Introduction
Office hysteroscopy is the gold standard method for the diagnosis and surgical treatment of intracavitary uterine pathologies. While being well tolerated by the patient in most cases, pain is one of the primary reasons for failure or procedure interruption1,2,3.
Pain perception during the procedure is associated with multiple factors related to the patient and the technique4. Office hysteroscopy avoids patient’s approach in the operating room and contributes with a significant positive impact on patient safety, healthcare quality and decreases the direct and indirect costs associated with the procedure, all of which growing concerns for the highest health bodies such as the WHO5,6. In order to complete a higher number of office hysteroscopies, pain reduction techniques have been used, both pharmacological and non-pharmacological1,7. In particular, various forms of anesthesia, such as paracervical and intracervical, have been studied for this procedure, suggesting the need for further investigation and the definition of new techniques8.
In this article it is provided a detailed description of a local and intracavitary anesthetic procedure which we called “hysteroscopic anesthesia”, comprising an amplification of the “focal-local” technique previously described in the literature9. The purpose of this retrospective study was to evaluate the effectiveness and safety of this method in reducing pain for patients undergoing office hysteroscopy.
Methods
This study was designed as a retrospective assessment considering a group of 859 patients, who underwent office hysteroscopy in two specialized units: in a public hospital between May 25th, 2011, and December 5th, 2019, as well as in a private health center between April 26th, 2016, and November 28th, 2018.
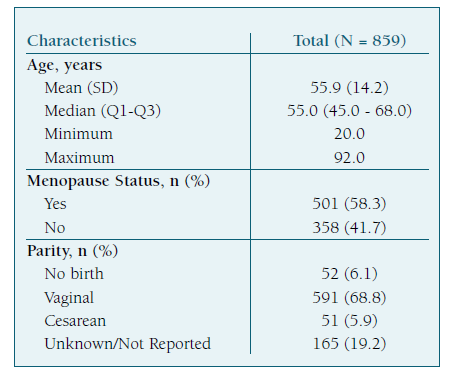
The study population was comprised of women that were elected to perform an hysteroscopy, between 20 and 92 years old, averaging 55.9 years old with a median of 55 years old. A total of 501 patients (58.3%) had already reached menopause and 358 were women of reproductive age (41.7%). As for parity, 52 (6.1%) were nulliparous, 591 (68.8%) had had vaginal births, 51 (5.9%) had undergone cesarean section. There was no parity data on 165 (19.2%) of the patients. (Table I)
The hysteroscopic procedures were performed in an office setting by gynecologists that were experienced in this technique, as well as by professionals in training under the supervision of specialists at all times. The procedures were preceded by a preliminary appointment where the technique was explained with the appropriate level of detail, followed by patient observation and consequent treatment of potential vaginal infections.
The preparation to ensure proper conditions of the cervical canal and endometrium for the procedure was selectively planned, resulting in empiric decision about the need to use misoprostol (intravaginal and/or oral), local estrogens and hormonal contraception.
At the end of the preliminary appointment, eventual enquiries were clarified, and the patients were provided with written information respective to the technique and contact details of the responsible Medical Doctor, who later would perform the hysteroscopy or supervise the professional in training. The authorization to perform surgical procedures and to access clinical information were obtained with the signing of an informed consent.
For all cases, the hysteroscopy was performed using the “see and treat” model with a vaginoscopy approach10, without the use of a speculum or tenaculum, and the distension medium was a 0.9% saline solution, heated to 37°C when at the public hospital and at room temperature when at the Private Health Center. The serum pressure was adjusted on a case-by-case basis, by regulating the inlet and outlet valves of the hysteroscope, varying according to the uterine cavity characteristics and the patient’s tolerance. The pressure used did not exceed the maximum values suggested in the literature11.
The hysteroscope was a Bettocchi Karl Storz® 5 mm rigid with 30° optics. In surgical hysteroscopies, there was also the use of tweezers, scissors and bipolar electrodes (Versapoint®’s Twizzle type), depending on the surgical needs.
