Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.14 no.3 Lisboa set. 2018
CASOS CLÍNICOS
Hybrid management for spontaneous isolated dissection of the common iliac artery: a clinical case
Abordagem híbrida de dissecção espontânea da artéria ilíaca comum: a propósito de um caso clínico
Andreia Coelho1,2, Miguel Lobo1, Clara Nogueira1, Ricardo Gouveia1, Jacinta Campos1,2, Rita Augusto1,2, Nuno Coelho1,2, Ana Carolina Semião1, Alexandra Canedo1,2
1 Angiology and Vascular Surgery Department; Centro Hospitalar Vila Nova de Gaia e Espinho;
2 Faculdade de Medicina da Universidade do Porto
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Iliac artery dissection without aortic involvement is a rare entity, with most cases associated with predisposing factors such as trauma, atherosclerosis, connective tissue disorders or vigorous exercise. The best treatment is not unanimous, and depends on the acuteness and severity of symptoms. Criteria for intervention include prevention of aneurysmatic degeneration, acute limb ischemia, inguinal pain and aneurysm rupture. Recent results using endovascular technique showed comparability with open repair, but there is paucity of data concerning long term results.
Methods: Relevant medical data were collected from hospital database.
Results: The patient is a 65 years old male, referred to the emergency department for abdominal pain in the left lower quadrant with inguinal irradiation. No signs or symptoms of acute limb ischemia were present. He had no previous history of connective tissue disease, cardiovascular risk factors, trauma or vigorous exercise. A CTA was performed, which identified an acute common left iliac artery dissection, with no evidence of vascular compromise of the ipsilateral limb. He was submitted to surgical left femoral approach and percutaneous right femoral approach and dissection exclusion with two stentgrafts. Resolution of abdominal pain occurred immediately. Imagiologic follow-up with CTA was performed 12 and 24 months later with no signs of dissection or residual stenosis.
Conclusion: In this case, an hybrid procedure with femoral surgical approach was performed for access site control. The use of bilateral femoral access was useful to identify the true lumen more accurately and to accommodate a more precise stent placement assuring adequate sealing. At 24 months follow-up, the patient maintains asymptomatic with no evidence of complications in the imagiologic follow-up. No signs or symptoms suggestive of connective tissue disease developed.
Keywords: arterial dissection; common iliac artery; hybrid management
RESUMO
Introdução: A dissecção da artéria ilíaca sem envolvimento da aorta é uma entidade rara, estando a maioria dos casos associados a fatores de risco como traumatismo, aterosclerose, distúrbios do tecido conjuntivo ou exercício vigoroso. A melhor opção terapêutica não é consensual e depende da gravidade e velocidade de evolução dos sintomas. Os critérios de intervenção incluem prevenção de degeneração aneurismática, isquemia aguda de membros, dor inguinal e rotura de aneurisma. Estudos recentes com recurso à técnica endovascular mostraram resultados sobreponiveis com a cirurgia aberta, mas os relativos a resultados a longo prazo são escassos.
Métodos: Observação clínica e consulta de registos clínicos.
Resultados: O doente é um homem de 65 anos, referenciado ao serviço de urgência por dor abdominal no quadrante inferior esquerdo com irradiação inguinal. Sem evidência clínica de isquemia aguda de membro. Não apresentava história prévia de doença do tecido conjuntivo, fatores de risco cardiovascular, trauma ou exercício vigoroso. Foi realizada uma angio-tomografia computadorizada (AngioTC), que identificou uma dissecção da artéria ilíaca esquerda aguda comum, sem evidência de compromisso vascular do membro ipsilateral. Foi então submetido a abordagem cirúrgica femoral esquerda e a abordagem percutânea femoral direita para exclusão da dissecção com recurso a dois stents recobertos. A resolução da dor abdominal ocorreu imediatamente. O follow-up imagiológico com AngioTC foi realizado aos 12 e 24 meses, sem evidência de dissecção ou estenose residual.
Conclusão: Neste caso, um procedimento híbrido com abordagem cirúrgica femoral foi realizado para o controle do local de acesso. O uso do acesso femoral bilateral foi útil para identificar o verdadeiro lúmen com maior precisão e para acomodar uma colocação mais precisa do stent, assegurando uma exclusao adequada do flap de disseção. Aos 24 meses de follow-up, o doente mantém-se assintomático sem evidência de complicações no estudo imagiológico. Estudos comparativos entre tratamento cirúrgico e endovascular demonstraram resultados similares. No entanto, nenhum resultado a longo prazo foi relatado para a colocação de stent endovascular para a disseção da artéria iliaca comum, pelo que são necessários mais estudos para avaliar sua eficácia a longo prazo.
