Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.15 no.2 Lisboa jun. 2019
ARTIGO DE REVISÃO
Systemic artery aneurysms in Kawasaki Disease - a Comprehensive Review
Aneurismas arteriais sistémicos na doença de Kawasaki
Nuno Henriques Coelho1, Paulo Barreto1, Victor Martins1, Clara Nogueira1, Jacinta Campos1, Pedro Sousa1, Andreia Coelho1, Rita Augusto1, Carolina Semião1, Evelise Pinto1, João Ribeiro1, Alexandra Canedo1
1 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar Vila Nova de Gaia/Espinho
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Kawasaki Disease (KD) is a self-limited, unknown-cause febrile vasculitis that predominantly addresses medium-sized arteries and most patients are under 5-years-old. In addition to life-threatening coronary artery involvement, aneurysms may develop in almost any medium-sized vessel, however systemic artery aneurysms (SAA) are described in only 2% of cases. The objective of this study was to identify cases of KD associated SAA and to analyze their frequency, anatomical distribution, treatment and outcomes.
Methods: systematic literature review, performed using MEDLINE database.
Results: Literature review retrieved a total of 9 reports corresponding to 38 patients and a total of 134 KD-SAA. The most affected arteries were the brachial artery (29.8%), the internal iliac artery (18,6%), the common iliac artery (16,4%) and the subclavian artery (11,2%) with bilateral involvement being a common feature. History of concomitant coronary involvement was present in almost every patients. Only 5 SAA (3,7%) required intervention. Medical therapy was associated with SAA regression in approximately half of the patients, with better results when initiated promptly after diagnosis. Worst outcomes were found in younger patients, showing higher rates of morbimortality. The underlying coronary sequelae dictated the prognosis.
Conclusions: Considering their rarity, only multicenter collaboration and literature research can provide more insight about KD-SAA treatment and outcomes, defining the potential role of KD as a primary cause of late vascular lesion. Late presentation KD-SAA may present some diagnostic and therapeutic challenges in view of a more likely need for intervention once the benefit of medical treatment has been outweighed.
Keywords: Kawasaki disease, small and medium-sized arteries vasculitis, systemic artery aneurysms, peripheral aneurysms
RESUMO
Introdução: A Doença de Kawasaki (DK) é uma vasculite de pequenos e médios vasos, autolimitada e de causa indeterminada. Frequentemente acomete crianças até aos 5 anos de idade. Para além do atingimento coronário, alterações aneurismáticas podem ocorrer concomitantemente noutros territórios. Contudo, aneurismas sistémicos são descritos em menos de 2% dos casos, sendo por isso escaço o conhecimento que temos acerca da sua distribuição anatómica, evolução e outcome. Realizámos uma revisão sistemática da literatura acerca dos aneurismas arteriais sistémicos associados à DK (AAS-DK).
Métodos: revisão sistemática da literatura, através da base de dados MEDLINE
Resultados: foram selecionados 9 artigos, correspondendo a um total de 38 doentes e 134 AAS-KD. Os segmentos arteriais mais acometidos foram a artéria umeral (29.8%), a artéria ilíaca interna (18,6%) e comum (16,4%) e a artéria subclávia (11,2%). O envolvimento de eixos arteriais de forma simétrica e a história de envolvimento coronário concomitante foi constatado em quase todos os doentes. Apenas 5 dos AAS-DK (3,7%) careceram de intervenção (cirúrgica convencional ou endovascular), 3 dos quais nos casos de apresentação tardia. O tratamento médico isolado associou-se regressão dos aneurismas em quase metade dos casos, sendo mais efetivo quando instituído precocemente. Os doentes mais novos e com formas mais agressivas da doença tiveram maiores taxas de morbimortalidade, sendo o prognóstico ditado pelas sequelas cardíacas.
