Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.15 no.2 Lisboa jun. 2019
ARTIGO ORIGINAL
Above-knee amputation stump ischemia: a surgical challenge in preventing death
Isquemia de coto de amputação transfemoral: um desafio cirúrgico na prevenção da mortalidade
Inês Antunes1, Carlos Pereira1, Gabriela Teixeira1, Carlos Veiga1, Daniel Mendes1, Carlos Veterano1, Henrique Rocha1, João Castro1, Rui Almeida1
1 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar do Porto
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Above-knee stump ischemia is a serious condition. If left untreated usually courses with progression to irreversible ischemia. Without treatment the path from here usually leads to hip disarticulation and death. Our aim is to present our most recent experience in stump revascularization.
Material/Methods: We retrospectively reviewed all patients with above-knee stump ischemia treated in our institution between July 2018 to March 2019.
Results: We present four clinical cases treated in our institution in the last nine months. Two of them presented with non-acute stump ischemia with pain and skin lesions developed after minor trauma several months after surgery and stump healing. In both cases the computed tomography angiography (CTA) showed occlusion of the common femoral artery (CFA) and was inconclusive regarding the status and quality of the deep femoral artery (DFA). Despite this, ischemia severity deemed obligatory an attempt to revascularization, DFA was surgically exposed and proved to be an adequate target run off to a bypass. In the other two, the ischemia of the stump was acute. In one patient it was after surgical treatment of an ipsilateral false aneurism of the CFA (with ligation of the EIA) treated with a bypass from the EIA to both the superficial and DFA. The other was a patient admitted with aortic bifurcation occlusion and irreversible right leg ischemia that was submitted to primary above-knee amputation. In the next postoperative days, the patient developed severe stump ischemia. An axillo femoral bypass and proximal re-amputation was performed. Three patients resolved the stump ischemia and fared well, the last one died in the postoperative period.
Discussion/Conclusions: Above-knee stump ischemia usually leads to progressive stump degradation/necrosis/infection, eventually leading to death. When the common/deep femoral arteries are occluded, re-amputation is usually insufficient and progression of ischemia can dictate the need for a hip disarticulation, a very aggressive and mutilating procedure with high rate of morbidity and mortality that do not prevent progression to pelvic ischemia and death. Revascularization of above-knee amputation stump, based on DFA or hypogastric revascularization, is the best therapeutic alternative and should be attempted even in frail patients. We believe that our small series reinforces the idea that stump revascularization is possible and can save both: stump and life.
Keywords: Stump ischemia, hip disarticulation, deep femoral artery revascularization, above-knee amputation
RESUMO
Introdução: A isquemia de coto de amputação transfemoral (TF) é uma condição clínica grave e que, se não tratada, geralmente cursa com progressão da isquemia o que pode levar à necessidade de desarticulação da anca e à morte. O objetivo deste trabalho é apresentar a nossa mais recente experiência em revascularização de cotos.
Materiais/Métodos: Revisão retrospetiva de todos os doentes com isquemia de cotos TF tratados na nossa instituição entre julho de 2018 e março de 2019.
Resultados: Nos últimos nove meses foram tratadas quatro isquemias de cotos TF. Dois deles apresentaram isquemia não aguda, com dor associada e lesões tróficas após pequeno trauma, vários meses após a cirurgia e cicatrização do coto. Em ambos os doentes, a tomografia computadorizada (TC) revelou oclusão da artéria femoral comum (AFC) e foi inconclusiva relativamente à permeabilidade da artéria femoral profunda (AFP). Face à gravidade da isquemia, foi considerada obrigatória uma tentativa de revascularização tendo-se procedido a uma exploração cirúrgica da AFP. Intra-operatoriamente a AFP revelou ter condições para ser outflow de um bypass. Nos outros dois casos, a isquemia do coto foi aguda. Um caso desenvolveu isquemia após tratamento cirúrgico de um falso aneurisma ipsilateral da AFC (com necessidade de laqueação da AIE) tratado com um bypass da AIE para as AFP e AFS. O segundo caso refere-se a um doente admitido com oclusão da bifurcação aórtica e isquemia irreversível da perna direita tendo sido submetido a amputação TF primária. No pós-operatório evoluiu com isquemia do coto com agravamento progressivo. Foi realizada revascularização com bypass axilo-femoral e re-amputação proximal. Em três casos ocorreu cicatrização do coto e bom outcome, o último doente morreu no pós-operatório.
