Introduction
Higher-order pregnancies (>2 fetuses), which predominantly arise from ovarian stimulation and assisted reproductive technology (ART)1, can also occur spontaneously, particularly in women of advanced maternal age2. In 2021, the triplet and higher-order multiple birth rate in United States was 80.0 per 100,000 births, with quadruplet births accounting for just 0,000036% of the total3.
Multiple gestations carry a significantly increased risk of maternal, fetal, and neonatal complications, such as: early or late fetal loss, preterm labour and delivery, low birth weight, and increased perinatal mortality1,2,4. Such pregnancies often result in a higher proportion of infants with very low birth weight or prematurity-related complications.
While preventing multiple gestations through better management of ART is ideal, in cases where preventive interventions fail or when spontaneous conception occurs, procedures for multifetal pregnancy reduction have been developed to improve outcomes by redu-cing the number of fetuses4,5. Nonetheless, patient autonomy remains paramount, and some women opt not to undergo reduction despite the risks.
The outcomes of these pregnancies depend on the number of fetuses, the quality of obstetric and neonatal care, and the individual management strategy employed. Given the rarity of quadruplet pregnancies, comprehensive guidelines for their management are lacking.
Here, we present a successful case of a spontaneous quadruplet pregnancy, emphasizing the role of tailored prenatal care and close monitoring.
Case Report
A 32-year-old woman, G3P2, with a history of depression, asthma, and gestational diabetes was referred to Hospital Beatriz Ângelo for first-trimester screening after a spontaneous conception. Initial ultrasound revealed a trichorionic quadrigeminal pregnancy, with two monochorionic/biamniotic fetuses. Multifetal pregnancy reduction was offered to mitigate the risks associated with higher-order pregnancies, but the patient declined. During the second trimester, the patient was diagnosed with gestational diabetes, which was managed effectively with metformin, maintaining reaso-nable glycemic control. Biweekly ultrasounds showed normal fetal growth, no signs of twin-to-twin transfusion syndrome; and only a mild pyelectasis detected in fetus 1.
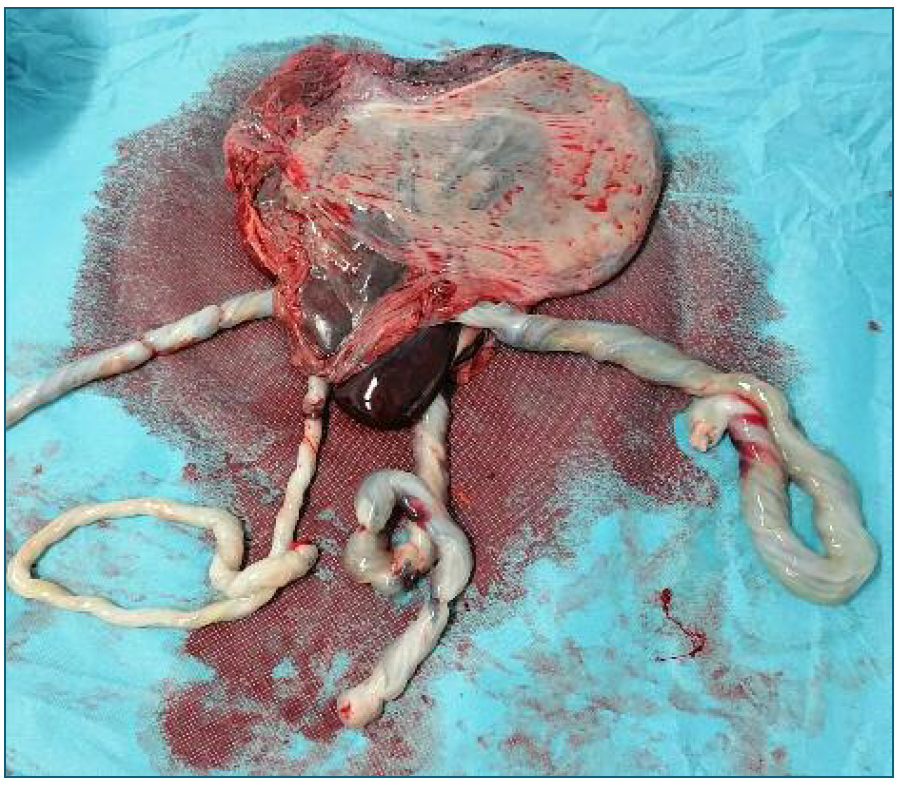
At 28 weeks, a cervical shortening of 14 mm was detected. She was admitted and treated with vaginal progesterone and administered betamethasone to promote fetal lung maturity in anticipation of preterm labor. At 30 weeks, she underwent a cesarean section following the spontaneous onset of labor. Four healthy newborns were delivered: a male weighing 1024 g, a female weighing 1056 g, another female weighing 1076 g, and a second male weighing 1201 g, all with good Apgar scores. Placental examination revealed fused discs and no pathological abnormalities.
The mother had an uneventful postoperative recovery, and the newborns were discharged after 42 to 47 days, following stabilization from complications such as retinopathy, hyaline membrane disease, jaundice, and gastroesophageal reflux.
Conclusion
This case highlights the importance of tailored prenatal care in managing spontaneous higher-order pregnancies. Despite the risks, the patient’s decision to decline multifetal reduction led to the successful delivery of four healthy infants. Vigilant monitoring, early complication detection, and timely interventions were key to the outcome. Sharing cases like this may guide cli-nical decisions, support the development of structured follow-up protocols, and improve care strategies for higher-order multiple pregnancies.
Author’s contribution
Carolina Mendonça performed the literature search, collected the data, wrote the article and is the guarantor and corresponding author. Inês Jorge assisted with the literature search. Diana Martins was involved in providing critical revisions for important intellectual content and assisted with the editing and proofreading of the manuscript.