Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.8 no.4 Lisboa dez. 2012
Unconventional Endovascular Treatment of Iatrogenic Ilio-Cava Fistula*
Tratamento endovascular não convencional da Fistula Ilio-cava Iatrogénica
Clara Nogueira, Rui Machado, Carolina Vaz, Luís Loureiro, José Tavares, Rui Almeida
Angiology and Vascular Surgery Department
Centro Hospitalar do Porto– Hospital Santo António, Porto, Portugal
|ABSTRACT|
Arteriovenous fistula (AVF) following lumbar discectomy is an uncommon, threatening complication. Endovascular treatment is increasing worldwide. A 58-years-old woman was admitted with iatrogenic ilio-cava AVF and right external iliac artery (EIA) occlusion. Several attempts, retrograde and antegrade, to cross EIA occlusion failed, with both guidewires progressing to vena cava. Goose neck snare was used to snare contralateral guidewire (on venous system) and it was exteriorized on femoral artery, followed by EIA angioplasty and endograft exclusion of the AVF. Tips and tricks, like the one described, are essential for any vascular surgeon.
Key-words: arteriovenous fistula, iatrogenic, discectomy, endovascular
|RESUMO|
A fístula arteriovenosa (FAV), pós discectomia lombar, é uma complicação rara, potencialmente grave. O recurso ao tratamento endovascular tem sido crescente. Os autores apresentam o caso clínico de uma doente de 58 anos de idade, com FAV ilio-cava iatrogénica e oclusão da artéria ilíaca externa (AIE) direita. Foram efectuadas várias tentativas de cateterização, retrógrada e anterógrada, do eixo arterial ilíaco direito, com progressão sistemática dos fios-guia para a veia cava inferior. Com o auxílio de um Goose neck snare, foi possível enlaçar o fio guia contra-lateral (que já se encontra no eixo venoso) e recolocá-o no eixo arterial. Procedeu-se a angioplastia transluminal da AIE e exclusão de FAV com endoprótese recoberta. Dicas e truques, como o descrito, são de elevada utilidade para o cirurgião vascular.
Palavras-chave: fístula arteriovenosa, iatrogenia, discectomia, endovascular
INTRODUCTION
Vascular injury during lumbar discectomy is a rare, potentially severe complication. [1,2,3] It occurs more frequently in L4-L5 space1, anatomically corresponding to iliac veins confluence, which is separated from lumbar spine only by the anterior longitudinal ligament. [3.4] Vascular lesions during discectomy can result in acute hemorrhage, arteriovenous fistula (AVF) or false aneurysm.
AVF symptoms may be diversified or even non- existent (up to 50%), with late onset, contributing to delayed diagnosis.[3] Clinical features associated with AVF include high-output heart failure (65%), lower limb edema (39% ), lower limb ischemic symptoms, abdominal/ lumbar pain. On physical examination, a continuous abdominal thrill/ murmur (89%)[2] is frequent. Imaging tests are essential for diagnosis[1,5] and planning treatment. Surgery, classic or endovascular, allows complete resolution of AVF.
CASE REPORT
A 58 years old woman presented with right lower limb (RLL) edema, cyanosis, paresthesias and rest pain, with 6 days evolution. Medical history included lumbar discectomy (L4-L5) 32 days before, apparently without complications. Patient denied fever, chils or sweating.
Abdominal examination revealed a continuous murmur over right quadrants, without perceptible thrill. Right-sided femoral pulse was felt to be weak, in opposite to left lower limb (LLL) which presented wide femoral, popliteal and distal pulses. Ankle / brachial index at RLL was 0.35 and >1 at LLL.
Duplex scan suggested an AVF, confirmed by computed tomographic angiography (CTA): right ilio-cava AVF associated with right external iliac artery (EIA) occlusion. | FIGURE 1 |
| FIGURE 1 | Ilio-cava fistula and right external iliac artery occlusion. White arrow – right common iliac artery | Black arrow – vena cava

An endovascular procedure was attempted, as described below:
> Retrograde common femoral artery (CFA) access was obtained bilaterally, by percutaneous catheterization (5F introducer) on the left and surgical exposure on the right (6F introducer).
