factors, including advanced age, obesity, comorbidities and operative delivery9. Nonetheless, Loverro and Vasquez et al. described ICU obstetric patients as young, primiparae, with low prevalence of chronic illnesses. This indicates that ICU admitted women generally have a serious pregnancy-related complication10), (11, reinforcing that ICU admission represents a small part of the population with SMM. Also, cardiovascular pathology is gaining ground as an important factor in maternal morbidity in HIC. In countries like the USA and UK deaths due to cardiovascular disease are unchanged or increasing despite the reported global decrease in direct causes of maternal mortality12.
Management of critically ill women during pregnancy, delivery and puerperium is complex. These patients are fundamentally different from other critically ill ones, requiring specific pregnancy physiology and pathology knowledge13. Therefore, it is mandatory that both obstetricians, intensivists and anaesthetists are involved, in order to provide a multidisciplinary approach5), (14. Although illnesses are generally severe, fatality rate is relatively low, with possibility of full recovery5), (11. Adequate access to ICU facilities has been recognised as key to maternal mortality reduction in HIC15. A better understanding of obstetric patients characteristics admitted to ICU could point to where the focus of obstetric training and awareness should be directed at, and further reduce maternal mortality and morbidity16, transforming deaths into ‘near-misses’17.
Little is known about the ethnicity impact in maternal outcomes. Some studies found associations at this level with ICU admission, which is greater in non-europeans6 and black race18. A prospective cohort study, in Netherlands, reported a 1,4 fold increased risk (95% CI 1,2-1,7) of ICU admission in non-western compared to western women5. Nowadays such analysis is of utmost importance, given migration trends, that also include pregnant and women of reproductive age. The number of international migrants is globally estimated at 272 million, which already surpasses some projections made for 205019. Large, prospective multicentre studies are needed to improve insight into the cultural and medical background of these trends20.
The accurate evaluation of ICU obstetric admissions and knowledge of near-miss maternal mortality helps identifying the persisting threats to maternal health21, as reduction of maternal mortality remains a global health priority3.
This study aims to review obstetric admissions to the ICU in a tertiary care centre, and assess incidence, maternal and pregnancy characteristics, required interventions and outcomes.
Material and methods
We retrospectively reviewed the clinical records of all obstetric ICU admissions in a Portuguese tertiary care centre, over a 10-year period (2010-2019). ICU admission was decided among obstetricians, anaesthetists and intensivists. Data were retrieved for each case: medical and obstetric history (including age, parity, nationality, residency, comorbidities, pregnancy type), location of primary obstetric care, gestational age at hospital admittance and at delivery, mode of delivery, ICU admission diagnosis, time between delivery and ICU admission, length of ICU and hospital stay, ICU interventions, maternal morbidity and mortality. Additionally, neonatal variables were also retrieved (birth weight, Apgar scores and neonatal ICU admission). Statistical analysis was performed using Statistical Package for the Social Science (SPSS®) version 23.0. This study was approved by the Ethics Committee for Health of the hospital (3/CE/2021). International ethical standards and anonymity were applied.
Results
There were 38 ICU obstetric admissions, 23974 deliveries and 3555 patients admitted to the ICU in this 10-year period. The median admittance per year was 2,5, with highest incidences recorded in 2011 (n=8), 2018 (n=11) and 2019 (n=5).
Obstetric admissions were 1,07% of all ICU admissions, 2,3% of women admitted to the ICU and 0,16% of deliveries (1,59 ICU admission per 1000 deliveries). All women admitted delivered in our institution. The majority of ICU admissions occurred in the postpartum period (97,4%; n=37), in the first 24 hours after the delivery (73,7%; n=28).
