Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.13 no.3 Lisboa dez. 2017
CASO CLÍNICO
Cystic adventitial disease of the popliteal artery presenting as acute limb ischemia : popliteal artery's cad presenting as ali
Doença adventicial quística da artériapoplítea — apresentação como isquemiaaguda de membro
Duarte Rego1, Paulo Almeida, Rui Almeida
1Angiology and Vascular Surgery Department of Centro Hospitalar do Porto — Hospital de Sto. António, Porto
Autor para correspondência
ABSTRACT
Introduction: Cystic adventitial disease is a rare cause of intermittent claudication. Its presentation as acute limb ischemia is exceedingly rare. This disease is caused by the growth of multiple cysts within the adventitia. Although its etiopathogeny isn't fully understood most evidence supports an embryonic defect during the development of non-axial arteries. Treatment includes several options: adventitial layer excision, percutaneous aspiration of the cysts and segmental arterectomy with bypass.
Methods: We present a case of acute limb ischemia caused by popliteal cystic adventitial disease.
Clinical Case: A 60 years old male presented with acute limb ischemia of the right leg. Duplex ultrasound showed a tight stenosis of the popliteal artery caused by adventitial cysts. The patient was intervened: from a posterior approach an excision of the cysts and adventitial layer was performed with total recovery of foot's perfusion and pedal pulse. After 18 months of follow-up the patient is asymptomatic without imagiological evidence of recurrence.
Conclusions: Due to the disease's rarity there are no studies designed to compare the different treatment strategies for this pathology. However, the available data from case series shows that the surgical technique chosen for this patient presents very good results and, therefore, it seems to be a good therapeutic option assuming a patent popliteal artery without intimal lesion. Clinical presentation as acute limb ischemia isn't described in the literature and isn't today understandablebecause the factors affecting mucin secretion rate by cyst's mesenchymal cells are unknown.
Keywords: Peripheral Arterial Disease; Cystic adventitial disease; Popliteal artery; Cystic arterial disease
RESUMO
Introdução: A doença adventicial quística é uma causa rara de claudicação intermitente. A sua apresentação como isquemia aguda de membro é ainda mais incomum. Esta patologia é causada pelo crescimento de múltiplos quistos na túnica adventícia. Apesar de a sua etiopatogenia não estar totalmente esclarecida a maioria da evidência científica aponᆳta para um erro ocorrido durante o desenvolvimento embrionário das artérias não axiais. Existem várias opções teraᆳpêuticas, nomeadamente, a excisão da túnica adventícia, a aspiração percutânea dos quistos e a exérese segmentar da artéria afetada com reconstrução arterial por pontagem.
Métodos: Apresentamos um caso de isquemia aguda de membro causada por doença adventicial quística da artéria poplítea.
Caso Clínico: Doente do sexo masculino com 60 anos de idade observado no Serviço de Urgência por quadro clínico compatível com isquemia aguda do membro inferior direito. A avaliação com eco-doppler revelou uma estenose severa da ᆳdagem poplítea posterior foi realizada a exérese dos quistos em conjunto com a túnica adventícia com recuperação da normal perfusão do pé com pulsos pedioso e tibial posterior presentes. Aos 18 meses de follow-up o doente encontra-se assintomático sem evidência imagiológica de recidiva.
Conclusões: Devido à raridade da doença não existem estudos que comparem as diferentes estratégias terapêuticas. No entanto, a evidência científica procedente de séries de casos clínicos revela que a técnica cirúrgica escolhida para este doente associa-se a bons resultados constituindo por isso uma boa opção terapêutica desde que a artéria poplítea esteja permeável sem significativa lesão intimal. A apresentação clínica sob a forma de isquemia aguda de membro não está descrita na literatura científica e não é, de momento, totalmente compreensível já que se desconhecem os fatores que regulam a secreção de mucina pelas células mesenquimatosas dos quistos adventiciais.