During the procedure, according to patient request, a local anesthesia with 1% lidocaine was administered endoscopically. This method that the authors called “hysteroscopic anesthesia”, resorts to the use of an endoscopic needle of 22Ga, 5Fr in diameter, 35 cm in length and 8 mm tip (Cook Williams® Cystoscopic Injection Needle) that is introduced into the operating channel of the hysteroscope, allowing a localized injection of anesthetic in specific pain points identified during the procedure.
This hysteroscopic anesthesia technique is a modification and amplification of Skensved’s “Hysteroscopically Guided Intramyometrial Local Anesthesia - The Focal Local” 9 going beyond the anesthesia of the fibroid base, with infiltration in the polyp bases, in the uterine septum, in the cervical canal and in the utero-sacral area.
In order to define the hysteroscopic anesthesia technique, the following standard procedure was designed considering the different structures and findings:
1. Filling the syringe with 10 to 12 cc of 1% lidocaine, ensuring no refilling during the procedure, to avoid involuntary overdose;
2. Before administration of the anesthetic, regardless of the structure or finding, proceed with aspiration after insertion of the endoscopic needle;
3. When administering 1% lidocaine in the cervical canal (Figure 1), approach the tissue with an angle between 15° and 30° (Figures 2 and 3), similar to an intradermal injection, pointing the needle bevel towards the center of the channel. The puncture should be as shallow as possible, aiming for an anesthetic button;
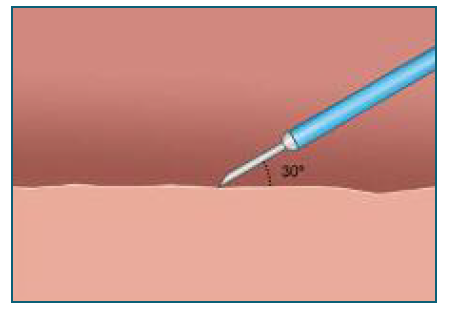
Figure 2 Anesthesia to the cervical canal. Approaching the Cervical tissue with an angle between 15° and 30°, similar to an intradermal injection.
4. When administering 1% lidocaine at the base of fibroids or polyps (Figure 3), approach the base tissue with an angle between 30° and 45° (Figures 4 and 5), similar to a subcutaneous injection, pointing the needle bevel towards the center of the cavity;
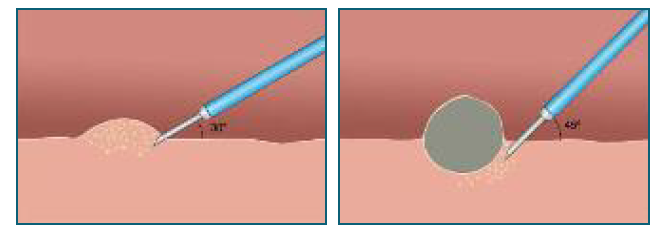
Figure 4 Anesthesia to fibroids and polyps. Approaching the base tissue with an angle between 30° and 45°, similar to a subcutaneous injection.
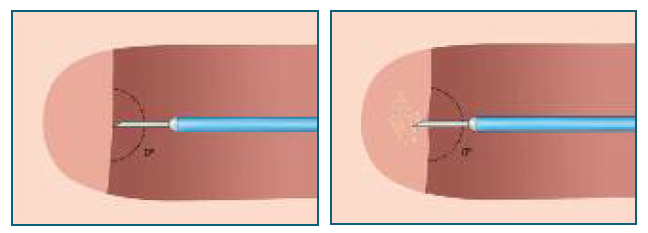
Figure 5 Anesthesia to uterine septum and uteral-sacral area. Approaching the septum wall and uteral- sacral area at an angle as close as possible to 0°.
5. When administering 1% lidocaine to the uterine septum, approach the septum wall at an angle as close as possible to 0° (Figures 5 and 6);
6. When administering 1% lidocaine to the uteral-sacral area (figure 6), it is mandatory a vaginoscopy approach at an angle as close as possible to 0°, so that the uteral-sacral ligaments are infiltrated (Figure 5 and 6).
After the administration of anesthesia according to this standard procedure, the hysteroscopy and eventual surgical procedures were performed and eventually concluded in most cases.