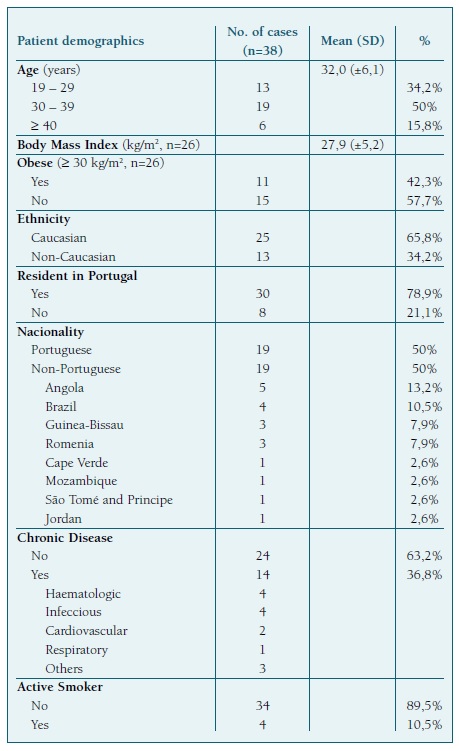
The mean maternal age was 32±6,1 years. Concerning demographics 25 were caucasian (65,8%), 19 were Portuguese (50%) and 30 lived in Portugal (78,9%).
Fourteen patients had a chronic disease (36,8%), four were active smokers (10,5%) and eleven were obese (42,3%, n=26).
Patient demographics are shown in Table I.
Twenty-two women were nulliparous (57,9%). Among multiparous women, previous cesarean section (c-section) rate was 37,5%. Thirty-four pregnancies were single (89,5%) and spontaneous pregnancy rate was 92,1% (n=35).
Thirty-two pregnancies had regular surveillance outside our hospital (84,2%) and three did not attend antenatal care (7,9%).
The mean gestational age upon hospital admission was 35,3±4,2 weeks, and 35,5±4,2 weeks at delivery. The prematurity rate was 52,6% (n=20), and gestational age was less than 32 weeks in 7 deliveries (18,4%).
The main reasons for hospital admission were hypertensive disorders (23,7%; n=9), labour (13,2%; n=5) and labour induction (10,5%; n=4). Delivery took place in the absence of labour in more than half of cases (65,8%), with c-section being the most common mode of delivery, in 86,8% (n=33).
Pregnancy and delivery characteristics are shown in Table II.
Table II Pregnancy and delivery characteristics
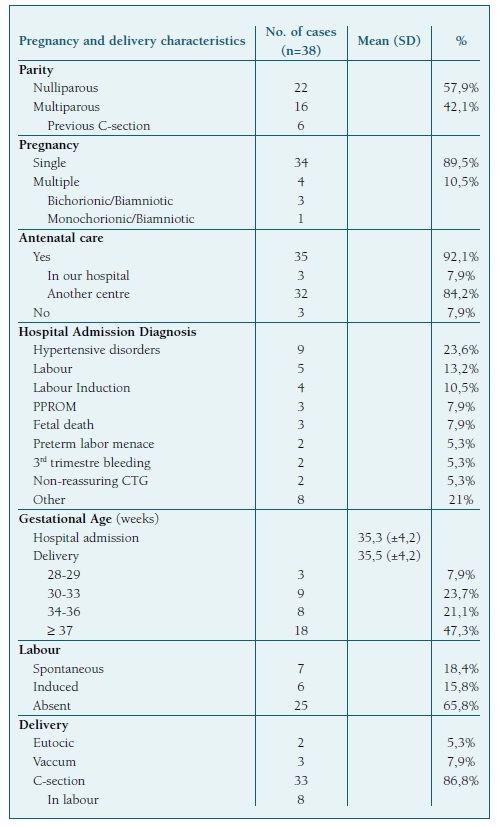
C-section - cesarean section; PPROM - Preterm premature rupture of membranes; CTG - cardiotocography.
A single antepartum ICU admission took place upon pulmonary thromboembolism suspicion, in a 31-week single pregnancy, admitted with preterm premature rupture of membranes. The remaining obstetric ICU admissions were in the postpartum period (n=37).
The most common diagnosis of ICU admission was major obstetric haemorrhage (MOH) with disseminated intravascular coagulation (DIC) (44,7%, n=17), including one case of uterine rupture.