Palavras-chave: disseção arterial; artéria ilíaca comum; abordagem hibrida
Introduction
Injury to the common iliac artery (CIA) is uncommon because of the protection afforded by the bony pelvis and its posterior location in the retroperitoneum.(1) Also, primary spontaneous dissection of arteries is usually described in the aorta and the carotid artery, with iliac artery dissection without aortic involvement being a rare entity, judging by the paucity of cases reported in the literature.(2)
Most cases of isolated iliac artery dissection described are associated with predisposing factors such as trauma, pregnancy, atherosclerosis, connective tissue disorders or vigorous exercise.(3-11) Idiopathic CIA isolated dissection is an exceedingly rare diagnosis.
The natural course of CIA isolated dissection is widely variable. Patients may present with no symptoms, intermittent claudication or acute limb ischemia, iliac wall aneurysmatic degeneration or even pseudoaneurysm progression of the involved segment with subsequent risk of rupture.(12)
The best treatment management is not unanimous, and depends on the acuteness and severity of symptoms. Criteria for intervention include acute limb ischemia, inguinal pain, aneurysm rupture and prevention of aneurysmatic degeneration.(13)
Recent results using endovascular techniques showed comparability with open repair, but there is still paucity of data concerning long term results.(12)
In this case report, we aim to describe the hybrid management of idiopathic isolated dissection of the common iliac artery, with 3 years of follow-up.
Methods
Relevant medical data were collected from hospital database.
Results
The patient is a 65 year-old-male, with no significant medical history, particularly connective tissue diseases, cardiovascular risk factors, history of trauma or vigorous exercise.
He was referred to the emergency department with a sudden abdominal pain located in the left lower quadrant with inguinal irradiation. He had no symptoms referred to the leg, fever, gastrointestinal symptoms or any other complaints. Physical examination revealed slight discomfort with abdominal palpation. Femoral, popliteal and distal pulses were palpable bilaterally.
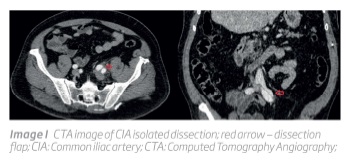
A Computed Tomography Angiography (CTA) was performed, which revealed an acute left CIA dissection, with no evidence of vascular compromise of the ipsilateral limb. Other arterial walls appeared normal, with no evidence of significant atherosclerotic disease. (Image I)
Urgent hybrid management was performed under locoregional anesthesia, with surgical left femoral approach for access site control and correct identification of dissection flap.
Right femoral percutaneous access was used to perform a diagnostic angiography in order to identify the intimal flap and allow safe retrograde guidewire progression.
However, the attempt for ipsilateral retrograde true lumen catheterization with a 0.035-inch hydrophilic guidewire assisted by a 4F catheter and a 6F sheath was unsuccessful. Catheterization of the true lumen was achieved by crossover from right femoral approach with snaring of the contralateral guidewire.
Dissection flap exclusion was attempted with antegrade placement of a stentgraft Endurant II Medtronic Inc, Minneapolis, Minn ETLW161682 with an oversizing of nearly 12%. The stentgraft was deployed proximately from the ostium of the left CIA, with right CIA ostium protection with a guidewire positioned from ipsilateral femoral access . Unfortunately, dissection exclusion with one stengraft was insufficient and a second stentgraft (Endurant II Medtronic Inc, Minneapolis, Minn ETLW161393) deployment was necessary with internal iliac artery exclusion and partial loss of pelvic blood flow. Final angiography from the right femoral access clearly revealed a fully patent lumen and obliterated dissection flap.
Abdominal pain subsided immediately with uneventful recovery. The patient was discharged medicated with dual anti-platelet therapy with clopidogrel (75mg) and low dose acetylsalicylic acid (100mg) for three months and acetylsalicylic acid (100mg) chronically thereafter.
On follow-up, as an outpatient he remained asymptomatic. Clinical evaluation directed for the exclusion of connective tissue disorders revealed no arthralgia, myalgia, Raynaud´s phenomenon or other signs and symptoms suggestive for connective tissue disorders. Haemogram, inflammatory markers and serologic evaluation were unremarkable.
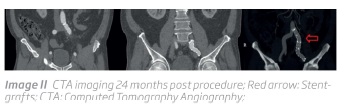
Imagiologic follow-up with CTA was performed at 9 and 24 months revealed no signs of dissection, residual stenosis or stent related complications. (Image II) No further imagiologic control was performed, but the patient was re-evaluated as an outpatient 3 years post-procedure and remained asymptomatic with palpable distal pulses.
