Case
Prenatal diagnosis of TADA is usually incidental in third trimester. The vast majority of cases has a good prognosis, though regular ultrasound follow-up is needed given the associated thrombotic risk1. Maternal diabetes and blood group A are considered high-risk factors1,2. TADA is related with trisomy 21 and 13, as well as, connective tissue diseases, as Marfan and Ehlers-Danlos syndromes3, related with alterations in elastin expression or intima cushioning, or has multifactorial etiology1,2.
We present a male with prenatal diagnosis of TADA. His mother, a 36-year-old woman, with blood group A, has a personal history of hypothyroidism and type 1 diabetes with no history of exposure to teratogens, namely consumption of polyphenol-rich substances, herbal infusions, or nonsteroidal anti-inflammatory drugs4, and has a previous healthy daughter.
At 12 weeks of gestation, fetal ultrasound revealed a small omphalocele with intestinal content and invasive prenatal testing was performed through chorionic villus sampling. The results of QF-PCR and arrayCGH (CGX-HD 180K, PerkinElmer) were both normal. MS-MLPA for Beckwith-Wiedemann syndrome was not possible to perform due to insufficient fetal DNA and early gestational age. Subsequent ultrasound evaluation showed regression of the omphalocele and adequate fetal growth.
Considering maternal diabetes background and the need to exclude other congenital malformations, fetal echocardiogram was performed at 24 weeks. It showed a tortuous ductus arteriosus with a turbulent high velocity flow, with a maximum velocity of 130 cm/s (Figure 1). Regarding the potential thrombotic or rupture risks, weekly echocardiogram was performed until birth, evaluating the ductus morphology and doppler flow, and searching for signs of right ventricular disfunction (tricuspid regurgitation and ventricular dilatation), showing no deterioration. The child was born at 38 weeks by vaginal delivery, with a birth weight of 3150 grams (25th centile) and Apgar score 9/10. Echocardiogram performed on the 3rd day of life, corroborated the prenatal findings, with complete resolution at 1 month of age (Figure 2).
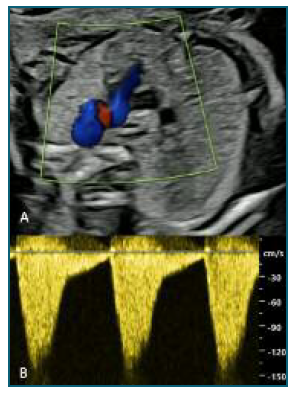
Figure 1 Prenatal ultrasound evaluation, twenty-four weeks gestation prenatal transabdominal echo: A - Three vessel view showing tortuous and aneurismatic ductus arteriosus; B - Flow Doppler with elevated velocity (120-130 cm/s).
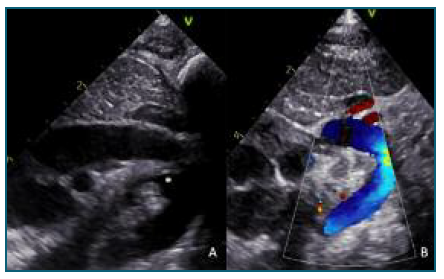
Figure 2 Postnatal ultrasound evaluation (Suprasternal views) A - Three days of life postnatal transthoracic echo: aortic arch with ductus arteriosus (large ampola*) and restriction at pulmonar side; B - One month of life postnatal transthoracic echo: normal aortic arch, no ductus arteriosus (closed).
This case highlights the unusual frequency of TADA in the earlier stages of pregnancy and recalls its most frequently observed follow-up and prognosis.















