Introduction
Endometrial hyperplasia (EH) is characterized by a proliferation of endometrial glands, resulting in a greater gland-to-stroma ratio relative to normal proli-ferative endometrium, and is classified according to the presence or absence of nuclear atypia1.
EH is both a marker and a precursor of endometrial cancer, especially EH with atypia2. Its pathogenesis is related to unopposed estrogen secretion resulting in the proliferation of endometrial glands. Despite having been described in the literature, EH resulting from estrogen secretion from an ovarian tumor is rarely encountered in clinical practice.
Granulosa cell tumors (GCTs) of the ovary are a rare form of ovarian cancer, representing 5% of all ovarian cancers, accounting for 70% of all ovarian sex cord-stromal tumors3. Originating from a hormonally active component of the ovarian stroma that produces estrogen, most patients present with abnormal uterine bleeding (AUB), related to hyperestrogenism, and a palpable mass4. Endometrial abnormalities, including EH and endometrial cancer, are found in more than 30% of cases5.
In this report, we describe the case of a 68-year-old woman presenting with recurrent EH and undergoing total laparoscopic hysterectomy and bilateral salpingo-oophorectomy (TLH-BSO), with the diagnosis of an adult GCT.
Case description
An asymptomatic 68-year-old post-menopausal woman was referred for gynecology consultation at our specialized cancer hospital upon finding a 13mm endometrial thickening on routine ultrasound (Figure 1). The patient weighed 66kg, and her height was 1.63m (body mass index of 24.84kg/m2). Medical history was otherwise remarkable only for arterial hypertension, hypothyroidism, and dyslipidemia, and she reported menarche at age 13 and menopause at 55.
She had undergone four hysteroscopies (in 2011, 2013, 2015, and 2018), for post-menopausal uterine bleeding and endometrial thickening on ultrasound (>10mm), and biopsies had yielded focal EH on a polyp, nonatypical EH, atrophic endometrium, and simple endometrial polyp.
This time, in 2020, upon the presence of an asymptomatic endometrial thickness (13mm), the patient was submitted to a new hysteroscopic, with performance of polypectomy and curretage. The histological exam revealing nonatypical EH and so the patient was kept under medical surveillance. Follow-up trans-vaginal ultrasound (TVUS) six months later revealed a normal-sized uterus with a thickened avascular endometrium of 12mm, and both ovaries with normal size and morphology.
Upon discussion of the case with consideration of medical versus surgical treatment, it was decided to perform total hysterectomy with bilateral salpingo-oophorectomy (TH-BSO), taking into consideration that it was a recurrent EH. The patient accepted and the surgery was performed laparoscopically, with no complications. The uterus and both ovaries had an atrophic appearance.
Macroscopic examination of the surgical specimen found a uterus with 90x65x35mm, with endometrial surface irregularity, the right ovary with 25x13x6mm, and the left ovary with 32x21x15mm, which, upon section, contained a 20mm solid nodular formation. Histology revealed an adult granulosa cell tumor (AGCT, figures 2 and 3), limited to the ovary, with intact capsule, without vascular invasion (stage IA by FIGO staging system) and presenting focal atypical EH.
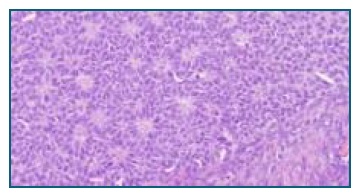
Figure 2 Hematoxylin-Eosin stained section from the Adult Granulosa Cell Tumor, showing an insular growth pattern, with cells surrounding small spaces containing eosinophilic fluid or hyalinized material (Call-Exner bodies). Cytoplasm is scant, and nuclei are uniformly small, and oval, with irregular nuclear membranes and grooving. (HE, 400x)
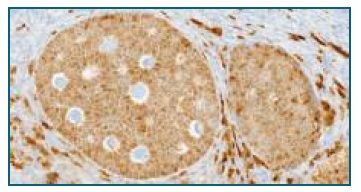
Figure 3 Immunohistochemical stain for inhibin, showing diffuse positivity of tumor cells, and highlighting the insular architecture of the tumor. (Inhibin, 400x)
The multidisciplinary meeting recommended clinical follow-up in outpatient gynecology consultation, and subsequent examination showed no surgical complications. One-month after surgery, lab workup showed no pituitary suppression or hyperestrogenism. Serum concentrations of specific hormones were: follicle-stimulating hormone (FSH): 74.19 mIU/mL; luteinizing hormone (LH): 48.88 mIU/mL; and estradiol: < 12 pg/mL.
Discussion
Ovarian Granulosa Cell Tumors are rare malignant tumors and are subdivided into juvenile and adult types, according to clinical and histopathological characte-ristics. Originating from the hormonally active granulosa cell, these tumors may produce excess estrogen. The adult type (AGCT) usually occurs in postmeno-pausal women, with peak incidence in the fifth decade4. The most common presenting symptoms are an abdominal palpable mass with a mean diameter of 9.4cm, and abnormal uterine bleeding4. The mass approach is usually based on imaging studies such as TVUS. Tumor markers that may be positive are anti-müllerian hormone (AMH), and inhibin B6; CA 125 is usually normal, but, since the diagnosis is usually not suspected they are rarely measured preoperatively. Definitive diagnosis is obtained by histological examination, after surgical removal of the tumor. As with ovarian epithelial tumors, the treatment and staging of ovarian GCTs are mainly surgical. These tumors have a recurrence rate of 10-64%, directly correlating with stage of disease6.
In GCTs, endometrial abnormalities are common, due to estrogen secretion. Endometrial hyperplasia was observed in 29.2% and endometrial cancer in 7.5% of patients7. In cases where fertility-preservation surgery is considered in symptomatic women above 40 years old, an endometrial biopsy is recommended7, hysterectomy not being necessary whenever endometrial abnormalities are not found5.
We herein report the case of a 68-year-old woman submitted to multiple hysteroscopies and uterine biopsies for persistent endometrial thickening on ultrasound, with disparate findings: from atrophic endometrium to focal atypical endometrial hyperplasia.
As the patient did not present relevant risk factors for endometrial cancer, besides increasing age8, she was kept on clinical surveillance for EH. As EH persisted, surgery (TH-BSO) was the chosen treatment, histology revealing an AGCT of the ovary, which had not been suspected from the analysis of imaging studies. This estrogen-secreting tumor was deemed the likely cause of EH persistence. No further surgical staging was performed, since the tumor had been completely excised and the prognosis for early stage AGCT is good, with additional lymph node resection being of limited value6. Follow up imaging studies were postponed by a few months, to diminish the interference of inflammation associated with the surgical procedure.
The association of GCTs and EH is not novel. In the case herein reported, the level of suspicion was very low, because no ovarian tumor was identified in ima-ging studies. The authors consider this case can remind clinicians of the importance to search for a cause in cases with recurrent or persistent endometrial hyperplasia or abnormal uterine bleeding. Serum hormonal concentrations measurement might have been useful in this case, as they would probably have shown a low FSH and a high estradiol level. AMH and inhibin B serum measurements may also be helpful in follow-up, as they have may be elevated months to years before the first symptoms associated with relapse9.