Conclusões: Tendo em conta a sua raridade, apenas a realização de estudos multicêntricos e revisões da literatura poderão fornecer mais dados que permitam inferior acerca do tratamento e outcome dos AAS-DK. A apresentação tardia de um AAS-DK pode trazer alguns desafios quer em termos diagnósticos, quer em termos terapêuticos tendo em conta uma mais provável necessidade de intervenção, uma vez ultrapassado o timming para o tratamento médico.
Palavras-chave: Doença de Kawasaki, vasculite de pequenos e médios vasos, aneurismas arteriais sistémicos, aneurismas periféricos
Introduction
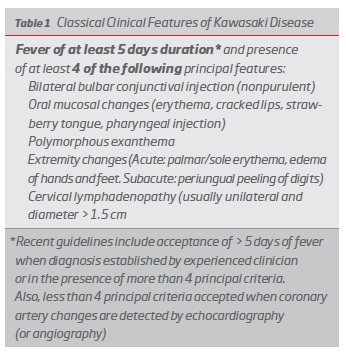
Kawasaki Disease (KD) is an self-limited, unknown-cause febrile vasculitis that predominantly addresses medium-sized arteries.(1) It has an ethnic bias towards Asian children, with Japan having the highest incidence (138/100 000). In USA and UK, the incidence is 17.1/100 000 and 8.1/100 000, respectively. Most patients are under 5-years-old and males are affected 1.5 times more often than girls.(2) It is an exclusion diagnosis, based on clinical “pathognomonic” manifestations (table 1).(1)
Current standard treatment consists of a combination of intravenous immunoglobulin (IVIG), acetylsalicylic acid +/- corticosteroids. This aggressive medical intervention has improved prognosis, in the last decades.(1) When untreated, life-threatening coronary artery ectasias and aneurysms can develop in almost one third of patients.(3,4) Although KD prognosis is mainly dictated by the coronary involvement, systemic artery aneurysms (SAA) can also occur in approximately 2%.(5) SAA can be associated with rupture, embolization or occlusion and may have a delayed presentation, years after KD acute phase.(6) Relatively little literature has been published on the frequency, distribution, treatment and outcomes of KD-SAA. The objective of this study was to identify cases of KD-SAA and to analyze their frequency, anatomical distribution, treatment and outcomes.
Methods
performed using MEDLINE database with the following query: ((Kawasaki disease) OR (Kawasaki syndrome)) AND ((non-coronary arterial aneurysms OR systemic arterial aneurysms OR peripheral arterial aneurysms). All reports that did not provide information about therapeutic approach and outcomes were excluded. Only English language papers were included.
Results
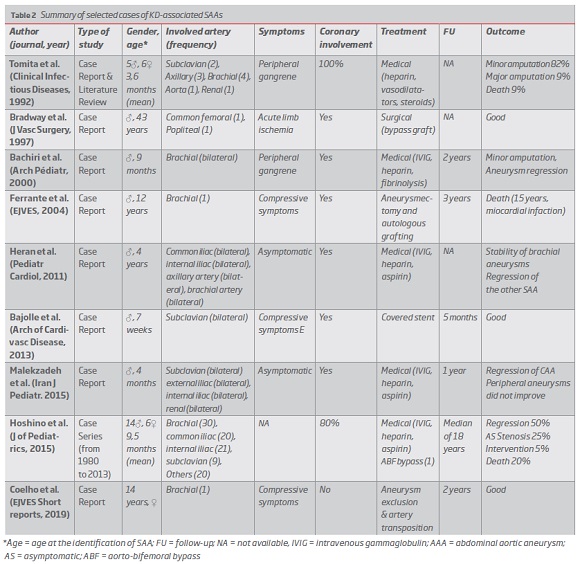
Literature review retrieved a total of 9 reports that meet the eligibly criteria (table 2).(5,6,7,8,9,10,11,12,13) Thirty eight patients (25B and 13@) were identified, corresponding to a total of 134 KD-SAA. Although most SAA were diagnosed in children under 5-years-old, three delayed presentations were found in previously undiagnosed patients.(8,10,13) The most affected arteries were the brachial artery (29.8%), the internal iliac artery (18,6%), the common iliac artery (16,4%) and the subclavian artery (11,2%). Bilateral involvement was a common feature. History of concomitant coronary involvement was present in almost every patients. When identified during KD acute or subacute-phase, medical therapy (IVIG, heparin, antiplatelet and/or fibrinolysis) was the mainstay of SAA treatment. Only 5 SAA (3,7%) required intervention. One during KD acute-phase due to severe compressive symptoms(11), another due to aorto-iliac aneurysm growth during follow-up (aorto-bifemoral bypass at 25 years-old).(6) Intervention was also required in the three delayed presentation cases: one due to acute limb ischemia (n=1)(8) and two cases with upper limb compressive symptoms (n=2).(10,13) Medical therapy was associated with SAA regression in approximately half of the patients, with better results when initiated promptly after KD diagnosis. Worst outcomes were found in younger patients, showing higher rates of morbimortality. The underlying coronary sequelae dictated the prognosis.