> After an unsuccessful attempt to cross EIA occlusion from the right side, in a retrograde approach (guidewire progressing directly to inferior vena cava (IVC)), a crossover antegradely catheterization was attempted, once again, with guidewire advancing directly to IVC.
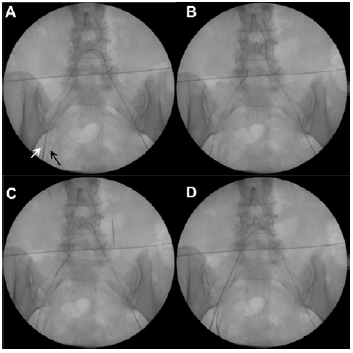
> Goose neck snare was introduced through right CFA, and intentionally progressed to IVC, to snare contralateral guidewire, which already was in IVC. Left guidewire was pulled out through right CFA, crossing right EIA and common iliac artery (CIA). | FIGURE 2 |
| FIGURE 2 | A – guidewire progressing to venous system, in a retrograde or antegrade approach; B – snaring contralateral guidewire, on venous system; C – pushing back contralateral guidewire, through external iliac artery; D – contralateral guidewire exteriorized on femoral artery. White arrow – common femoral artery | Black arrow – common femoral vein
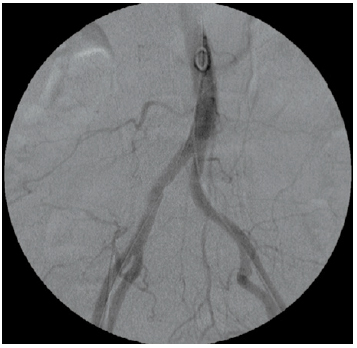
> Aortography revealed non-occlusive thrombus on EIA | FIGURE 3 |, which was managed by CIA and EIA balloon angioplasty (8x40mm and 5x10mm balloon, respectively, under 11F introducer). AVF exclusion was reached after releasing a covered stent (Hemobahn® 9x50mm) in right CIA.
| FIGURE 3 | Non-occlusive thrombus on external iliac artery

> Final angiogram confirmed AVF exclusion and right EIA permeability. | FIGURE 4 |
| FIGURE 4 | Final control after iliac artery angioplasty and arteriovenous exclusion with covered stent Hemobahn®
Patient recovered wide and symmetric RLL femoral, popliteal and distal pulses, with an ankle/brachial index of 1.
Residual paresthesias persisted after the procedure, but significantly improved through the first month.
Lifelong anticoagulation was introduced, due to continuous contact of endograft with venous system.
During 5 years of follow-up, no complications were identified on physical examination, duplex scan or CTA.
DISCUSSION
Lumbar discectomy has a low complication rate (2-6%), being vascular lesions even more rare (0.04-0.14%),[4] and estimated overall mortality of 0.5%. Vascular injury prevalence is probably underestimated, because clinical manifestations are highly variable, resulting in misdiagnosis.[6] Mortality, following vascular injury, has been reported to occur in 15-61% of patients.[7] Chronic AVF is associated with a more benign course, but still with high mortality rates (5-10%).[8] Right-sided iliac artery injury is more frequent (43% vs 29%).[6]
Most abdominal AVF are secondary to rupture/ erosion of an abdominal aortic aneurysm in contiguous venous system.[1,3] Less frequently, are secondary to traumatic and iatrogenic injuries[1] or associated with mycotic aneurysm, connective tissue diseases, Takayasu arteritis, among others.
In present case, taking into account the clinical history and imaging results, it is assumed AVF secondary to lumbar discectomy.