Hypertensive disorders were the second most common cause (21,1%; n=8), all with severe features of pre-eclampsia and 5 of them haemolysis, elevated liver enzymes and low platelet (HELLP) syndrome. No eclampsia occurred. Respiratory and cardiac failure were responsible for 6 (15,8%) and 2 (5,3%) ICU admissions, respectively.
Obstetric ICU admission characteristics are shown in Table III.
Table III Obstetric ICU admission characteristics
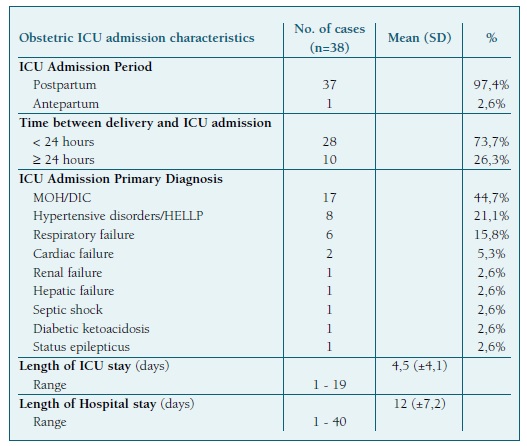
ICU - Intensive Care Unit; MOH - Major obstetric haemorrhage; DIC - Disseminated intravascular coagulation; HELLP - Haemolysis, Elevated Liver enzymes and Low Platelet syndrome.
The most common interventions during ICU stay were mechanical ventilation (52,6%) and administration of anti-hypertensive drugs (39,5%). Prophylactic anti-convulsivant therapy (magnesium sulphate) was given to 10 patients (26,3%).
Twenty-two patients had red blood cells transfusion (57,9%), with mean 5,9±3,4 units transfused. A maximum of twelve units per patient were given twice, both in haemorrhagic shock and DIC. C-section was the mode of delivery on these two occasions - one for elective delivery due to placenta previa and the other for induction failure.
Other blood products were given to 19 patients (50%), and pooled platelet concentrate to 7 patients (18,4%). Three patients required dialysis (7,9%), one of which also underwent plasmapheresis, due to haemolytic-uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP), diagnosed in the late postpartum period. It was a single pregnancy, in a 41-year-old nulliparous patient, admitted at term for labour induction. C-section was performed for failed induction after 3 days. In the postpartum she was admitted to the ICU with DIC. She was transfused with 12 red blood cell units, 4 fresh frozen plasma (FFP) units and 3 pooled platelet concentrates, with the longest ICU and hospital stays (19 and 40 days, respectively). Dialysis was maintained after discharge. Two other cases required dialysis: one of pre-eclampsia with acute kidney failure and a HELLP syndrome.
ICU interventions are shown in Table IV.
Table IV ICU interventions

*Range of units per patient: 1-12 packed red cell units (mean 5,59±3,4); 1-13 FFP units; 4-14 FFP+CPP units. ICU - Intensive Care Unit; FFP - fresh frozen plasma; CPP - cryoprecipitate.
The mean length of ICU stay was 4,5±4,1 days, longer in c-section comparing with vaginal delivery (4,9±4,2 vs. 2±0,7 days, p=0,14). The mean length of hospital stay was 12±7,2 days.
No maternal deaths were recorded. Postpartum hysterectomy was the main morbidity and all cases were due to MOH. It was performed in 5 patients (13,2% of all patients and 29,4% of MOH). Two of them were subtotal (with cervix preservation) and histology confirmed two cases of placenta increta.
Newborns had a mean weight of 2402,1±780,2g. The median 1st minute Apgar score was 7 (0-10), 5th and 10th were, respectively, 9 and 9,5 (0-10). Twenty-eight newborns (66,7%) required Neonatal Intensive Care Unit admission. Most were admitted for prematurity (64,3%; n=18), neonatal surveillance (14,3%; n=4) and respiratory distress syndrome (7,9%; n=3).
There were 4 fetal deaths, all in single pregnancies. Three took place before hospital admission, at 30, 34 and 39 weeks, with placenta abruptio, DIC and HELLP syndrome, respectively. One occurred after major placental abruption, in a 32-week patient admitted to the hospital for menace of preterm labour.
