Introduction
The current practice of reproductive medicine has evolved towards the individualization of treatments and a personalized choice of ovarian stimulation is increasingly advocated1), (2), (3.
The implementation of this objective implies its extension to the luteal phase. Since the introduction of the concept of luteal phase deficiency in 19494, it has been attempted to prove the influence of the defects of the production of the progesterone or the response to its production as motivators, at least in part, of infertility. However, this concept is controversial, due to the difficulty in establishing diagnostic criteria for this entity5.
The perfect synchrony between a receptive endometrium and a top-quality embryo is vital for assisted reproductive treatments to succeed, meaning that a competent luteal phase is essential. Progesterone is the hormone responsible for the secretory transformation of the endometrium, favoring embryo implantation and immunological tolerance of the implanted embryo, meaning that progesterone is essential for a successful pregnancy6.
A large debate on the need to give luteal phase supplementation in infertile women is ongoing and there is still a lot of controversy concerning the need to supplement according to the type of cycle, the day of the cycle on which supplementation should start, as well as the ideal duration of supplementation. Luteal phase support can be conducted with human chorionic gonadotropin (hCG) or gonadotropin-releasing hormone (GnRH) agonists, but exogenous progesterone is the preferred method7.
Assisted reproductive technology cycles are associated with an insufficient luteal phase, probably because of the supra-physiologic estrogen levels of in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) in the follicular phase, meaning that luteal phase support is essential8. However, there is scarce evidence of the need to do luteal phase progesterone supplementation in intrauterine insemination (IUI) cycles performed with letrozole or clomiphene citrate9. Besides that, supplementation is usually prescribed by reproductive medicine doctors, in many different ways10), (11.
The objective of this study is to make a descriptive report of the use, indications and protocols of luteal phase progesterone supplementation used among Portuguese reproductive medicine doctors.
Material and methods
The authors carried out an online anonymous survey directed to Portuguese reproductive medicine doctors, sent by e-mail to the mailing list of the Portuguese Reproductive Medicine Society. The participation was deemed voluntary, being the request to participate reinforced by e-mail a couple of weeks later.
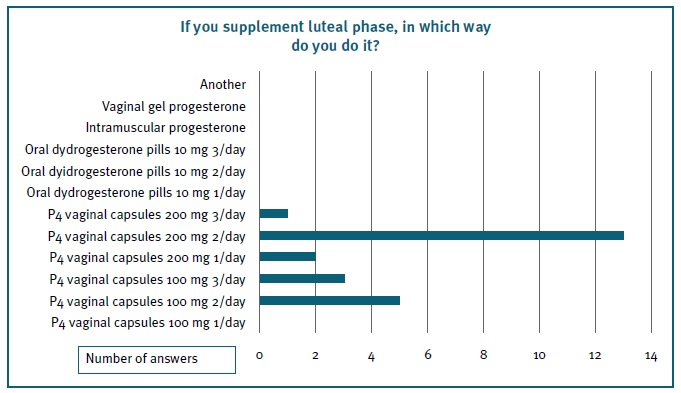
The survey was composed of 13 multiple-choice questions and the estimated time spent to answer was about five minutes. The first three questions aimed at contextualizing the doctor and the unit in which he/she works. The subsequent three questions were about the IUI cycles indication and type of stimulation used. Then, the remaining questions were all about luteal phase supplementation in different IUI cycles and type and duration of supplementation. Table I contains the questions presented.
Data were collected using the online Google Forms platform and statistical analysis was performed using the SPSS® version 21.0.
Results
Of the 80 Portuguese reproductive medicine doctors invited, 41 participated in the study, giving a response rate of 51.3%. There was an equal distribution between doctors working in private and in state institutions. Twenty-five of those doctors (61.0%) had more than ten years of experience working in reproductive medicine.