Discussão/Conclusões: A isquemia de cotos de amputação TF conduz normalmente a agravamento progressivo, necrose, infeção e morte. Quando as AFC/AFP estão ocluídas, a re-amputação geralmente é insuficiente e a progressão da isquemia pode ditar a necessidade de uma desarticulação, procedimento muito agressivo e mutilador com alta taxa de morbi/mortalidade e que não impede a progressão para isquemia pélvica e morte. A revascularização, com base na AFP ou na hipogástrica, é a melhor alternativa terapêutica e deve ser tentada mesmo em doentes frágeis. Acreditamos que a nossa pequena série reforça a ideia de que a revascularização do coto é possível e pode salvar tanto o coto como a vida do doente.
Palavras-chave: Isquemia de coto, desarticulação de anca, revascularização de artéria femoral profunda, amputação acima do joelho
Introduction
Ischemia of above-knee stump is a serious complication that can lead to bacterial infection and eventually sepsis and death. Revision of the amputation stump to a higher level is sometimes successful if there is a patent common/deep femoral artery. When there is an occlusion of this artery, reamputation is usually insufficient with progression of ischemia which normally leads to amputation by an even higher level that can end in hip disarticulation (a very aggressive and mutilating procedure with high rate of morbidity and mortality). Revascularization of above-knee amputation stumps, usually based on deep femoral artery revascularization, is the only therapeutic alternative for these patients to prevent hip disarticulation and death from progression of the ischemia.
The aim of this study is to present our most recent institutional experience of four clinical cases of revascularization of above-knee amputation stumps and to review the available literature.
Clinical Cases
A 72-year old male, history of active smoking, hypertension, dyslipidaemia and peripheral occlusive arterial disease.
After failure of prior revascularization surgery, the patient was submitted to above-knee amputation. In the postoperative period the wound completely healed. At the fifth postoperative month, the patient suffered a trauma of the amputation stump, which did not heal and complicated with infection (Figure 1). The patient was admitted for intravenous antibiotic therapy and wound care, with improvement of local inflammatory signs but without healing. A complementary study with CTA scan revealed occlusion of the common femoral artery and of the initial segment of the deep femoral artery. The patient was proposed to attempt revascularization of the deep femoral artery. Intraoperatively, we found a deep femoral artery permeable (except for the initial segment) and a bypass from de external iliac artery to the deep femoral artery with graft was performed. In the postoperative period there was an improvement of the local pain and the lesions evolved favourably and the patient was discharged on the 8th postoperative day. At follow-up visit after 1 month, occlusion of the bypass was detected but with good evolution of the stump (almost complete healed, with only a minor dry necrosis plaque).
The second case, a 57-year old man with history of diabetes, hypertension, dyslipidemia, poliomyelitis. Due to peripheral occlusive arterial disease the patient was submitted to iliofemoral crossover bypass, which occluded, and the patient was submitted to above-knee amputation that completely healed in the postoperative period. Nine months after surgery the patient developed a small trophic lesion in the stump probably in relation to trauma of the prosthesis. Despite the care of the dressing, the ulcer worsened, and the stump become cold and cyanotic and the patient was guided by the physiatrist for observation by vascular surgery at the 23rd postoperative month. At our observation the stump was cold and cyanotic, with a trophic lesion with about 3cm of greater axis (Figure 2). The CTA revealed occlusion of the crossed iliofemoral bypass, occlusion of the common femoral artery and of the initial segment of the deep femoral artery. The patient was proposed for exploration of the deep femoral artery and attempted revascularization. A thrombectomy of the iliofemoral bypass and a jump graft to the most distal DFA was performed. In the postoperative period, it presented good evolution with improvement of pain, cooling and cyanosis and healing of the trophic lesion.