Palavras-chave: Doença arterial periférica; Doença adventicial quística; Artéria poplítea; Doença arterial quística
INTRODUCTION
Cystic adventitial disease (CAD) is a rare pathology that was first described in 1947 affecting an external iliac artery(1). CAD is located in the popliteal artery in 85–90% of cases, usually is unilateral, however, cases of bilateral disease have been described(2). It usually affects male patients (ratio of 15:1), and the typical age is mid-40s(3). The classic prevalence of cystic adventitial disease is reported around 1:1200 cases of claudication(4). This disease results from the development of cysts in the adventitial layer of the blood vessel wall that may result in arterial stenosis and compromise of blood flow.
Its clinical presentation is rather uncharacteristic and the diagnosis is usually based on the absence of the traditional cardiovascular risk factors on a young claudicant patient. The confirmation of this diagnosis can be based in several methods such as duplex ultrasound (DUS), angioCT, MRA and angiography. Although MRA is considered the gold standard method, because it clearly describes cysts anatomy and its relation to the artery(5,6), DUS can provide enough information to confirm the diagnosis and plan a therapeutic intervention(7).
We present a case of popliteal adventitial disease and discuss the various therapeutic options.
CLINICAL CASE
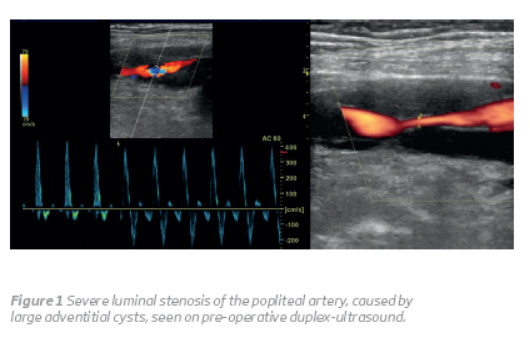
A 60 year old male was first observed for right leg edema and light, diffuse, calf pain that aggravated with exertion but that sometimes was also present at rest. He had hypertension and dyslipidemia but no other atherosclerotic risk factors such as smoking or diabetes. Physical examination was normal. DUS excluded popliteal DVT but revealed several cystic lesions along the second segment of the popliteal artery's (P2) wall without causing luminal stenosis even with knee flexion. His pain wasn't suggestive of vascular claudication (and the patient had had an episode of recent strenuous physical exertion) and was discharged and referred to vascular outpatient clinic. The patient was re-observed 2 weeks after and was completely asymptomatic with unchanged DUS findings. One month later he was reevaluated at outpatient clinic and complained of a right poikilothermic, and thermal hypoesthesic, foot. Pedal pulse was diminished with extension of the leg and abolished with flexion of the knee (Ishikawa's sign(8). There was no motor deficit. DUS showed enlarged adventitial cysts surrounding the popliteal artery with severe lumen stenosis (Figure 1), these findings were confirmed with angioCT and peri-operative angiography (Figure 2).

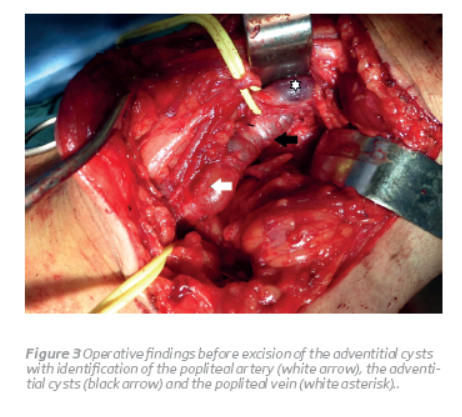
Given the rapid progression of the cystic lesions with a near total occlusion of the popliteal artery it was decided to perform an urgent surgical intervention before thrombosis could occur. From a posterior approach the popliteal artery and the adventitial cysts were exposed (Figure 3).
