Pregnancy loss exerts a profound emotional toll on women and their partners1. Most couples seek explanations for their losses and treatments to prevent recurrences. Yet, a substantial number remains unexplained even after detailed investigation2. Cytogenetic analyses of miscarriages have revealed that chromosomal abnormalities of the embryo account for approximately 50% to 65% of spontaneous abortions3.
Hysteroscopic removal of retained products of conception has proven to be effective minimizing damage to endometrial tissue. Transcervical hystero-embryoscopy can be performed simultaneously with hysteroscopic evacuation, offering the advantage of direct visualization of the uterine cavity, gestational sac, detailed embryo morphology, and enabling the direct collection of cytogenetic samples from both the embryo and trophoblastic tissue.
The authors report the case of a 39-year-old woman with a history of recurrent pregnancy loss who presented at 8 weeks of amenorrhea for an appointment to begin her pregnancy surveillance. She was asymptomatic. This was her 5th pregnancy, with a history of one vaginal delivery and three first-trimester miscarriages (IO1031).
Previous investigations of her recurrent pregnancy loss, including thrombophilia screening and karyotype analysis for both partners, showed no abnormalities.
A transvaginal ultrasound performed during the appointment revealed a non-viable twin gestation, with the largest embryo measuring 15.01 mm and the smaller 3.37 mm, corresponding to 7 weeks + 6 days and 6 weeks + 0 days of gestation, respectively. Only one gestational sac was identified, divided by a thin membrane, suggesting a monochorionic diamniotic pregnancy.
A hystero-embryoscopy was performed to complement the recurrent pregnancy loss investigation and to treat retained products of conception. The procedure was done in an inpatient setting under sedation. Following vaginoscopy, a 5 mm continuous flow operative hysteroscope with a 5Fr operative channel (manufactured by Storz®, Tuttlingen, Germany) was used to navigate from the endocervix to the endometrial cavity. The endometrial cavity was inspected, revealing an intact gestational sac. The chorion was opened using microscissors, allowing visualization of two embryos. The amnion was also opened to obtain a detailed view of the larger embryo (Figure 1).
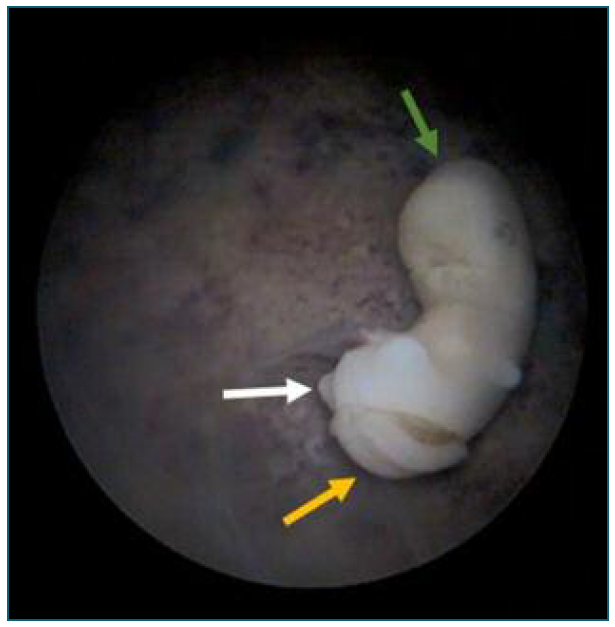
Figure 1 Generic view of the largest embryo. Green arrow pointing at the cephalic extremity and white arrow pointing at caudal extremity. Visible lumbosacral neural tube defect (yellow arrow).
Facial and limb development were consistent with the estimated duration of pregnancy. The observation of a spina bifida was noted, with no other embryonic anomalies (Figure 2). The cord insertion and yolk sac were visible and appeared normal. Biopsies of the embryo and trophoblastic tissue were taken using a hysteroscopic grasper (Biopsy and Grasping Forceps, manufactured by Storz®, Tuttlingen, Germany). A low-resolution microarray-based comparative genomic hybridization (array CGH) and histological examinations were conducted.