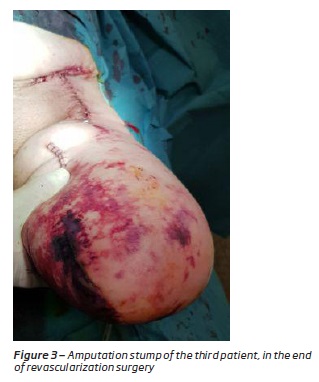
The third case, an 84-year-old woman, with a history of hypertension and atrial fibrillation. Patient admitted with gangrene of toes having undergone transmetatarsal amputation and posteriorly popliteal-peroneal bypass with graft. On the 10th postoperative day, thrombosis of the bypass was detected, the bypass was recovered but re-thrombosed five days later. A new thrombectomy and angioplasty of the peroneal artery was performed, with new thrombosis in the next day. The patient underwent an above knee amputation and removal of the vascular prosthesis (removal in the totality) and the femoral artery was closed with direct suture. At the 24th day after amputation, onset fever, increased inflammatory parameters and pulsatile inguinal swelling. CTA was performed proving the presence of a false aneurism. The patient underwent urgent surgery to exclude the false aneurysm with external iliac artery ligation. In the postoperative period the patient developed progressive severe ischemia of the above-knee stump (with cyanosis up to the thigh root) and for that reason, the patient was submitted to reconstruction of the external iliac artery and femoral bifurcation (with great saphenous vein bypass from the external iliac artery to the superficial and deep femoral arteries) (Figure 3). In the postoperative period, there was a good evolution of the stump, which delimited in an extensive superficial necrosis plaque in the area of previous incision that progressively improved with complete healing documented at the 45th day after revascularization surgery. In a follow-up visit at the 3rd and 6th month thrombosis of the bypass was observed, but the iliac artery was permeable and stump was well perfused, without trophic lesions.
The fourth case, a 74-year-old woman with a history of cerebrovascular disease with cerebral infarction five years before with global aphasia and hemiplegia, hypertrophic cardiomyopathy, atrial fibrillation, and dyslipidemia. The patient was brought to urgent observation for prostration and lower limb pain (severe in the right side). At observation the patient had a right lower limb with irreversible ischemia and had no bilateral femoral pulse. A complementary study with Doppler ultrasound demonstrated occlusion of the aortic bifurcation. The patient underwent transfemoral thrombectomy but failed to get satisfactory inflow. Given the irreversible right-side ischemia (requiring major amputation), the absence of critical ischemia in the left side and the general condition/comorbidities of the patient, it was decided not to proceed to additional revascularization and perform only the above-knee amputation. In the postoperative period, the amputation stump became cyanotic (Figure 4, left image). Initially it was decided to maintain medical treatment namely hypocoagulation and clinical surveillance, but the amputation stump presented poor evolution with worsening of cyanosis and after that signs of pelvic ischemia (Figure 4, right image) and worsening of the analytical parameters of infection. Despite the comorbidities of the patient, since in the absence of revascularization the patient would evolve with ischemia and death, the patient was submitted, 10 days after the above-knee amputation, to an axillofemoral bypass and more proximal re-amputation of the stump. Despite the patient revascularization in postoperative period she evolved to shock that did not reverse and died.
