Introduction
Congenital knee dislocation (CKD), also recognized as genu recurvatum, is an infrequent condition occurring in approximately 1 in 100,000 live births1,2,3. It occurs at a rate 100 times lower than congenital hip dislocation and exhibits a higher prevalence among, females2,3,4. Historical records suggest the first documentation of this anomaly back to 18201.
Characteristic clinical findings of CKD include knee joint hyperextension and forward tibia displacement, heightened transverse skin folds on the anterior knee surface, and femoral condyle protrusion into the popliteal fossa1,4,5.
The causes of CKD can be either intrinsic or extrinsic. Intrinsic causes include genetic syndromes and complex anomalies with no obvious underlying genetic anomaly. Among the extrinsic causes, breech presentation, oligohydramnios and compression may contribute to the etiology1,3,6.
CKD may manifest as an isolated anomaly or in conjunction with other skeletal malformations, or within the spectrum of a congenital syndrome like Larsen syndrome or arthrogryposis multiplex congenita1,2,3.
The most recent classification suggests three types of CKD based on reduction and stability criteria: Type I (55%) is easily reducible, remaining stable in flexion; Type II (31%) is reducible but unstable; and Type III (14%) is irreducible with absence of anterior skin folds5.
The prenatal diagnosis of this condition has not been described extensively. There are 20 cases of CKD with prenatal diagnosis reported in the literature, of which only 7 as an isolated anomaly. The few reports available in the literature describe different management strategies, ranging from a conservative approach to termination of pregnancy1.
Case report
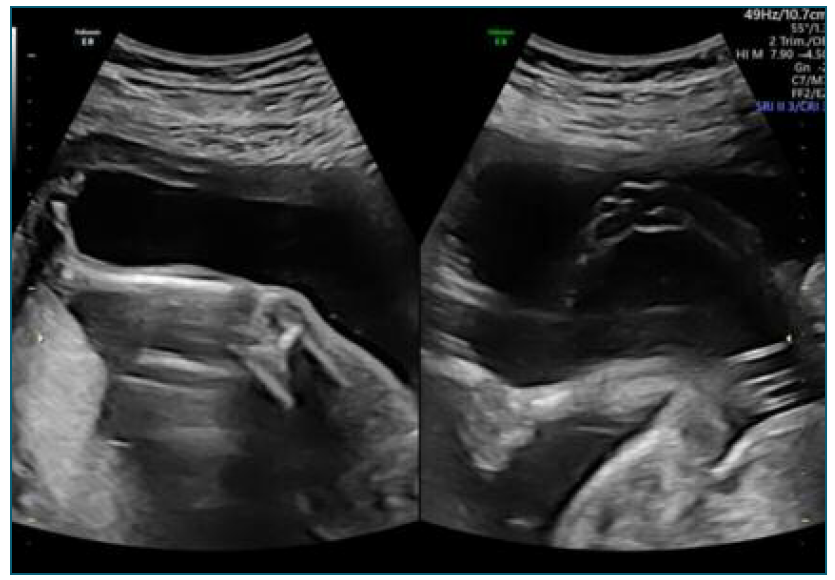
A 35-year-old woman was referred to our department for combined first-trimester screening. Ultrasound scan documented a 13 weeks and 3 days fetus with a 2.3 mm nuchal translucency and normal fetal anatomy. Placental biomarkers were also normal, with a low risk for aneuploidies (Trisomies 13, 18, 21) and preterm pre-eclampsia on combined testing. At 21+3 weeks a second trimester anomaly scan was performed and revealed normal anatomy, including normal bilateral hip/knee relationship, and a low-lying placenta (Figure 1).
During a routine ultrasound assessment performed at 31+4 weeks, an altered orientation of the left knee was observed, with knee overextension and an inverted-convex popliteal fossa, leading to a CKD diagnosis (Figure 2). The position and mobility of all other limbs and joints appeared completely normal, no additional structural anomaly was detected and amniotic fluid volume was normal. Because of these findings, an amniocentesis was performed at a gestational age of 32+0 weeks, and genetic analysis was carried out using array comparative genomic hybridization (aCGH) and a Next Generation sequencing (NGS) panel for collagen disease (including Ehlers-Danlos, Marfan, Loeys-Dietz syndromes and others). The results indicated normal genetic findings for a female fetus. Subsequent serial ultrasound examinations were performed every 2 weeks, confirming an isolated anomaly and normal growth. A fetal echocardiogram was also performed at 37+1 weeks of gestation, with normal results.
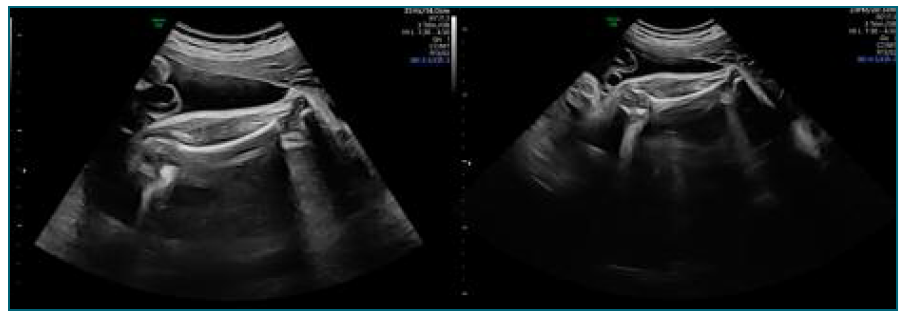
Figure 2 2D - Ultrasound at 31+4 weeks’ gestation revealing left knee overextension and an inverted-convex popliteal fossa.
