Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.13 no.1 Lisboa mar. 2017
CASO CLÍNICO
Pseudoaneurisma da artéria pulmonar: uma lesão vascular rara após cateterismo cardíaco direito
Pulmonary artery pseudoaneurysm: a rare vascular lesion after right heart catheterization
André Gomes*, Paula Campos*
*Serviço de Imagiologia Geral, CHLN — Hospital de Santa Maria
RESUMO
Os pseudoaneurismas da artéria pulmonar podem ser causados por infecção, trauma, lesões neoplásicas ou iatrogénicas, tal como a ruptura durante cateterismo cardíaco direito. O quadro clínico pode variar desde um achado incidental até uma hemor- ragia severa com hemoptise massiva. Apresentamos um caso de uma mulher de 67 anos com antecedentes de escleroder- mia que desenvolveu uma hemoptise massiva após cateterismo cardíaco direito. A angiografia por tomografia computorizada demonstrou um pseudoaneurisma no ramo segmentar basal posterior da artéria pulmonar no lobo inferior esquerdo. A tomo- grafia computorizada permite o diagnóstico, localização e caracterização do pseudoaneurisma, bem como fornece informações importantes para o planeamento terapêutico. Sem tratamento, os pseudoaneurismas podem aumentar ou sofrer ruptura. Embora uma complicação rara, os pseudoaneurismas da artéria pulmonar associam-se a importante morbilidade e mortalidade.
Palavras-chave: Tomografia Computadorizada Multidetectores; Falso Aneurisma; Doença Iatrogénica; Cateterismo de Swan-Ganz
ABSTRACT
Pulmonary artery pseudoaneurysms may be caused by infection, trauma, neoplasm or iatrogenic lesions, such as pulmo- nary artery rupture during right heart artery catheterization. Clinical presentation can range from an incidental finding to a life-threatening bleeding with massive hemoptysis. We present a case of a 67 year old woman with systemic sclerosis that developed massive hemoptysis after right heart catheterization. Computer tomography angiography showed a pulmonary artery pseudoaneurysm in the posterior basal segmental branch of the left lower lobe. Computer tomography angiography usually allows pseudoaneurysm diagnosis, localization and characterization and can aid in therapeutic procedure planning. Without treatment pseudoaneurysms may enlarge or rupture. Although a rare complication, pulmonary artery pseudoa- neurysms are associated with high morbidity and mortality, and should not be missed.
Keywords: Multidetector Computed Tomography; Aneurysm, False; Hemoptysis; Iatrogenic Disease; Catheterization, Swan-Ganz.
INTRODUÇÃO / INTRODUCTION
A pseudoaneurysm is defined as an arterial dilatation that does not comprise all of its wall layers, thus it is at a higher risk of rupture when compared to a true aneurysm. Although rare, pulmonary artery pseudoaneurysms (PAP) have high morbidity and mortality and should not be missed. PAPs can have different etiologies depending on what caused the arterial wall damage, such as infection, trau- ma, neoplasm or iatrogenic lesion 1. Tuberculosis, pyogenic bacteria or fungi can cause PAPs. When secondary to tuber- culosis, they are called Rasmussen aneurysms, usually found in the upper lobes. Mycotic aneurisms and pyogenic bacteria PAPs are more frequently diagnosed in intrave- nous drug users and are associated with endocarditis and septic embolization. Penetrating thoracic injuries, such as stab or gunshot wounds, are the most common traumatic cause PAP 2. Pulmonary neoplastic lesions, either primary or more rarely secondary, can erode an arterial wall leading to a PAP formation. Iatrogenic lesions are the most frequent cause of PAPs and include right heart and pulmonary artery catheterization, chest tube insertion, pulmonary biopsies and cardiothoracic surgery 3. Clinical presentation of a PAP can range from an incidental finding to a life-threatening bleeding with massive hemoptysis.