Discussion
Obstetric care analysis is of utmost importance to promote best practice and outcomes. Maternal mortality remains the health metrics in many reports, despite its low rates in HIC and the discrepancy with low-income countries. As a result, maternal morbidity recently became a main topic of research. Most obstetric complications are manageable in adult ICU. Therefore, ICU admission may be considered an objective marker of SMM, and its analysis a key for further improvement in maternal healthcare.
As a relatively small number of obstetric patients develop complications that require ICU admission, a long-term analysis is more appropriate, for which a 10-year study is fitted and consistent with other published reports on the subject. The incidence of obstetric ICU admission in this study is in accordance with the literature, regarding HIC13 - obstetric admissions represented a small proportion of both ICU admissions (1,07%) and deliveries (1,59 ICU admission per 1000 deliveries).
Year-to-year analysis revealed asymmetric distribution of ICU obstetric admissions throughout this period. Outliers were recorded in 2011, 2018 and 2019, the last two mimicking the rise seen in Portuguese MMR4.
The demographics review showed that all patients admitted to the ICU for obstetric reasons in 2011 lived in Portugal and all but one were caucasian. In contrast, only 54,5% (n=6) and 40% (n=2) of patients admitted in 2018 and 2019 lived in Portugal, and 54,5% (n=6) and 80% (n=4) were non-caucasian in the same years, respectively. As a result, we could question if these outliers’ peaks may, in part, be associated with migratory trends. Nowadays, maternal demographics heterogeneity cannot be disregarded, due to the increasing migration trends, imposing new challenges on obstetric practice. In the upcoming years, we won’t be able to perform a strictly dichotomic research (high vs. low-income countries). Efforts must be made in order to balance the gap, as maternal health cannot be disregarded by being based on the countries income level.
Proper and timely care is a universal right. Lack of surveillance in pregnancy is a morbidity risk factor, which can also be linked to migratory and low resource groups22. Nonetheless, most patients admitted to the ICU had antenatal care in a different institution (84,2%), and only 7,9% completely lacked obstetric surveillance (n=3). Communication barriers may additionally contribute to suboptimal care in an otherwise considered proper antenatal surveillance23.
Additionally, obesity and overweight are known as the epidemics of the 21st century and maternal demographics is no exception. Mean body mass index of obstetric patients admitted to the ICU (n=26) was 27,9 kg/m2 (±5,2), with 42,3% obesity rate. This trend is of highest importance as it could dictate poor maternal outcomes9, besides being a modifiable risk factor.
Statistics of obstetric ICU admittance vary across literature: MOH and hypertensive disorders are the two most frequent causes, and postpartum is the main time for ICU admission5), (10), (24. We also verified this trend in our study, since almost all obstetric ICU admissions occurred in the postpartum. Prompt recognition of illness severity and multidisciplinary team assessment, with close interface decision for ICU admission, are major points to pursue low maternal morbidity and mortality14), (25. This is in accordance with our study results, as time mediated between delivery and ICU admission was less than 24 hours in most cases, with low morbidity and no mortality recorded.
MOH was the most common cause for obstetric ICU admission in our study, with DIC diagnosed in more than a third of these patients. Transfusion was the most common ICU intervention, more than half with red blood cells. Other blood products were transfused and cannot be disregarded when facing obstetric haemorrhage, providing adequate patient resuscitation. All obstetric ICU admissions for obstetric haemorrhage occurred in the postpartum, the majority after c-section (70,6%, n=12).
Average weight of newborns in this group was superior to the global mean weight (2911±417g vs. 2402,1±780,2g). Two fetal deaths occurred in this group, one diagnosed upon hospital admission and the second resulted of massive placental abruption, after hospital admission for menace of preterm labour.