Discussion/Conclusions
Traditionally, lower extremity amputation was viewed as a procedure with an exceptionally high mortality in relation to the magnitude of the procedure(1). In 1984, Blunt et al published a series of 253 consecutive major amputations(2) with operative mortality of 0.9% for below-knee and 2.8% for above-knee amputations. The authors realized that mortality was in large part a result of acute postoperative gangrenous ischemia of the above-knee stump and they defended that in the presence of frank necrosis, attempts to revascularize the ischemic stump was often futile and stump ischemia lead to ascending gangrene, sepsis and death. This has led to an interest in identifying stumps at risk of ischemia before they become ischemic. In 1985 Blunt TJ published 3 criteria to identify patients of high risk to develop this potentially lethal complication and those criteria included thrombosed aortobifemoral bypass, nonvisualisation of the common femoral artery by angiography or a nonpalpable femoral pulse and also an occluded femoral superficial artery in combination with a highly stenotic or occluded deep femoral artery. When the authors did a review of their series, they found 14 patients with these criteria: 5 of them presented acute ischemic stump gangrene and 9 of them were flagged as being at high risk to develop stump ischemia. Concerning the 5 patients with acute stump ischemia, all of them underwent inflow revascularization (2 axillofemoral, 2 profundoplasty and 1 femoro-femoral bypass with profundoplasty) and the overall mortality rate was 60% (2 procedures failed resulting in ascending necrosis and patient death, 1 patient died of pulmonary embolism). From the 9 patients identified at high risk to develop acute stump ischemia, all of them underwent successful prophylactic inflow revascularization without development of stump ischemia with no immediate patient mortality. So, the authors concluded that to avoid this potentially lethal complication and considering that revascularization implies a small additional risk, all patients at high risk to develop stump ischemia should undergo prophylactic revascularization. Similar conclusions were drawn regarding chronic ischemia of amputation stumps. In 1979 Kwaan and Connolly(3) reported a series of chronic ischemic above-knee stump and the authors noted a 100% mortality rate in patients with necrotic or ischemic chronic above-knee amputation stumps without revascularization (7 patients).
The key for the healing of an above-knee amputation stump is the status of the DFA and for this reason this artery is the target of these revascularization procedures. The surgical treatment may consist of(1) profundoplasty (usually associated with femoral endarterectomy) when the disease is limited to the common femoral artery and the initial segment of the deep femoral artery;(2) iliac revascularization (endovascular, surgical);(3) crossed femoro-femoral bypass when revascularization of the iliac axis is not possible or(4) axilofemoral bypass when iliac revascularization is not achieved and contralateral ilio/femoral occlusive disease coexists. The internal iliac artery also plays a very important role in pelvic and thigh perfusion. In fact, in the presence of significant stenotic disease of the internal iliac artery, its treatment may be enough to increase perfusion and enhance stump healing.
In some situations, particularly if there is a patent common/deep femoral artery, revision of the amputation stump with re-amputation to a higher level could be successful. In this situation the ischemia is probably related to poor distal collateral vessels. But in the case of an absent femoral pulse, re-amputation to a higher level was normally useless. Without revascularization, the natural history is the need of successively higher amputations, debridements of necrotic stump, hip disarticulation and eventually death because of continued ascending necrosis and sepsis.
Unfortunately, despite advances in vascular surgery, there is no standard of care of ischemic stump(4) and patients unable to heal an above-knee amputation represent a therapeutic challenge. Historically these patients were often managed with a hip disarticulation with a mortality rate between 40 and 50%(6,7) and with a high dependence on any mobility, and these patients are usually institutionalized(8,9). Nowadays, hip disarticulation represents a last line treatment to be considered only when there is no potential for revascularization and considering the general state and comorbidities of the patient. Hip disarticulation is the amputation of the lower limb through the hip joint. It is a complex, highly mutilating surgery with high mortality rate(10). Endean et al reported a series of 53 patients submitted to hip disarticulation, of which 10 were due to ischemia and 14 due to ischemia and infection. The authors reported 60% rate of operatory wound complications (more in the group of ischemia and infection). The higher mortality (50%) was in patients with ischemia. In fact, the authors found that the presence of ischemia and cardiopathy were the highest predictor of mortality. Dénes et al(11) also reported a series of 63 hip disarticulations (34 for ischemia) and also reported higher surgical wound complications in the ischemic group (64.86% versus 20.83% in the tumour group) and higher mortality rate in the ischemic group (43.4% versus 0%). Also, there are few studies analysing hip disarticulation functional results and they demonstrate a poor quality of life, significant difficulties in the recovery of the gait and difficulties regarding the using of a prosthesis(12,13,14,15). Also, the energy expended to walk in patients with a hip disarticulation increases by 82%, so the patient is often bedridden or confined to a wheelchair(16,17). Age, overall health status, comorbidities and individual motivation are crucial factors for recovery the gait and functional success also depends on the cause of disarticulation and those due to vascular conditions are worse suit to gait again. For these reasons, all efforts are made to avoid hip disarticulation, including some poorly established therapeutic strategies as hyperbaric oxygen therapy. In 2016 Columbo et al published a series of 4 patients with above-knee amputation stump ischemia with nonreconstructable vascular disease facing hip amputation that healed their amputation stumps with hyperbaric oxygen therapy, wound care and negative pressure therapy(18). Hyperbaric therapy consists in an increased oxygen pressure in the inspired gas that lead to an increase of oxygen tension, improves cellular metabolism and inhibits inflammation(19,20) but the efficacy in healing ischemic wounds are heterogenous and benefits remain unclear(21,22,23). The authors suggested that hyperbaric therapy should be considered in ischemic stumps when hip articulation is being considered.