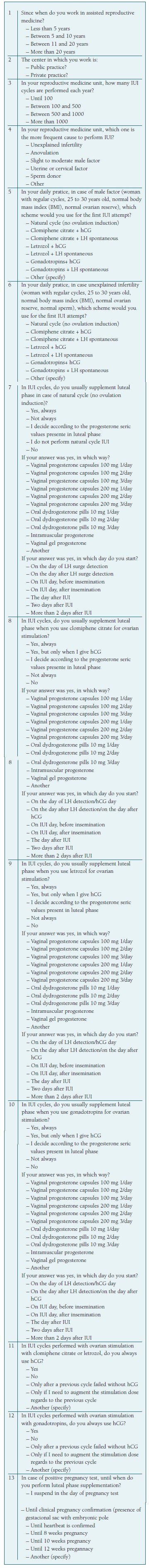
In 21 of the units (51.2%), the volume of IUI cycles performed varies between 100 and 500 per year, while in 18 centers (43.9%) the number is less than 100 per year. The most common reason to indicate IUI is unexplained infertility (51.2%), followed by anovulation (36.6%) (Figure 1).
Concerning the type of medication prescribed, in case of male factor or unexplained infertility, the vast majority of doctors use injectable gonadotropins, followed by ovulation trigger with human chorionic gonadotropin (hCG). Portuguese reproductive medicine doctors rarely use spontaneous LH surge in daily clinical practice in case of male factor or unexplained infertility.
Thirty-four doctors (82.9%) use hCG trigger when prescribing clomiphene citrate or letrozole, whether 41 (100%) use hCG trigger when prescribing gonadotropins.
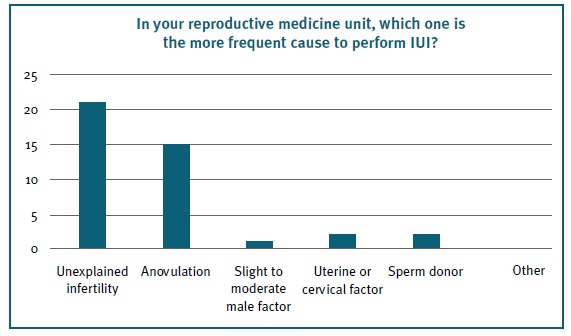
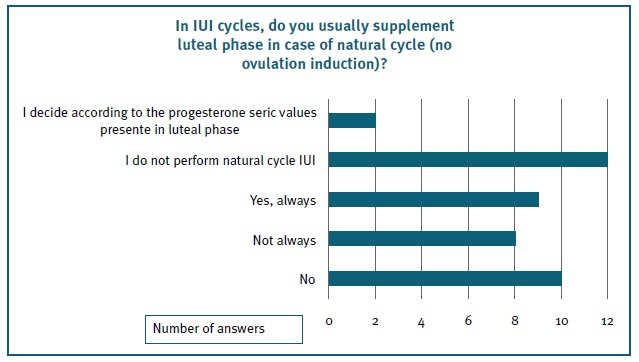
In the case of natural cycle IUI, there is substantial disagreement on the need to perform luteal phase supplementation; however, remarkably, 12 doctors (29.3%) do not perform natural cycle IUI at all. From the doctors who perform luteal phase supplementation in natural cycle IUI, the majority uses progesterone vaginal capsules of 200 mg twice a day, mostly starting on the IUI day (Figure 2a and b).
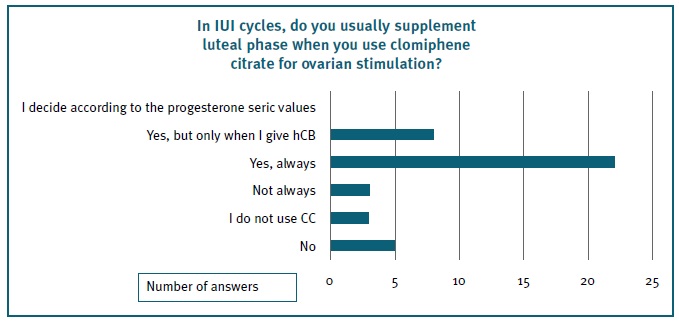
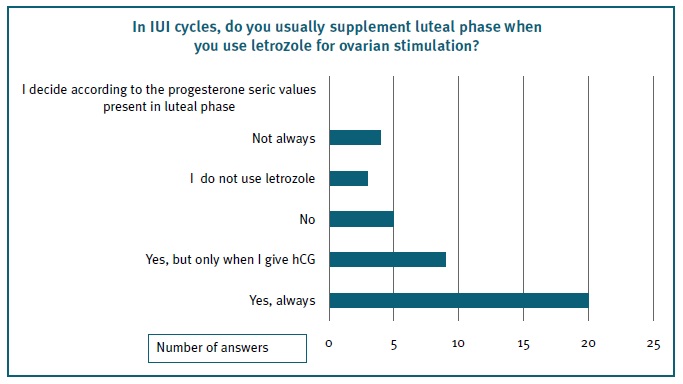
In case of ovulation induction with clomiphene citrate or letrozole, 53.7% and 48.8% of doctors, respectively, supplement the luteal phase (Figures 3 and 4), using 200 mg progesterone vaginal capsules twice a day in 66.1% and 66.7% of cases. Most doctors initiate progesterone supplementation on the day of the IUI.