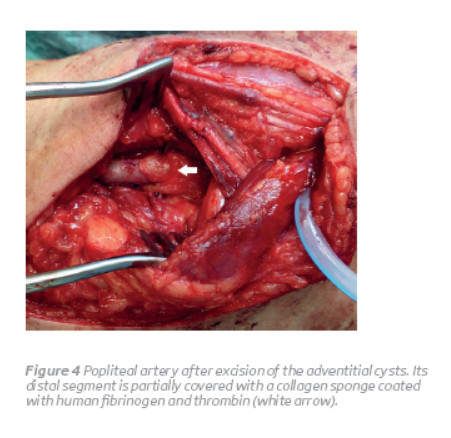
Then, total excision of P2's adventitia and its cysts was done (an “exarterectomy” as named by van Rutte et al(9))(Figure 4). Surgery was technically complex because excision of the adventitia led to significant arterial wall weakening and some minor arterial lacerations had to be corrected with interrupted polypropylene sutures. Completion angiography was performed showing a patent popliteal artery without stenosis both with a flexed and an extended knee. The patient had an uneventful hospital stay and was discharged 4 days after surgery with normal pedal pulse, both with an extended or bent knee.
A portion of the excised cyst was sent to histological analysis. Its wall was described as resembling the wall of a Baker's cyst with fibrous areas and areas of myxoid degeneration.
Unfortunately, immunohistochemistry analysis of the fluid was not performed.
At 18th month of follow- up the patient remains asymptomatic and DUS shows a patent popliteal artery without residual/recidivant stenosis or aneurysmal degeneration.
DISCUSSION
Due to its rarity, CAD's natural history isn't completely understood. Although the cause of CAD is still unclear, four theories to explain this disorder have been proposed(10,11). The theory of CAD as a myxomatous systemic degenerative condition associated with a generalized disease was postulated initially. Repeated trauma theory had its origin due to the proximity of the popliteal artery to the knee joint, which would presumably stretch or distort the vessel, causing destruction and cystic degeneration of the adventitia wall. Repetitive trauma could also cause small detachments from the media of the artery, with intramural bleeds generating the cystic changes. Another theory is the synovial (or ganglion) hypothesis, which suggests that adventitial cysts arise as capsular synovial structures from the adjacent joint that migrate along vascular branches into the adventitia of the major vessel. The developmental theory has been postulated by Levien and Benn(11) as a unifying hypotheses; it presents CAD as an embryologic abnormality, in which undifferentiated mesenchymal cells are included in the artery wall during the embryologic development of the vessel; these cell remnants will subsequently secrete the mucoid material that fills the adventitial cysts. This last theory is nowadays the most commonly accepted.
CAD typically presents as rapidly progressive unilateral, intermittent, calf claudication with a prolonged time of recovery. Rarely, CAD presents as acute-onset limb pain due to bleeding in the cyst or rupture of the cyst(12), or, alternatively, as acute limb ischaemia due to thrombosis of the affected arterial segment(13). Our patient presented a subacute evolution of its disease that coincided with a period of worsening of symptoms related to a chronic gonarthrosis. In fact, the patient's first complaint, of leg edema, was probably secondary to his aggravated gonarthrosis since there was no venous compression on DUS and the subsequent surgery definitely excluded associated venous adventitial disease (there are rare descriptions of venous CAD and the involvement of the popliteal vein is extremely rare(14)) Although today's most accepted ethiopatogeny defends an embryologic defect it also conceives the presence of reminiscent channels between arterial cysts and the knee joints and this could explain the coincident worsening of the patient's CAD and gonarthrosis by the enlargement of the popliteal cysts due to increased pressure in synovial cysts (the patient had a documented synovial cyst that was observed during surgery). The above mentioned channels are frequently observed in patients with CAS and were described in several published case reports(15,16,17,18).
The subacute evolution of this case also conditioned our timing of intervention; the rapid progression of the stenosis due to enlarging cysts presented a risk of arterial thrombosis that, due to intimal injury, could potentially worsen a revascularization procedure's prognosis.