At the end of the hysteroscopy, each patient was presented with a survey inquiring about pain intensity associated with the procedure, before and after hysteroscopic anesthesia, using a numerical scale from 0 to 10, where “0” was absence of pain and “10” was the most intense pain ever experienced. For those who weren’t submitted to hysteroscopic anesthesia the level of pain was also accessed by this scale. For statistical purposes, this study defined cohorts of pain, classified as mild for a score between 0-3, moderate between 4-7 and intense between 8 and 10. The patients were also questioned on the preference to undergo the same procedure under general or locoregional anesthesia in the operating room. After the procedure, the physician had to subjectively assess the perceptiveness of each patient towards the classification, rating the reliability related with the patient’s pain in a -5 (very degraded) to +5 (very favored) scale.
Multiple demographic characteristics of interest were collected from the electronic health records (EHR) as data about the hysteroscopic procedure including the answers collected from the surveys.
The effectiveness of this method, which has the objective of completing the hysteroscopy procedure and reducing pain for the patients, was evaluated comparing the reported pain levels before and after anesthesia, the number of completed procedures with anesthesia, the number of cases in which there was pain reduction after anesthesia and, for these cases, the mean, minimum and maximum pain reduction, and the number of women who would repeat the procedure in-office. The safe of this method was evaluated by the number of complications reported.
For the assessment of factors that could induce misinterpretation of the effectiveness results, this study compared the characteristics of interest as well as the pain intensity reported by patients before anesthesia between the patients that underwent anesthesia and the ones who did not. The patient’s reported pain and the physician’s assessment on the reliability of the patient’s response were assessed for discrepancy.
The approach of the statistical analysis performed in this study compared the continuous variables using t-test, ANOVA, Wilcoxon Rank-Sum test and Kruskall Wallis, and its normality was assessed with the use of the Shapiro Wilk test. The categorical variables were compared using χ2 test and Fisher Exact test.
The characteristics of interest, specifically the relationship between reported pain score, hysteroscopic procedure duration and patients’ age, were assessed with Pearson or Spearman correlations. These characteristics of interest were also assessed for relationship with the pain cohorts defined for this study. In the cases where data was missing, there was no replacement. The significance level was set at p-value = 0.05.
Results
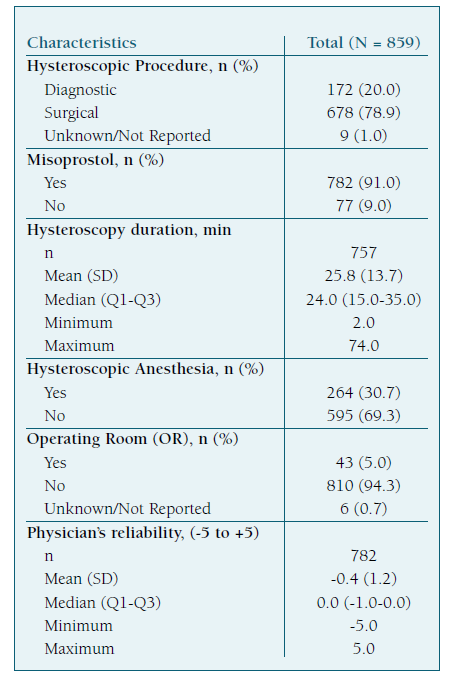
This study addressed 859 procedures, with 172 (20.0%) diagnostic hysteroscopies and 678 (78.9%) surgical hysteroscopies. In 9 cases (1.0%) the diagnostic or surgical nature of the hysteroscopy was unknown. Misoprostol was used for 782 patients (91.0%) in preparation for the hysteroscopy. As for the duration of the procedures, the average was 25.8 minutes and the median was 24.0 minutes per hysteroscopy, with a minimum time of 2 minutes and a maximum recorded time of 74 minutes.