Discussion
KD is virtually as enigmatic today as it was when first described by Kawasaki in 1967. Five decades later, no specific inciting etiological agent was yet identified.(4) Independently of the initial insult, KD-acute phase is characterized by an intense inflammatory response, leading to degeneration and weakening of the medium-sized arteries wall.(4,5) Once systemic blood pressure has stressed the weakened vessel sufficiently, an aneurysm can form.(5) Considering that blood pressures are roughly symmetric across the sagittal plane, one can expect to see a degree of symmetry in aneurysm distribution, as well as a predilection for the coronary, subclavian-axillary-brachial axis and for the iliac arteries.
As highlighted by the present results, the existence of SAA increases the likelihood of coronary involvement and SAA outcome is similar to coronary aneurysms.(14) SAA can regress, persist with progressive growth (sometimes requiring intervention) or evolve to a stenotic lesion (found more commonly more than 20 years after KD onset).(15) Despite its proved reduction in coronary aneurysms (from 15-30% to 3 to 5%), studies have not yet documented if there is a concomitant decrease in SAAs with early medical therapy.(5)
As there are no specific KD markers of worst outcome, in the absence of SAA complications adoption of a conservative strategy seems wise.(6,16,17) Enlarging aneurysms or aneurysms causing neurologic or vascular symptoms should be treated surgically. Definitive surgical treatment involves resection of the aneurysm with arterial repair or reconstruction. In infants and small children, microsurgical techniques are required. Results of surgical interventions seem favorable, however patient age and anatomic factors must be considered. Endovascular treatment is not advisable in early ages. However, as reported by Bajolle et al., in the setting of an extreme manifestation - exuberant arm edema and plexus brachial block, in a 7 week-newborn - endovascular aneurysm exclusion may be considered as a bridge to a more definitive intervention.(11)
SAA have been described anecdotally in adult patients with a previous history of KD. However, given the survival benefit obtained with current medical therapy, late-onset SAA could have a higher incidence than previously reported. On the other hand, SAA associated with incomplete/atypical forms of KD (with mild clinical manifestations) can remain undiagnosed until compressive symptoms or limb- threatening events appear.(18) Nevertheless, the relation with a previous KD may be difficult to establish and only the anatomopathological examination can confirm the diagnosis.
Conclusion
It is clear that coronary KD involvement is of paramount importance. Nevertheless, SAA should never be neglected, due to its inherent morbidity (highlighting thromboembolic complications and rupture).
Late presentation KD-SAA may present some diagnostic and therapeutic challenges in view of a more likely need for intervention, once the benefit of medical treatment has been outweighed.
Considering KD rarity, only multicenter collaboration and research can provide more insight about SAA treatment and outcomes, defining the role of KD as a primary cause of late vascular lesion.