In an antenatal pediatric orthopedic consultation, all the potential postnatal orthopedic treatment options and expected outcomes were discussed with the parents.
The pregnancy was otherwise uneventful.
A cesarean section was performed at 38+6 weeks after failed induction of labor, delivering a female newborn with a birth weight of 4055 g and 1-min, 5-min, and 10-min Apgar scores of 8, 9, and 10, respectively. Congenital left knee dislocation was confirmed and bilateral acrocyanosis of the forefeet was detected (Figure 3).
The neonate underwent vascular and pediatric orthopedic evaluation in the initial 24-hour period of life, and peripheral arterial occlusive disease was excluded. This was followed by the application of a plaster cast on the left lower limb. Subsequent daily adjustments were made to the plaster cast, facilitating progressive correction of the deformity. By the fourth day of life, the infant achieved a 90-degree flexion. Ultrasound examination revealed a left hip dysplasia.
The infant received routine orthopedic assessments and plaster cast interventions, resulting in symmetric knee flexion by 1.5 months of age and resolution of hip dysplasia by 3 months of age.
At the time of this report, the infant is 6 months old and demonstrates normal flexion in both knees. However, due to his age, an evaluation of his walking ability is not yet feasible.
Discussion
CKD is a well-known anomaly, however, prenatal reports are scarce. To the best of our knowledge, there are only 20 documented cases of prenatal diagnosed CKD in the existing literature.
CKD presents an unknown physiopathology. Nonetheless, various mechanisms appear to play a role, stemming from both intrinsic (genetic syndromes and complex anomalies without apparent genetic underpinnings) and extrinsic factors (breech presentation, oligohydramnios…)1,2,3,6.
This condition may manifest as an isolated finding or coexist with other anomalies, which imply different prognostic outcomes1,2,6.
In a recent systematic review examining prenatal diagnoses of CKD, encompassing the 20 cases reported in the literature, the condition was isolated in 7 cases (35%) and associated with other anomalies in 13 cases (65%). Among the non-isolated cases, 10 (77%) were confirmed to have a genetic basis, while 3 (23%) were not associated with a genetic syndrome despite concurrent structural abnormalities. Genetic testing yielded normal results in all isolated cases for which information was available (4 out of 7). Of the 10 cases with a genetic disorder, five had Larsen syndrome, two had Desbuquois syndrome, one had Escobar syndrome, one had Grebe syndrome, and one had Noonan syndrome1.
Other genetic syndromes characterized by joint hypermobility include Ehlers-Danlos syndrome, Marfan syndrome, spondyloepiphyseal dysplasia, and osteogenesis imperfecta. Non-genetic conditions predisposing to joint hypermobility in the differential diagnosis encompass arthrogryposis multiplex, spastic cerebral palsy, myelomeningocele, and cervical myopathy1,2,3,6.
Referral for an extensive ultrasound assessment, amniocentesis, comprehensive genetic testing (including cytogenetics, array CGH, and gene panel analysis to rule out associated syndromes), and subsequent management is considered essential and recommended1.
The outcome of CKD is heterogeneous, being excellent in isolated cases with early and appropriate orthopedic treatment and less positive for more complex cases1,2.
In the recent systematic review examining prenatal diagnoses of CKD mentioned previously, postnatal treatment was conservative in most cases, with only 2 out of 11 cases (18%) reporting surgical intervention. All isolated cases in which the pregnancy continued had a favorable outcome with no need for surgery, whereas two of the complex cases required, surgery1.
Various treatments for CKD have been described, including closed reduction, serial casting, physiotherapy, minimally invasive or open quadricepsplasty, and femoral shortening. The success rate of manipulation is 77%, and the outcome improves further after treatment with serial casting. However, with late presentation (> 5 weeks after birth), manipulation and serial casting are successful in only 27% of cases, with other cases requiring surgery1. The most common indication for surgery is failure of conservative treatment, which must be performed within 15 months of life and not later than 2 years. Surgical treatment should be performed before the infant begins to stand or put weight on the affected knee, preferably around 6 months of age2,3,6.
Since early orthopedic care improves the outcome, all affected neonates should be referred early (before 48 h postpartum) for expert pediatric orthopedic treatment. Follow-up to older age is needed to evaluate treatment and detect non-identifiable syndromes that might be more evident later in life2.
The presented case achieved a favorable outcome within 1,5 months and at follow-up, despite the severe clinical findings at birth. This was possible owing to multidisciplinary engagement, starting with prenatal diagnosis and orthopedic consultation followed by immediate reduction and casting after birth.
We consider this case significant due to its rarity and prenatal period diagnosis, which facilitated the exclusion of syndromic pathologies and enabled anticipatory care, impacting positively the outcome.
Ultimately, prenatal diagnosis plays a pivotal role in facilitating timely referral to pediatric orthopedic therapy, being a crucial factor in improving postnatal outcomes. Prenatal ultrasound evaluation of the hip/knee relationship is therefore advocated and should be implemented.
Author’s Contribution
Marta Xavier has contributed substantially to the collection and analysis of data, writing of the manuscript and final approval of the version to be published.
Mariana Leal, Mónica Melo, Conceição Brito, and Inês Nunes have contributed substantially to the critical review of the manuscript and final approval of the version to be published.