Postpartum hysterectomy was needed in a third of these patients, all after c-section delivery. Their mean age was 34,4±1,3 years, and all but one were multiparous women. Only one patient had two previous c-sections and concurrently a placenta previa, admitted at 36 weeks with placental abruption. Two hysterectomies were performed immediately after delivery, resulting from intra-operatory diagnosis of placenta accreta spectrum disorders (both histologically confirmed as placenta increta). The remaining patients where reoperated, between 1 and 24 hours post-delivery. Cervix was preserved in two patients (subtotal hysterectomy), which is a common practice in this setting, since it has been associated with less operative time and blood loss26.
Hypertensive disorders were the second most common cause for obstetric ICU admission, and the main reason for hospital admission in this study. The majority of women were nulliparous, which is a known risk factor for this condition.
Several reports state hypertensive disorders as the leading cause of obstetric ICU admission, with published rates varying between 34 and 75,6%10), (11), (13), (20), (27. This was the case in a Portuguese study where hypertensive disorders represented 35,5% of ICU admissions, followed by MOH (24,7%) and sepsis/infection (20,4%). It should be noted that specifically obstetric infections accounted only for a fraction of the latter27. Our results point to the fact that, despite the important prevalence of hypertensive disorders in the ante and postpartum period, thorough obstetric care can successfully manage these events, decreasing the need for ICU admission. Accordingly, some studies present hypertensive disorders as the second most common cause for obstetric ICU admission, with rates between 6,3 and 29,3%5), (16), (14), (28.
In this spectrum a HUS/TTP diagnosis was made. It is should be noted that diagnosis, although difficult, remains vital as plasmapheresis will be indicated, substantially decreasing mortality29.
Time between admission and delivery was short, with mean gestational age upon delivery slightly superior to the admission one (35,3±4,2 vs. 35,5±4,2 weeks). Delivery took place in the absence of labour in 65,8% of cases, one third of which in preterm pregnancies. C-section was the most common mode of delivery in women who required ICU admission, with similar rates in literature13. Whether this is the result of the negative impact and complications secondary to procedure or if it is needed for critically ill women is still to be understood. In our study the criteria for most of c-sections where pregnancy related disorders and labour was absent. Additionally, more than half were multiparous (50% with previous c-section). Two thirds of c-sections were performed in preterm pregnancies, a third of which under 32 weeks.
As in similar studies, advanced maternal age and chronic diseases don’t appear to be associated with an increased risk for obstetric ICU admission6), (13. Young age (mean 32±6,1 years) and low rate of chronic diseases (36,8%) appear to be major contributors to rapid recovery from serious complications. Mean length of ICU and hospital stay was 4,5±4,1 and 12±7,2 days. Mechanical ventilation was needed in approximately half of patients, comparable to the rates in similar studies.
One possible study bias is the absence of strict criteria for obstetric ICU admission. Nonetheless, all the admissions where thoroughly discussed by a multidisciplinary team, ensuring a criterious mode of care.
Additionally, efforts are to be made in respect to ICU scoring systems used to predict mortality. According to several studies, they appear unsuitable for obstetric ICU admissions, as they’re unable to accurately predict mortality6), (7), (11), (24, thereby the absence of their analysis in this study.
Finally, the retrospective study design can be a setback. However, data were retrieved from electronic files, in a single centre, which ensures accurate retrieval.
Low maternal morbidity and mortality absence are according to current published research concerning HIC, based on timely and adequate interventions. Nonetheless, it is still a relevant problem for any tertiary referral centre10 and an important part of obstetric practice20. Ageing societies, migration trends and obesity are challenges for a new era, and efforts should not be spared regarding maternal health care management and policies.
List of abbreviations
C-section - Caesarean section
CPP - Cryoprecipitate
CTG - Cardiotocography
DIC - Disseminated intravascular coagulation
FFP - Fresh frozen plasma
HELLP - Haemolysis, elevated liver enzymes and low platelet syndrome
HIC - High income countries
HUS/TTP - Haemolytic-uremic syndrome/Thrombotic thrombocytopenic purpura
ICU - Intensive care unit
MMR - Maternal mortality ratio
MOH - Major obstetric haemorrhage
SMM - Severe maternal morbidity
WHO - World Health Organization