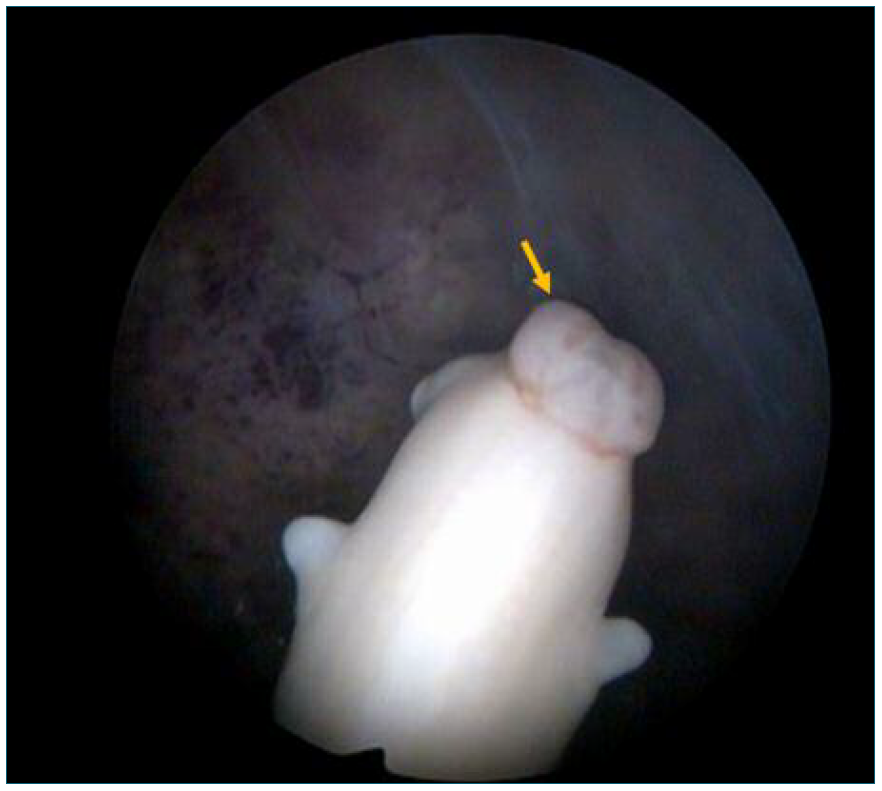
Figure 2 Dorsal view of the largest embryo inside the amniotic cavity revealing a lumbosacral neural tube defect.
Using a hysteroscopic grasper, gestational sac detachment was performed gently separating it from the surrounding uterine lining. Once fully detached, the tissue was removed using the hysteroscopic grasper.
Genetic analysis of embryo and trophoblast were concordant and revealed free trisomies of both 18 and 21. Maternal contamination was excluded. Histological examination of the ovular tissue revealed a hydroptic gestational sac with inconspicuous vesicles, consistent with an apparently complete miscarriage of 7-8 weeks of gestation.
This case illustrates how hystero-embryoscopy can be a valuable tool in investigating pregnancy loss, particularly through its ability to detect morphological anomalies such as neural tube defects that may not be identified by ultrasound in early pregnancy. By enabling direct visualization of embryonic structures, hystero-embryoscopy enhances the precision of diagnoses in cases of structural abnormalities. Moreover, this technique enables the direct collection of cytogenetic samples from both the embryo and trophoblastic tissue, avoiding the risk of tissue contamination4),(5. Additionally, it allows for the simultaneous treatment of retained products of conception, reducing the risk of complications from blind curettage.
Cytogenetic analysis offers significant benefits, particularly in identifying couples with balanced chromosomal rearrangements, enabling targeted genetic counseling. It complements karyotype analysis, which is frequently included in the protocol for investigating recurrent miscarriages and provides further clarity on the causes of pregnancy loss, helping to alleviate the frustration and uncertainty often faced by affected couples3-5.
Thus, hystero-embryoscopy may be particularly valuable for patients with recurrent pregnancy loss, providing the detection of morphological anomalies in early pregnancy, while offering both diagnostic and therapeutic benefits for couples undergoing treatment for retained products of conception.
Author’s contribution
Cristina Oliveira was responsible for conceptualization, methodology, resources, and supervision.
Ana Portela Carvalho contributed to methodology formal analysis and writing - review and editing.
Fabiana Castro conducted the investigation and was responsible for writing of the manuscript and final approval of the version to be published.