REFERENCES
1. Eleftheriou, D. et al. Management of Kawasaki disease. Arch. Dis. Child. 99, 74-83 (2014). [ Links ]
2. Newburger, J. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 110, 2747-2771 (2004). [ Links ]
3. Mason, A. NIH Public Access. 19, 389-399 (2009).
4. Satou, G. M., Giamelli, J. & Gewitz, M. H. Kawasaki disease: Diagnosis, management, and long-term implications. Cardiol. Rev. 15, 163-169 (2007). [ Links ]
5. Heran, M. K. S. & Hockley, A. Multiple mirror-image peripheral arterial aneurysms in Kawasaki disease. Pediatr. Cardiol. 32, 670-673 (2011). [ Links ]
6. Hoshino, S., Tsuda, E. & Yamada, O. Characteristics and fate of systemic artery aneurysm after Kawasaki disease. J. Pediatr. 167, 108-112.e2 (2015). [ Links ]
7. Tomita, S., Chung, K., Mas, M., Gidding, S. & Shulman, S. T. Peripheral Gangrene Associated with Kawasaki Disease. Clin. Infect. Dis. 14, 121-126 (1992). [ Links ]
8. Bradway, M. W. & Drezner, A. D. Popliteal aneurysm presenting as acute thrombosis and ischemia in a middle-aged man with a history of Kawasaki disease. J. Vasc. Surg. 26, 884-887 (1997). [ Links ]
9. Bachiri, A. et al. Ischémie de la main révélant une maladie de Kawasaki. 1307-1310 (2000).
10. Ferrante, A., Manni, R., Pintus, C. & Snider, F. Late presentation of brachial artery aneurysm in a child affected by Kawasaki disease -Case report. EJVES Extra 8, 20-22 (2004). [ Links ]
11. Bajolle, F., Jurzak, P., Cohen, S. & Boudjemline, Y. Endovascular treatment of peripheral aneurysms in Kawasaki disease. Arch. Cardiovasc. Dis. 106, 694-696 (2013). [ Links ]
12. Malekzadeh, I., Ziaee, V., Sadrosadat, T., Moardinejad, M. H. & Sayadpour-Zanjani, K. Kawasaki disease and peripheral gangrene in infancy. Iran. J. Pediatr. 25, 10-13 (2015). [ Links ]
13. Coelho, N. H., Barreto, P., Martins, V., Nogueira, C. & Campos, J. Rare Condition , Unusual Anatomy , Elegant Solution e an Uncommon Manifestation of Kawasaki Disease. EJVES Short Reports 42, 12-14 (2019). [ Links ]
14. Cabrera, N. D., Sridhar, A., Chessa, M., Carminati, M. & Report, C. Giant Coronary and Systemic Aneurysms of Kawasaki Disease in an Infant. 915-916 (2010). DOI: 10.1007/s00246-010-9688-7
15. Takahashi, K., Oharaseki, T. & Naoe, S. Pediatric Cardiology. 138-142 (2001). DOI: 10.1007/s002460010180
16. Ames, E. L., Jones, J. S., Van Dommelen, B. & Posch, J. L. Bilateral hand necrosis in Kawasaki syndrome. J. Hand Surg. Am. 10, 391-395 (1985). [ Links ]
17. Tsuda, E. et al. Incidence of Stenotic Lesions Predicted by Acute Phase Changes in Coronary Arterial Diameter During Kawasaki Disease. Pediatr. Cardiol. 26, 73-79 (2005). [ Links ]
18. von Planta, M., Fasnacht, M., Holm, C., Fanconi, S. & Seger, R. A. Atypical Kawasaki disease with peripheral gangrene and myocardial infarction: Therapeutic implications. Eur. J. Pediatr. 154, 830-834 (1995). [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: nunoc.90@gmail.com (N. Coelho).
Recebido a 01 de julho de 2018
Aceite a 27 de agosto de 2019