Introduction
Coronavirus Disease (COVID-19) is an infection caused by a novel coronavirus, called “Severe Acute Respiratory Syndrome Coronavirus 2 - SARS-CoV-2”, which was first identified as respiratory illness, in Wuhan city, Hubei, China1. The World Health Organization (WHO) reported the disease on December 31, 2019, declared COVID-19 a global health emergency on January 30, 20202 and as a Pandemic on March 11, 20203.
The transmission of SARS-CoV-2 from an infected mother to fetus during gestation or delivery seems to be possible, although it appears to occur in a minority of cases, of about 3.2% in large a systematic review4.
The truly occurrence of transplacental transmission, withs its consequences and outcomes, remains uncertain and more studies are needed.
Vertical transmission of SARS-CoV-2 is possible, even if the mother is asymptomatic or presents mild disease.
The diagnosis of neonatal infection is still limited due to the lack of specificity and sensibility of laboratory tests. These can be insufficient to make the diagnosis and improve the management and outcome neonate.
Case report
A 35-year-old pregnant woman, with class I obesity, Gesta III Para II, with two previous pregnancies without major complications and two vaginal deliveries, attended the Obstetrics Emergency Department at 29 weeks and 3 days of gestation, due to generalised itching, more intense on her hands, and also complaining of a mild hypogastric pain. She had past medical history of adenomatous multinodular goiter and microcarcinoma papilar, submitted to right hemithyroidectomy ten months before, and Gestational Diabetes treated with diet and lifestyle changes, in current pregnancy, without relevant complications to the present date.
The pregnant was in prophylactic isolation due to contact with a COVID-19 positive patient. At admission, she was normotensive and the other vital signs within normal parameters. On objective examination, she was found to have erythematous papular lesions on the anterior area of her thighs. From the obstetric evaluation, no changes were observed; the uterine cervix was closed, with a length of 40 mm. The Obstetric ultrasound scan showed a fetus in cephalic presentation, oligoamnios (Amniotic Fluid Index 1,5) and an estimated fetal weight of 1149 grams, corresponding to the 5th percentile of growth by Hadlock formula, with normal Dopplers of the umbilical artery and middle cerebral artery.
After clinical evaluation, blood tests were requested, with liver function and bile acid measurements and a RT-PCR test was performed for detection of SARS-CoV-2.
While waiting for analytic results, the pregnant was again observed due to the appearance of superior edema affecting her lip, without dyspnoea, and was medicated with hydrocortisone, which resolved the angyodema.
Her bloods tests showed an elevation of transaminases (ALT and AST) to more than double the reference values and thrombocytopenia of 95000, without anemia or bile acid elevation. The RT-PCR SARS-CoV-2 was positive.
She was admitted to the obstetrics ward due to hepatic dysfunction, suspected fetal growth restriction and COVID-19 infection, for diagnostic investigation and maternal fetal surveillance. Fetal maturation was initiated with intramuscular dexamethasone.
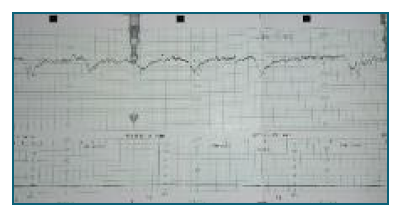
During hospitalization, she was medicated with an antihistamine for symptomatic treatment of pruritus, with good response. Laboratory results showed progressive improvement, with normalisation of liver function and normal platelet count on the 4th day of admission. On that same day, she reported a decrease in the perception of fetal movements and, due to pathological cardiotography (figure 1 and 2), an emergent cesarean section was performed, at 29 weeks and 6 days of gestation, with extraction of a female neonate, 1120 grams (< 1st percentil by Hadlock formula) and Apgar score 5/8/9 at the 1st, 5th and 10th minutes, respectively.
The neonate was admitted to the neonatal intensive care unit due to prematurity and respiratory failure. Umbilical cord blood was tested for SARS-CoV-2 RT-PCR and nasopharyngeal swabs were performed soon after birth and at 48 hours of life - all tests were negative. The neonate needed non invasive ventilatory support with nCPAP for the first two days of life and was breathing spontaneously in room air from day 3. She received parenteral feeding and initiated enteral feeding with irregular tolerance. A peripherally inserted central venous catheter was placed by day 2 of life.