Hysteroscopic Anesthesia was used in 264 patients (30.7%), and no anesthesia was used in the remaining 595 patients (69.3%). Office hysteroscopy, supported by this anesthetic technique, was completed in 94.3% of the cases. Only 43 patients (5.0%) had to be sent to the operating room, due to the inability to complete the procedure in an in-office environment. In 6 cases (0.7%) there was no follow-up record. In 77 cases (9.0%) it was not possible to put on record the Physician’s assessment regarding the patient’s pain perception. (Table II)
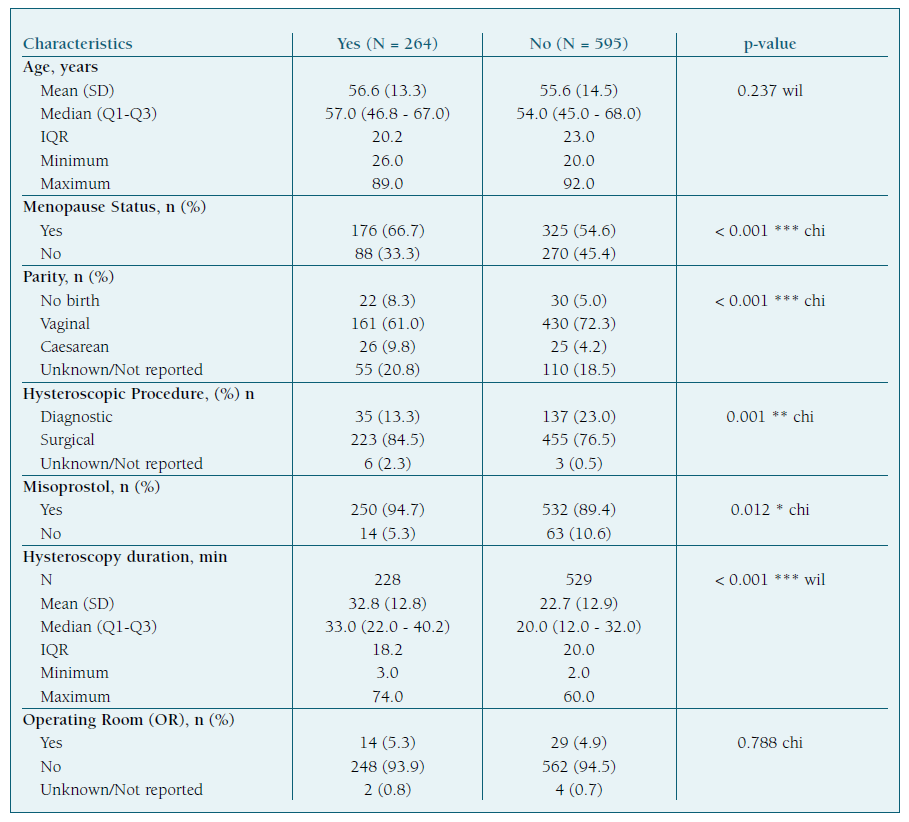
When characterizing the specific group of patients who have requested Hysteroscopic Anesthesia (264 patients) we found an average of 56.6 years old, a median of 57 years old, ranging from 26 to 89 years old. In this group, 66.7% were menopausal, 8.3% were nulliparous, 61.0% had vaginal deliveries, 9.8% had cesarean sections and for 20.8% there is no parity data. 13.3% of the procedures were diagnostic hysteroscopies, 84.5% were surgical hysteroscopies and for 2.3% there was no data. In 94.7% of these procedures misoprostol was given. As for the hysteroscopy time, the average was 32.8 minutes with a median of 33 minutes, ranging from 3 to 74 minutes. Within this group, 93.9% of the hysteroscopies were completed, while 5.3% of the patients were sent to the operating room. In 2 cases (0.8%) there was no data. There were no complications with the anesthetic procedure. For the 243 patients that were asked, 81.0% (197 patients) would undergo the procedure in-office again. In 26 cases (9.8%) it was not possible to put on record the Physician’s assessment regarding the patient’s pain perception.
The group that did not request Hysteroscopic Anesthesia (595 patients) had an average of 55.6 years old, a median of 54 years old, ranging from 20 to 92 years. In this group, 54.6% were menopausal, 5% were nulliparous, 72.3% had vaginal deliveries, 4.2% had cesarean sections and for 18.5% there was no parity data. 23% of the procedures were diagnostic hysteroscopies, 76.5% were surgical hysteroscopies and for 0.5% there was no data. Preparation with misoprostol was performed in 89.4% of cases. As for the hysteroscopy time, the average was 22.7 minutes with a median of 20 minutes, ranging from 2 to 60 minutes. Within this group, 94.5% of the hysteroscopies were completed while 4.9% of the patients were sent to the operating room. In 4 cases (0.7%) there was no data. For the 567 patients that were asked, 96.6% (548 patients) would undergo the procedure in-office again. In 51 cases (8.6%) it was not possible to put on record the Physician’s assessment regarding the patient’s pain perception. (Table III)
Table III Comparison of characteristics of interest between patients that requested Hysteroscopic Anesthesia vs patients who did not request.