Above knee stump ischemia is a serious condition. The diagnosis of stump ischemia is not always simple. When the stump is cyanotic and cold on palpation, the clinical diagnosis is simpler. However, in some cases, the clinical presentation is more widespread, with the development of trophic lesions and the diagnosis may not be so simple, especially if the patient and clinicians are not alerted to this possibility. As example, in our second clinical case, the patient was 14 months with a trophic lesion until he was referred for observation. We do not find in the literature established criteria for the diagnosis of amputation stump ischemia, so there must be clinical suspicion regarding the findings on physical examination of the patient, namely stump characteristics and the existence or not of a femoral pulse, but even with femoral pulse the stump can develop areas of ischemia. In our opinion, any stump with trophic lesions that do not heal despite adequate dressing care should be referred for vascular assessment.
In our opinion all efforts to revascularize these stumps should be made in the case of acute and in chronic ischemia. Importantly still is not to miss the revascularization timing due to the consequences that follow. In our case, one of the patients with acute ischemia was revascularized at an advanced stage of ischemia and died after revascularization. Amputation stump revascularization was normally based in DFA revascularization but the internal iliac artery is also an important artery in pelvic and thigh perfusion. In our department, we have a case where we opted for this strategy in a patient with a bellow knee amputation stump ischemia and the stump significantly improved perfusion in the post-operative period.
In conclusion, revascularization of above-knee amputation stump, based on DFA or hypogastric revascularization, is the best therapeutic alternative and should be attempted even in frail patients. We believe that our small series reinforces the idea that stump revascularization is possible and can save both: stump and life.
REFERENCES
1. TJ, Blunt. Gangrene of the immediate postoperative above-knee amputation stump: Role of emergency revascularization in preventing death. J Vasc Surg 2. 1985(6):874-877.
2. Blunt TJ, Manship LR, Bynoe RP, Haynes JL. Lower extremity amputation for peripheral vascular disease: A low risk operation. Am Surg 50.1984(11):581-584.
3. Kwaan JHM, Connolly JE. Fatal sequelae of the ischemic amputation stump: A surgical challenge. Arch Surg 138. 1979: 49-52.
4. Affonso BB, Motta-Leal-Filho JM, Cavalcante RN, Falsarella PM, Galastri FL, Cardoso RS, et al. Intra-arterial fibrinolysis for the management of acute ischemia on a below-knee amputation stump. Case report . Einstein (São Paulo) 16. 2018: 1-4.
5. Laszlo G, Kullmann L. Hip disarticulation in peripheral vascular disease. Arch Orthop Trauma Surg, 1987: 126-128. [ Links ]
6. Unruh T, Fisher DF Jr, Unruh TA, Gottschalk F, Fry RE, Clagett GP, et al. Hip disarticulation. An 11 year experience. Arch Surg 125. 1990:791-793.