On the 9th day of life a decline in respiratory function and hemodynamic instability was observed, with frequent episodes of bradypnea and bradycardia. There was rapid progression of respiratory failure, needing endotracheal intubation and mechanic ventilation. Despite effective ventilation, the neonate state deteriorated with circulatory failure. Advanced resuscitation maneuvers were performed, with no success, ending with the newborn’s death.
Post-mortem fetal tissue studies revealed non-specific type lymphocytic epicarditis/pericarditis and interstitial myocardial edema and individual myocytes necrosis, associated with chylous effusion (figure 3a-3d), justifying cardiac tamponade. Chronic pleuritis and pulmonary edema were also observed, with rare cells with heterogeneous condensed chromatin, which may relate to viral cytopathic changes in the context of SARS-CoV-2 infection. As the identified pathological condition, in particular non-specific lymphocytic pericarditis associated with pleural effusion and lung injury could translate viral infection, laboratory studies of molecular biology were performed and RT-PCR for Sars-Cov-2 was positive on fetal tissue paraffin blocks (lung and heart).
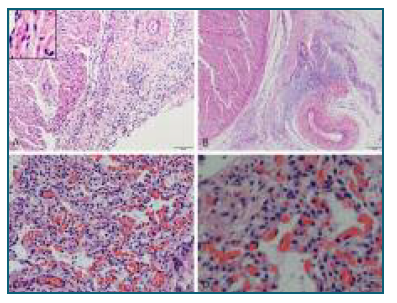
figure 3a-3d Fetal heart (A, B) and lung (C, D) histology: lym-phocytic epicarditis of non-specific type, individual cardiac myo-cyte necrosis and lung endothelial injury with hyaline membrane disease.
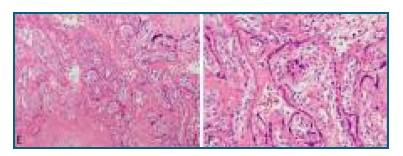
Pathological examination of the placenta showed massive transmural fibrin deposition, with mixed chronic villitis and intervillositis infiltrates and trophoblastic cells necrosis, chronic choriodeciduitis, and fetal vascular injury (figure 3e-3f). The molecular biology study identified, in paraffin block placental tissue samples, infection by SARS-CoV-2 in the context of vertical transmission by maternal COVID-19.
Discussion
Vertical transmission of SARS-CoV-2 is possible, even in mild disease and absence of maternal symptoms. Nonrespiratory symptoms of COVID-19 infections, such dermatologic eruptions and angiodema have been observed5), (6), (7.
The diagnosis of neonatal infection is still limited due to the lack of specificity and sensibility of laboratory tests, such as serologic and virologic tests These can be insufficient to make the diagnosis and improve the management and outcome of pregnancy and the neonate. Therefore placental tissue and/or fetal tissue assays should be performed for definitive diagnose8.
In this report, the maternal symptoms were not typical of COVD-19, but despite this, the vertical transmission of SARS-CoV-2 remains a probable cause of neonate death, as the neonate infection was confirmed in autopsy and placental pathological exam. Fetal growth restriction, also seen in this case (< 1st percentile by Hadlock formula) has been studied as hypothetic consequence of neonatal SARS-CoV-2 infection, but this association remains unclear. Furthermore, the histopathological findings are known to be associated with fetal growth restriction, even in the absence of SARS-CoV-2 infection.
Although postnatal transmission is a possibility, the histological findings of the placenta and the fact that the baby did not contact anyone other than the neonatology team, in which there were no reported cases of COVID-19 infection, make this hypothesis unlikely.
This case report reiterates once again the possibility of vertical SARS-CoV-2 transmission in the third trimester. Cumulative data of this type of transmission is necessary to a have a better knowledge of the impact of COVID-19 on maternal, fetal and neonatal outcomes.