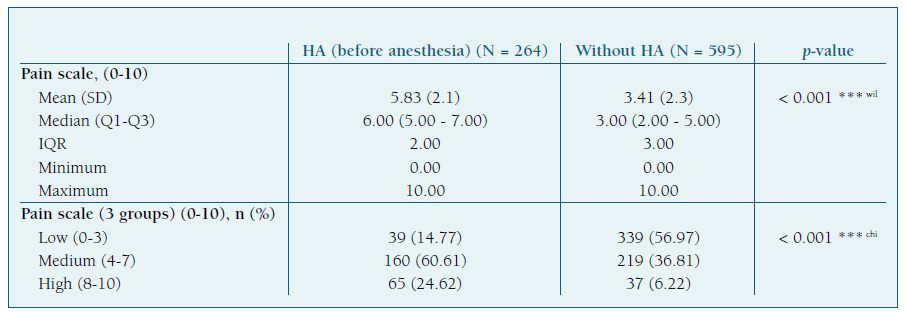
When comparing the initial level of pain reported by patients who requested Hysteroscopic Anesthesia with the level of pain reported by patients who did not request it, there was a significant difference between the two groups, with the mean value of reported pain intensity being 5.83 in the group that underwent AH and 3.41 in the group that did not. (Table IV)
Table IV Comparison of reported pain scores between patients who requested anesthesia (before anesthesia) vs patients who did not request.
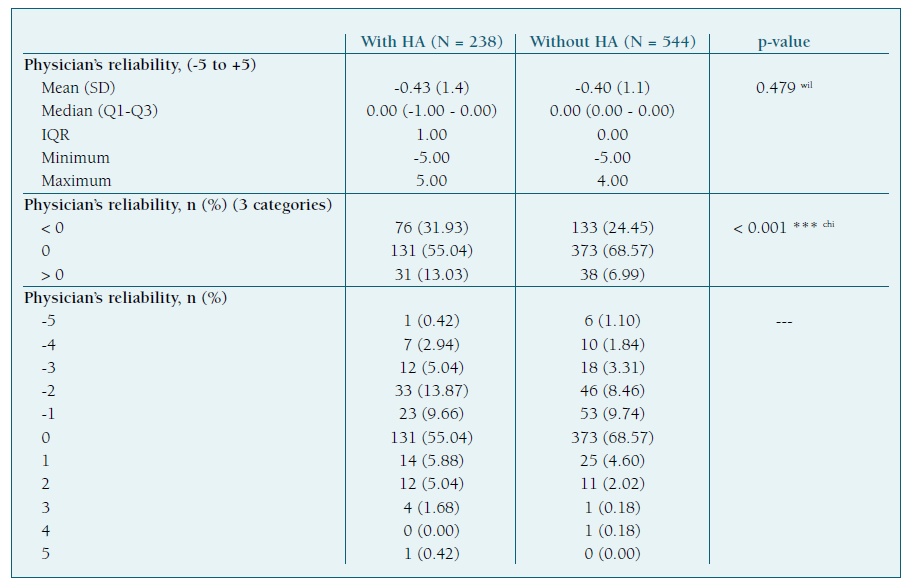
When comparing the Physician’s perception of pain reported by patients who underwent AH with the ones that did not, there was no significant difference. (Table V)
Table V Comparison of physician perception of patients reported pain score between patients who requested anesthesia vs patients who did not request.