Delayed AVF diagnosis induces late treatment (25% of AVF are detected one year after its emergence).[3] In our case, the association between AVF and EIA occlusion anticipated the diagnosis.
Until mid-90s, conventional surgery was the only therapeutic option, associated with significant bleeding and considerable mortality (up to 34%).[2,3,9] Collateral circulation and diffuse fibrosis around AVF are the main determinants for these results.[1,5] It remains the preferred therapeutic option for acute lesions in unstable patients.[4]
In recent years, endovascular treatment of iatrogenic AVF is rising, even in urgent situations.[10] Endovascular treatment emerges as an equally effective technique and less invasive, with fewer peroperative complications and smaller blood loss.[3,4,10] It is considered the first therapeutic option in chronic iatrogenic AVF,[1,3] which may be corrected with arterial or venous covered stents, embolization, or a combination of both techniques.[1,11] Morbidity with endovascular treatment is reported to be minimal.[6] In a report of 7 patients submitted to endovascular AVF repair, no complications were detected during a median follow up of 8.7 years, reinforcing its durability.[6]
CONCLUSIONS
Vascular injury during lumbar discectomy is a rare complication that can be associated with dramatic consequences.
All surgeons who perform lumbar discectomy should be aware of potential vascular complications, whether acute or chronic.
Endovascular repair is increasingly the first-line treatment for iatrogenic AVF. It is simpler and quicker, on experienced hands. It is also an excellent option in less frequent cases, with higher complexity, like the one presented: AVF associated to EIA occlusion.
REFERENCES
[1] WANG E. et al: Iatrogenic Left Iliac-Caval Fistula: Imaging and Endovascular Treatment. AJR 2004; 183: 1032-1034. [ Links ]
[2] FORBES T. et al: Endovascular Management of a Chronic Iliac Arteriovenous Fistula Following Lumbar Discectomy. EJVES Extra 2004; 8: 116-118. [ Links ]
[3] GALLERANI M. et al: High output heart failure due to an iatrogenic arterio-venous fistula after lumbar disc surgery. Acta Neurochir 2007; 149: 1243-1247. [ Links ]
[4] ERKUT B. et al: Iatrogenic vascular injury during to lumbar disc surgery. Acta Neurochir 2007; 149: 511-516. [ Links ]
[5] BRAWLEY J. MD, MODRALL J. MD: Traumatic Arteriovenous Fistulas. Vascular Surgery, Rutherford RB et al, 6th edition; cap.1112: 1619-1626. [ Links ]
[6] CANAUD L, HIRECHE K et al: Endovascular repair of aorto-iliac artery injuries after lumbar-spine surgery. Eur J Vasc Endovasc Surg 2011; 42, 167-171. [ Links ]
[7] GOODKIN R, LASKA LL. Vascular and visceral injuries associated with lumbar disc surgery: medicolegal implications. Surg Neurol 1998; 49: 358-370. [ Links ]
[8] PAPADOULAS S, KONSTANTINOU D et al: Vascular injury complicating lumbar disc surgery: a systematic review. Eur J Vasc Endovasc Surg 2002; 24: 189-195. [ Links ]
[9] DAVIS P. MD et al: Aorto-Caval and Ilio – Iliac Arteriovenous Fistulae. Am J Surg 1998; 176: 115-118. [ Links ]
[10] JIN SC, PARK SW et al: Management of proximal iliac artery injury during lumbar discectomy with stent graft. J Korean Neurosurg Soc 2012; 51: 227-229. [ Links ]
[11] CRONIN P. et al: Venous Covered Stent: Successful Occlusion of a Symptomatic Unternal Iliac Arteriovenous Fistula. Cardiovasc Intervent Radiol 2002; 25: 323-325. [ Links ]
E-mail: rmvasc@gmail.com
Notas
*Presented at 8th Portuguese Society Congress of Angiology and Vascular Surgery, 28th June 2008, Cascais, Portugal [ Links ]