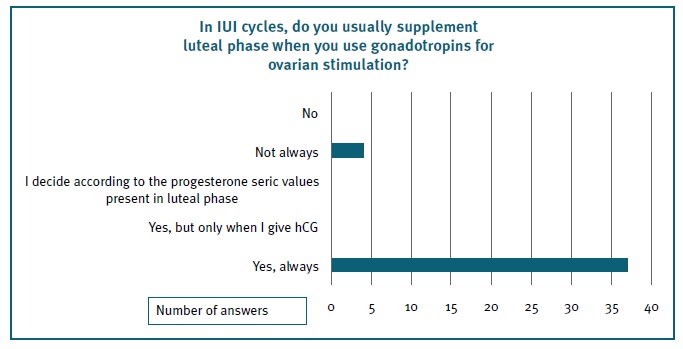
When ovulation induction is performed with gonadotropins, 85.4% use luteal phase supplementation (Figure 5), 58.5% with 200 mg progesterone vaginal capsules twice a day. Luteal phase supplementation started on the day of the IUI in 59.5% of cases and no doctor reported to use other ways of supplementation rather than progesterone.
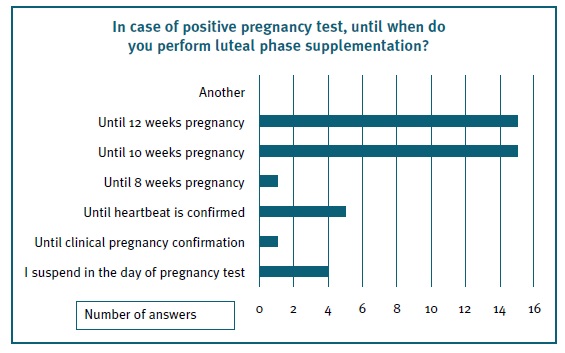
Fifteen doctors (36.6%) end progesterone supplementation at 10 weeks gestation and fifteen (36.6%) at 12 weeks (Figure 6).
The relatively low number of answers does not allow the authors to perform statistical analysis to find significant associations. However, it is remarkable that, when doing ovulation induction with clomiphene citrate or letrozole, there is a higher frequency of hCG trigger used in the centers with lower IUI cycles per year. All the doctors working in units with fewer than 100 IUI cycles per year reported using hCG, versus none of the doctors working in units with more than 500 procedures per year. There is also a higher frequency of progesterone supplementation until 12 weeks of pregnancy in centers with fewer than 100 IUI cycles per year (66.7%) versus centers with more than 100 procedures (13.0%); in fact, only 3 doctors of bigger centers reported supplementation until 12 weeks.
Discussion
The impact of luteal phase supplementation and of progesterone levels on ART outcomes are important research topics. To our knowledge, this is the first Portuguese study concerning luteal phase supplementation use among reproductive medicine doctors. The importance of doing a survey on non-IVF cycles is due to the well-known fact that luteal phase supplementation is mandatory in cases of supraphysiological estradiol levels12. However, because of the ascending use of freeze-all strategies in IVF, frozen embryo transfers are routinely used in reproductive medicine units, with a great interest in natural cycle transfers, creating an opportunity to study luteal phase supplementation in those cases.
Irrespective of infertility etiology, a striking number of physicians report using gonadotropin stimulation at the first IUI attempt, followed by hCG ovulation trigger. This is probably related to the fact that reproductive medicine specialists have the required knowledge to use these drugs.