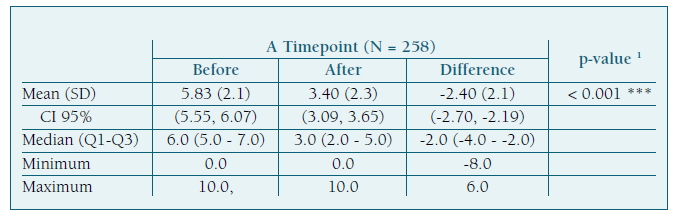
For the group that underwent hysteroscopic anesthesia the level of reported pain decreased by an average of 2.4, from an initial value of 5.8 to 3.4. (Table VI)
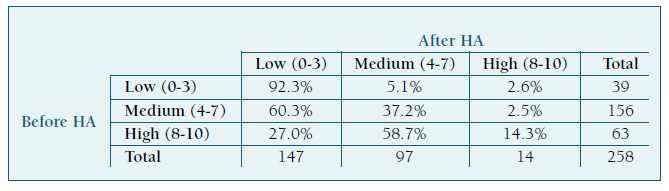
For the cluster defined as low reported pain (0-3), the level of pain reported was maintained or reduced in 92.3% of cases. For the cluster defined as mean, reported pain (4-7) was reduced in 60.3% of cases and maintained or reduced in 37.2% of cases. For the cluster defined as high reported pain (8-10), reported level of pain was reduced in 85.7% of cases and maintained or reduced in 14.3% of cases. (Table VI)
Conclusions
Pain is a subjective perception, but still is one of the main causes for not completing office hysteroscopy, leading to an increase of procedures performed in the operating room, with all the associated costs and risks.
The purpose of this study was to provide a detailed description of a technic we called “hysteroscopic anesthesia” and to evaluate the effectiveness and safe of this method in reducing pain for patients undergoing office hysteroscopy.
The study was exhaustive in presenting the guidelines for proper administration of anesthesia in any circumstance when required by the patient. It also proved that pain can be safely reduced with hysteroscopic anesthesia. The difference in the number of procedures completed with and without hysteroscopic anesthesia was not statistically significant, however greater comfort and reported pain reduction was achieved in the group of patients where hysteroscopic anesthesia was administered. To demonstrate the degree of patient’s satisfaction with the office method, most of them would do the same procedure under the same circumstances.
As shown in the results, there was no significant variance regarding the characteristics, the procedure preparation and the initial level of reported pain between the patients who underwent hysteroscopic anesthesia and the ones who didn’t.
Likewise, the subjective perception of the patient’s pain by the physician, that was used to validate the results, did not indicate a significant variance in the level of reported pain between the two groups of patients.
There were no significant differences between the percentage of procedures completed with and without hysteroscopic anesthesia. However, in women submitted to hysteroscopic anesthesia, the levels of reported pain reduction were significant, including cases where the level of reported pain after anesthesia was very close to those reported by women who did not undergo the anesthetic technique. According to the results, it was also concluded that pain reduction was verified in all pain levels initially reported (low from 0-3, mean from 4-7 and high from 8-10), and its effect was more noticeable in women who had higher initial level of reported pain. The anesthetic procedure was considered safe, with no reported complications. Most patients submitted to office hysteroscopy (96.6% under hysterscopic anesthesia and 81.1% without) would prefer, in case of need to repeat the procedure, to perform it in office under the same circumstances, instead of going to the operating room. This highlights the relevance of the office technique as a way to avoid complications previously reported.
The exclusion of confounding factors - such as the characteristics of the women in the study, technique preparation, type of procedure and pain assessment by the physician - allows to confirm that hysteroscopic anesthesia reduces pain independently. When considering misoprostol effect, as the number of patients to whom it was not administered was very small, this evaluation must be considered with caution and would benefit from a randomized case-control study.
The retrospective nature of this study and the potential for highly unbalanced groups of patients (a limitation of the study design) may reduce the power of the statistical analysis. So that, the main purpose of this study was to generate new hypothesis for subsequent prospective studies rather than to establish definite causality assessments of treatment effects. A prospective, case control randomized study would be recommendable.
Hysteroscopic anesthesia is an effective and safe method for pain control during office procedures. Its use can provide a greater comfort and satisfaction to the patient and allows to complete a great number of procedures without the potentially higher risks associated with the operating room approach.
Author contributions
Mariana Lourenço: data curation, formal analysis, methodology, visualization, writing-original draft. João Mairos: conceptualization, resources, data curation, formal analysis, investigation, supervision, validation, writing-review & editing. Patrícia Di Martino: conceptualization, resources, data curation, investigation, supervision, validation, writing-review & editing.