CASO CLÍNICO / CLINICAL CASE
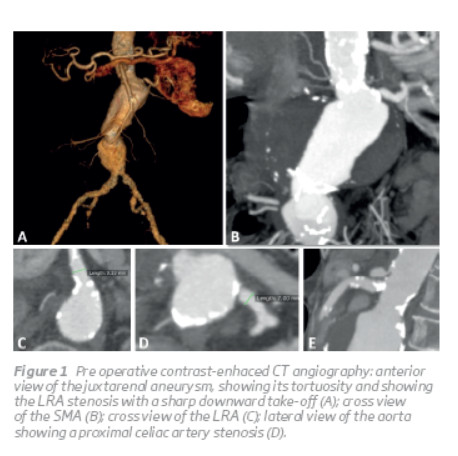
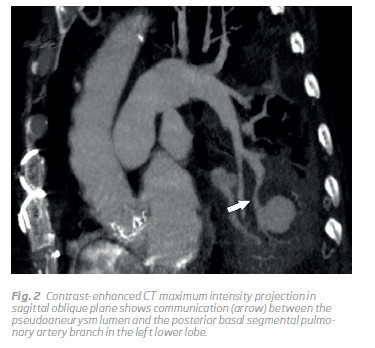
A 67 year old woman, with a background of systemic scle- rosis (diagnosed 19 years ago) with pulmonary fibrosis, cardiac insufficiency and gastrointestinal involvement, and open-heart aortic biologic valve replacement to treat aortic stenosis in 2014, was referred for an elective right heart catheterization due to pulmonary hypertension. During the procedure she presented with massive hemoptysis and hemodynamic instability leading to a cardiopulmonary arrest. After tracheal intubation and successful cardiopul- monary resuscitation she was admitted to an intensive care unit. Two bronchoscopic examinations were performed within 24hours, withoutactivebleedingvisualization. Three days later she presented with a new hemoptysis episode, hemoglobin level drop and hemodynamic instability promp- ting an urgent thoracic computer tomography angiography (CTA) scan request. It revealed a pseudoaneurysm (fig. 1) in the left lower pulmonary lobe with 28mm diameter and an eccentric thrombus, surrounded by parenchymal consoli- dation. Communication with the posterior basal segmental pulmonary artery branch confirmed a pulmonary artery pseudoaneurysm, which is better depicted in maximum intensity projection sagittal oblique image (fig. 2). Some adjacent bronchi had their lumina filled with content, presu- mably blood. Bilateral pleural effusion, mediastinal adeno- pathies and esophageal dilatation were noted. The patient evolved favorably with conservative management, and no complications or other hemoptysis episodes were reported. Four and nine days, respectively, after the first exam, other CTA scans demonstrated aneurysm stability.
DISCUSSÃO / DISCUSSION
Pulmonary artery rupture is a rare complication of pulmo- nary artery catheterization. It has been reported in 0,031% cases in a study with 32.442 patients 4. When bleeding is limited by thrombus or surrounding parenchyma, it can lead to a PAP formation. Known risk factors include fema- le and older (more than 60 years old) patients, steroid use and hypothermia 5. Fibroproliferative vasculopathy and mainly microvascular abnormalities are present in systemic sclerosis 6. However, we didn't find an association between Pseudoaneurisma da artéria pulmonar: Uma lesão vascular rara após cateterismo cardíaco direito systemic sclerosis and pseudoaneurism formation in the literature, and to the best of our knowledge, this is the first described case of a PAP in a patient with systemic sclerosis.
CTA usually allows PAP diagnosis, localization and characte- rization. A pseudoaneurys misseenasaroundorovalopacity with equivalent enhancement when compared to adjacent vessels, and in continuity with an arterial branch. This helps to distinguish a PAP from pulmonary infarct or parenchymal consolidation after pulmonary artery catheterization 7. When a patient presents with hemoptysis, urgent CTA is as accurate as bronchoscopy in detecting the site of bleeding 8, helps to identify the underlying cause and the effects of hemorrhage on lung parenchyma. Multiplane reformatted images (Fig. 2) are also a valuable tool in exam interpretation and can aid in therapeutic procedure planning 9. The treat- ment of choice is more frequently endovascular emboliza- tion as it is proven to be a safe and effective alternative to surgery 10. Without treatment, PAPs may enlarge or rupture, with mortality reaching 100% 11. Nevertheless, small pseu- doaneurysm may be successfully managed conservatively 12.