Most doctors do not perform natural cycle IUI. The authors speculate that this fact is related to the difficulties in planning complete natural cycles in daily practice, on top of avoiding weekends and organizing the work of reproductive medicine units. The same is true regarding the absence of respondents using spontaneous LH surge for IUI cycle programming.
For luteal phase supplementation, whether it is after clomiphene citrate or after letrozole stimulation, more than 20 doctors reported using supplementation, although there is no convincing evidence in literature of its need. Our findings are similar to those obtained in the United States by Weedin and co-workers, who report the frequent use of empiric progesterone supplementation in non-IVF treatment cycles10. Some authors argue that the need to use progesterone in IUI cycles is related to the number of developing follicles, meaning that when more than one follicle grows, progesterone supplementation is essential13.
Regarding luteal phase supplementation after gonadotropin stimulation, there is more agreement among Portuguese physicians, with the vast majority reporting that they always do it. This is in agreement with previous studies, giving evidence that progesterone use is associated with improved live births in gonadotropin IUI cycles9.
Concerning luteal phase supplementation, in our country, vaginal progesterone capsules are, by far, the most commonly prescribed, with the majority of doctors indicating the dose of 200 mg twice a day. No doctor chose intramuscular progesterone, which is most commonly used in the United States than in Europe. Oral dydrogesterone is available in our country in 10 mg pills, but it is still not routinely prescribed by reproductive medicine doctors. Besides the results of the Lotus II trial in luteal phase support for IVF14, demonstrating the non-inferiority of oral dydrogesterone in comparison to vaginal progesterone gel for the presence of fetal heartbeats at 12 weeks’ gestation, this strategy is still not commonly used in our country. However, being a safe and efficacious treatment, with the potential to overcome vaginal irritation and poor patient compliance, the authors believe that it will soon represent a valid option for reproductive medicine.
Regarding the day of starting progesterone supplementation, Portuguese reproductive medicine doctors tend to start it on the day of the IUI, following insemination, with 10 or fewer doctors reporting starting two days after the IUI, irrespective of the stimulation scheme used. In fact, there appears to be a 5 to 6 days’ time window for progesterone start after hCG triggering, because there is endogenous progesterone production from the corpus luteum. After that time, the endogenous production will fall. Within that time window, there doesn’t seem to be any difference in terms of pregnancy rate15.
From the findings of this study and our clinical experience, we can extrapolate that Portuguese reproductive medicine doctors do not usually measure the progesterone serum value. In IVF cycles and mainly in frozen embryo transfers, more and more work is emerging showing the relationship between luteal phase progesterone measurements and overall cycle outcomes16), (17, which is not the case in IUI cycles.
Regarding clinically relevant statistical associations, the small sample size creates an important limitation for its use. Despite that, we could find a higher frequency of hCG triggering and progesterone supplementation until later in pregnancy in the smallest units. This probably reflects the reduced experience of the centers that perform fewer reproductive treatments, leading to most defensive ways of working. Concerning differences between private and state institutions regarding IUI cycles, we found no evidence of differences between the type of center and the protocols used. However, our sample is probably underpowered to detect such differences.
The strengths of this study include the presence of a structured questionnaire used uniformly among all participants. The limitations include the absence of all Portuguese reproductive medicine doctor’s representation, but in the real world, 100% participation is never accomplished in any study. Although our sample is small, 51.25% of answers is considered a good response rate for an internet-based survey10. Another important limitation is that this survey does not allow us to know whether there is any difference in luteal phase supplementation, according to the clinical reason motivating an IUI cycle. Our study also does not question the timing of intrauterine insemination after ovulation triggering, which can be different among distinct reproductive units.
A potential bias that is inherent to the study is that doctors that tend to use more luteal phase progesterone supplementation may be overrepresented, because they were more interested in answering the survey. Also, we did not ask about demographic information of our doctors and regional characteristics can have an impact on luteal phase supplementation practices.
In conclusion, our investigation suggests that the vast majority of Portuguese reproductive medicine doctors prescribe similar drugs for ovulation induction when dealing with specific infertility causes. The agreement on the hCG trigger for this kind of cycle is also very high. However, there is some variability concerning luteal phase supplementation and the day of starting and ending progesterone, which is probably a reflection of the existing controversies on this subject.