7. Endean ED, Schwarcz TH, Barker DE, Munfakh NA, Wilson-Neely R, Hyde GL. Hip disarticulation: factors affecting outcome. J Vasc Surg.1991:398-404. [ Links ]
8. Remes L, Isoaho R, Vahlberg T, Viitanen M, Rautava P. Predictors for institutionalization and prosthetic ambulation after major lower extremity amputation during an eight-year follow-up. Aging Clin Exp Res.2009:129-135. [ Links ]
9. Fletcher DD, Andrews KL, Butters MA, Jacobsen SJ, Rowland CM, Hallett JW Jr. Rehabilitation of the geriatric vascular amputee patient: a population-based study. Arch Phys Med Rehabil. 2001:776-779.
10. Moura D, Garruço A. Desarticulação da anca - Análise de uma série e revisão da literatura. Rev Bras Ortop, 2016: 1-5. [ Links ]
11. Dénes Z, Till A. Rehabilitation of patients after hipdisarticulation. Arch Orthop Trauma Surg. 1997:498-499. [ Links ]
12. Fenelon GC, Von Foerster G, Engelbrecht E. Disarticulation ofthe hip as a result of failed arthroplasty. A series of 11 cases. J Bone Joint Surg Br 1980:441-446. [ Links ]
13. Jain R, Grimer RJ, Carter SR, Tillman RM, Abudu AA. Outcome after disarticulation of the hip for sarcomas. Eur J Surg Oncol. 2005:1025-1028. [ Links ]
14. Daigeler A, Lehnhardt M, Khadra A, Hauser J, Steinstraesser L,Langer S, et al. Proximal major limb amputations - a retrospective analysis of 45 oncological cases. World J Surg Oncol. 2009:1-10. [ Links ]
15. Ebrahimzadeh MH, Kachooei AR, Soroush MR, Hasankhani EG, Razi S, Birjandinejad A. Long-term clinical outcomes ofwar-related hip disarticulation and transpelvic amputation. J Bone Joint Surg Am. 2013:1-6. [ Links ]
16. Zalavras CG, Rigopoulos N, Ahlmann E, Patzakis MJ. Hipdisarticulation for severe lower extremity infections. Clin Orthop Relat Res. 2009:1721-1726. [ Links ]
17. Nowroozi F, Salvanelli ML, Gerber LH. Energy expenditure inhip disarticulation and hemipelvectomy amputees. Arch PhysMed Rehabil. 1983:300-303. [ Links ]
18. Columbo JA, Ptak JA, Buckey JC, Walsh DB. Hyperbaric oxygen for patients with above-knee amputations, persistent ischemia, and nonreconstructable vascular disease. J Vasc Surg. 2016:1082-1084. [ Links ]
19. Drenjancevic I, Kibel A. Restoring vascular function with hyperbaric oxygen treatment: recovery mechanisms. J Vasc Res 2014:1-13. [ Links ]
20. Wattel F, Mathieu D, Coget JM, Billard V. Hyperbaric oxygen therapy in chronic vascular wound management. Angiology. 1990:59-65. [ Links ]
21. Stoekenbroek RM, Santema TB, Legemate DA, Ubbink DT, van den Brink A, Koelemay MJ. Hyperbaric oxygen for the treatment of diabetic foot ulcers: a systematic review. Eur J Vasc Endovasc Surg. 2014:647-655. [ Links ]
22. Heyboer M 3rd, Grant WD, Byrne J, Pons P, Morgan M, Iqbal B,et al. Hyperbaric oxygen for the treatment of nonhealing arterial insufficiency ulcers. Wound Repair Regen. 2014:351-355. [ Links ]
23. Margolis DJ, Gupta J, Hoffstad O, Papdopoulos M, Glick HA, Thom SR, et al. Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and the prevention ofamputation: a cohort study. Diabetes Care. 2013:1961-1966. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: ines.antunes89@gmail.com (I. Antunes).
Recebido a 06 de junho de 2019
Aceite a 17 de agosto de 2019