Conclusion
Literature review revealed 17 cases of isolated iliac artery dissection reported up to date, most of them related to fibromuscular dysplasia. Only 4 cases were classified as idiopathic.(14-15)
The natural course of spontaneous isolated iliac artery dissection is not well established, because of the rarity of the condition and because of the broad range of presentations. As previously stated, intervention is recommended for prevention of future aneurismal degeneration, lower extremity ischemia, unremitting pain and aneurysm rupture.(15)
Therapeutic options include conservative management, open surgery with prosthetic replacement of the involved area and endovascular approach with covered or uncovered stent placement.(14)
In this case, a hybrid approach was particularly appealing because of its minimal invasiveness and relative technical facility. Self-expandable non-covered stent placement is described in the literature with good results, because the radial force of the stent produces enough compression and local thrombosis of the false lumen, sealing the entry site. Stentgrafts have the potential advantage of assuring sealing of entry and reentry sites.
In this procedure, femoral surgical approach was performed for access site control. The use of bilateral femoral access was useful to identify the true lumen more accurately and to accommodate a more precise stent placement assuring adequate sealing. Hypogastric artery occlusion was necessary, with no complications.
At 24 months follow-up, the patient maintained asymptomatic with no evidence of complications on CTA. Imagiologic control was not repeated thereafter.
As a conclusion, endovascular stent graft placement provides a safe and effective management option for spontaneous common iliac dissection. However, in the literature, no long term results have been reported for endovascular stent placement for CIA dissection, so further studies are necessary to evaluate its long term effectiveness.
REFERENCES
1. SM R, JR W, RT G. Blunt injury of the abdominal aorta: a review. J Trauma. 1997;: p. 42:748-755. [ Links ]
2. ME D, CH M, ES C. Dissection and dissecting aneurysms of the aorta: twenty-year follow-up of five hundred twenty-seven patients treated surgically. Surgery. 1982;: p. 92:1118. [ Links ]
3. Barker S, KG B. Retrograde iliac artery dissection in Marfan´s syndrome. A case report. J Cardiovasc Surg. 1989;: p. 30: 953-954. [ Links ]
4. JE N, Rutherford RB NS. Arterial dissections associated with pregnancy. J Vasc Surg. 1995;: p. 21:515-520. [ Links ]
5. Luck I HDGC. Spontaneous dissection of the external iliac artery due to fibromuscular dysplasia.. Vasa. 2003;: p. 31:115- 121. [ Links ]
6. Honjo O YYKYea. Spontanoeus dissection and rupture of common iliac artery in patient with fibromuscular dysplasia: a case report and review of the literature on iliac artery dissections secondary to fibromuscular dysplasia. J Vasc Surg. 2004;: p. 40:1032-1036. [ Links ]
7. Cattan S MXLFea. Iliac artery dissection in alpha 1-antitrypsin deficiency. Lancet. 1994;: p. 343:1371-1372. [ Links ]
8. Teh LG SKVSGea. Spontaneous common iliac artery dissection after exercise. J Endovasc Ther. 2003;: p. 10: 163-166. [ Links ]
9. Cook PS ELSPea. Dissection of the external iliac artery in highly trained athletes. J Vasc Surg. 1995;: p. 22:173-177. [ Links ]
10. Savolainen H HGFAea. Spontaneous dissection of common iliac artery. A case report.. Vasc Endovasc Surg. 2004;: p. 38:263-265. [ Links ]
11. FernandezAL H. Spontaneous and isolated dissection of the common iliac artery.. J Cardiovasc Surg (Torino). 1997;: p. 38:377-379. [ Links ]
12. Muradi A YMIKea. Hybrid management for spontaneous isolated dissection of the iliofemoral artery. Ann Vasc Surg. 2014;: p. 28: 490.e13-490.e16. [ Links ]
13. Fukui S CEPNea. Bilateral dissection of external iliac artery. Ann Vasc Surg. 2007;: p. 21:373e5. [ Links ]
14. ME D, CH M, ES C. Dissection and dissecting aneurysms of the aorta: twenty-year follow-up of fuve hundred twenty-seven patients treated surgically. Surgery. 1982;: p. 92:1118. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: andreiasmpcoelho@gmail.com (A. Coelho).
Ethical Responsabilities
Protection of patients and animals: The authors state that for this investigation no experiments were performed on humans and / or animals.
Confidentiality of the data: The authors state that they have followed the centre´s established protocols on the publication of patient data.
Right to privacy and informed consent: The authors declare that no patient data is available in this article.
Conflict of interest: The authors declare no potential confict of interest.
Recebido a 18 de junho de 2017
Aceite a 21 de agosto de 2018