Various treatments have been proposed and attempted for CAD. The first cases of CAD were treated by resection of the affected arterial segment and replacement by an interposition graft, either venous(19), arterial homograft(20) or synthetic graft(21). In the 1960s, alternative treatments were reported, including excision of a cyst with the outer layer of the arterial wall(8,22) and percutaneous needle aspiration of cysts in the wall of the popliteal artery(23,24). Although the described results for patients treated with resection and vein graft interposition are very good(9), which is not unexpected since this is a disease that generally maintains a preserved tibial runoff, this treatment option implies a more extensive surgical aggression to the patient due to vein harvesting. Besides, in order to allow the operation in ventral decubitus from start to end of the surgery the availability of a good quality small saphenous vein is advised. Given these arguments we opted to perform excision of the cysts with the outer layer of the arterial wall. This is a more recent surgical therapy for CAD that is also associated with excellent clinical results. It implies a patent popliteal artery and integrity of the medial layer of the arterial wall. Endovascular therapy was not considered because it is associated with poor results in CAD(25,26); one of the few, published, successful cases of endovascular treatment was a patient with recurrent popliteal CAD with restenosis after surgical cyst excision; the PTA probably was successful because the scarring from previous intervention prevented recoil. Percutaneous needle aspiration of cysts wasn't performed because of its high recurrence rate(25). Cystic excision has, compared to arterectomy and revascularization, the disadvantage of a higher recurrence rate, about 10–34%(3,27) due to remaining cystic lesions. Another potential disadvantage is the theoretical possibility of late aneurysmal degeneration of the popliteal artery due to loss of the adventitia; however, some case reports with longer follow- ups don't observe this phenomenon(28,29,30). Still, prolonged, close, clinical and imagiological follow- up is advisable and this patient will maintain surveillance with clinical and DUS evaluations once every year .
CONCLUSIONS
CAD is a rare disease and its natural history and ideal treatment aren't well defined. Furthermore, most of the published data concerning this pathology lacks long-term follow- up. According to this literature review it is our opinion that, in the presence of a patent artery without intimal lesion, the surgical technique of excision of the cysts and adventitia is the treatment of choice because it allows preservation of the intima and offers a less extensive surgical aggression than by pass. Besides, according to our own experience and the reported data, it isn't associated with late aneurismal degeneration. However, further studies with long-term follow- ups are necessary to definitely conclude that this is a safe treatment option.
BIBLIOGRAPHY
Atkins H, Key J. A case of myxomatous tumor arising in the adventitia of the left external iliac artery. Br J Surg. 1947, Vols. 34:165–75. [ Links ]
França M, Pinto J, Machado R, Fernandez G. Bilateral Adventitial Cystic Disease of the Popliteal Artery. Radiology. 2010, Vols. 255:655– 660. [ Links ]
Flanigan DP, Burnham SJ, Goodreau JJ, Bergan JJ. Summary of cases of adventitial cystic disease of the popliteal artery. Ann Surg. 1979, Vols. 189:165–75. [ Links ]
Elias DA, White LM , Rubenstein JD , Christakis M , Merchant N. Clinical evaluation and MR imaging features of popliteal artery entrapment and cystic adventitial disease. AJR Am J Roentgenol. 2003, Vols. 180:627–632. [ Links ]
Maged IM, Turba UC, Housseini AM, Kern JA, Kron IL, Hagspiel KD. High spatial resolution magnetic resonance imaging of cystic adventitial disease of the popliteal artery. J Vasc Surg. 2010, Vols. 51(2):471–4. [ Links ]
Holden A, Merrilees S, Mitchell N, Hill A. Magnetic resonance imaging of popliteal artery pathologies. Eur J Radiol. 2008, Vols. 67(1):159–68. [ Links ]
Correio eletrónico: duarterego@hotmail.com (D. Rego).
Recebido a2017-05-14;
Aceite a 25-10-2017;