CONCLUSÃO/ CONCLUSION
Although a rare pathology, pulmonary artery pseudoa- neurysms can have distinct etiologies, namely iatrogenic lesions. Computer tomography angiography is an excel- lent imaging modality to diagnose and characterize these lesions. Due to pulmonary artery pseudoaneurysms asso- ciation with high morbidity and mortality, they should not be missed. Treatment options include conservative mana- gement and surgical procedures, however endovascular embolization is the current preferred choice.
BIBLIOGRAFIA
1. Nguyen ET, Silva CI, Seely JM, et al. Pulmonary artery aneurysms and pseudoaneurysms in adults: findings at CT and radiography. AJR Am J Roentgenol. 2007;188(2). doi:10.2214/AJR.05.1652. [ Links ]
Quartey B, Jessie E. Pulmonary artery and vein pseudoaneurysm after gunshot wound to the chest. J Emerg Trauma Shock. 2011;4(2):313. doi:10.4103/0974-2700.82235. [ Links ]
Lafita V, Borge MA, Demos TC. Pulmonary artery pseudoaneurysm: Etiology, presentation, diagnosis, and treatment. Semin Intervent Radiol. 2007. doi:10.1055/s-2007-971202. [ Links ]
Kearney TJ, Shabot MM. Pulmonary artery rupture associated with the Swan-Ganz catheter. Chest. 1995;108(5):1349-1352. [ Links ]
Dieden JD, Friloux LA, Renner JW. Pulmonary artery false aneurys- ms secondary to Swan-Ganz pulmonary artery catheters. AJR Am J Roentgenol. 1987;149(5):901-906. doi:10.2214/ajr.149.5.901. [ Links ]
Pattanaik D, Brown M, Postlethwaite AE. Vascular involvement in systemic sclerosis (scleroderma). J Inflamm Res. 2011. doi:10.2147/ JIR.S18145. [ Links ]
Ferretti GR, Thony F, Link KM, et al. False aneurysm of the pulmonary artery induced by a Swan-Ganz catheter: clinical presentation and radiologic management. AJR Am J Roentgenol. 1996;167(4):941-945. doi:10.2214/ajr.167.4.8819388. [ Links ]
Revel MP, Fournier LS, Hennebicque AS, et al. Can CT replace bron- choscopy in the detection of the site and cause of bleeding in patients with large or massive hemoptysis? AJR Am J Roentgenol. 2002;179(5):1217-1224. doi:10.2214/ajr.179.5.1791217. [ Links ]
Bruzzi JF, Remy-Jardin M, Delhaye D, et al. Multi-Detector Row CT of Hemoptysis. Radiographics. 2006;26(1):3-22. doi:10.1148/ rg.261045726. [ Links ]
Karak P, Dimick R, Hamrick KM, et al. Immediate transcatheter embolization of Swan-Ganz catheter-induced pulmonary artery pseudoaneurysm. Chest. 1997;111(5):1450-1452. [ Links ]
Rudziński PN, Demkow M, Michałowska I, et al. Endovascular treat- ment of PA pseudoaneurysm caused by Swan-Ganz catheter. Adv Interv Cardiol. 2014;1(3):66-70. doi:10.5114/pwki.2014.41476. [ Links ]
Rouquier J, Arrivé L, Masini JP, et al. [Spontaneous resolution of asymptomatic false aneurysm of the pulmonary artery induced by Swan-Ganz catheter]. J Radiol. 2001;82(12 Pt 1):1732-1734. [ Links ]
Correio eletrónico: astgomes@gmail.com (A. Gomes).
Recebido a 02 de novembro de 2016;
Aceite a 11 de dezembro de 2016.














