Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.15 no.2 Lisboa jun. 2019
ARTIGO DE REVISÃO
Multiple Aneurysmal Disease: a review
Doença Polianeurismática: revisão
Mariana Lemos1, Ivone Silva1,2, Rui Almeida1,2
1 Instituto de Ciências Biomédicas Abel Salazar - Universidade do Porto, Porto, Portugal
2 Serviço de Angiologia e Cirurgia Vascular, Centro Hospitalar Universitário do Porto, Porto, Portugal
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: The degeneration of arterial aneurysms is a common manifestation of atherosclerosis, a process that involves the arterial vasculature, occurring in several arterial territories. With the increase of life expectancy, the number of patients with arterial aneurysms has increased, since its prevalence raises with age. Society of Vascular Surgery classifies arterial aneurysms according to their etiology. The most common form is the degenerative aneurysm, which can result from arterial wall degeneration due to several factors - genetic, inflammatory and/or environmental. Multiple aneurysms are more common in patients with arterial aneurysms of the lower limbs, especially in the popliteal artery. A relationship between abdominal aortic aneurysms and lower extremities aneurysms will be discussed in this review.
Objectives: The purpose of this review is to report what’s new concerning causes, epidemiology and diagnosis of the multiple aneurysmal disease of the abdominal aorta and the lower extremities’ arteries.
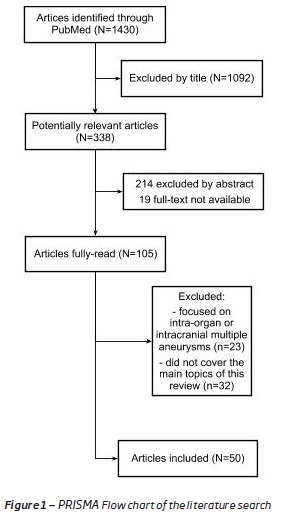
Methods: An initial search was conducted in PubMed that gathered 1430 articles, written in English and Portuguese, within a time period from 1960 to 2019. The articles were, firstly, selected on the basis of title and abstract, excluding criteria were non-English papers and single case reports, articles that focused on intra-oor that did not cover the main topics of this review. A definitive selection of 50 articles was based on full text evolution of the report.
Development: Multiple aneurysmal disease is rare and affects mainly the male sex. Multiple arterial aneurysms manifest as a systemic vascular disease and have been associated with multiple disorders. Atherosclerosis, vasculitis (polyarteritis nodosa and Behçet’s disease), infectious mycotic aneurysms and hereditary conditions, such as Marfan’s syndrome and Ehlers-Danlos are some of the most involved. The incidence of femoral and popliteal aneurysms in persons with abdominal aortic aneurysms appears higher than that noted previously. Ultrasound scanning is appropriate to the recognition of these peripheral aneurysms among patients with abdominal aortic disease. Because the complications can be serious, the early diagnosis assumes great importance for the prevention of complications associated with great morbidity. The role and the challenges associated with genetic tests to determine susceptibility for multiple aneurysmal disease are discussed in this review.
Conclusion: In most cases of multiple aneurysmal disease, symptomatology is vague. Multiple arteries should be surveyed when an aneurysm is suspected or detected at one site, especially in patients with cardiovascular risk factors and in those who present with an isolated aneurysm in the lower extremities.
Keywords: Multiple Aneurysms, Arterial, Etiology, Diagnosis, Treatment
RESUMO
Introdução: Os aneurismas do sistema arterial são uma manifestação frequente de aterosclerose podendo ocorrer em vários territórios arteriais. Com o aumento da esperança média de vida, o número de doentes com aneurismas arteriais tem vindo a crescer, dado a sua prevalência a aumentar com a idade. Existem vários fatores que influenciam na formação de aneurismas arteriais, classificados de acordo com sua etiologia pela Society of Vascular Surgery. A forma mais comum de doença aneurismática é o aneurisma degenerativo, que pode resultar da degeneração da parede arterial consequente a fatores genéticos, inflamatórios e/ou ambientais. Os aneurismas múltiplos são mais frequentes em doentes com aneurismas das artérias dos membros inferiores, especialmente da artéria poplítea. É descrita uma associação entre aneurismas da aorta abdominal e a presença de aneurismas arteriais periféricos do membro inferior, a qual será discutida nesta revisão.
Objetivos: Recentemente novos estudos reportam novas possíveis etiologias para a doença polianeurismática, sendo o objetivo desta revisão bibliográfica descrever o que há de novo no que respeita a causas, epidemiologia, diagnóstico e tratamento da doença polianeurismática da aorta abdominal e das artérias dos membros inferiores.
Métodos: Através da base de dados eletrónica Pubmed-Medline, foram selecionados artigos publicados entre 1960 e 2019, em inglês ou português, com base nos respetivos títulos e resumo. Apenas os artigos contendo informação sobre os principais tópicos abordados nesta revisão foram selecionados, com especial atenção nos mais recentes (de 2001 a 2018).
Desenvolvimento: A doença polianeurismática é rara e afeta mais o sexo masculino. Os aneurismas arteriais múltiplos manifestam-se como uma doença vascular sistémica. Têm sido associados a múltiplos distúrbios incluindo a aterosclerose, as vasculites (poliartrite nodosa e doença de Behçet), aneurismas micóticos infeciosos e a condições hereditárias como os síndromes de Marfan e Ehlers-Danlos. A incidência de aneurismas femorais e poplíteos em doentes com aneurismas da aorta abdominal (AAA) parece maior do que a observada no passado. O eco doppler desempenha um papel importante no diagnóstico de aneurismas periféricos nos doentes com AAA. O diagnóstico precoce é fundamental para a prevenção das complicações geralmente associadas a grande morbilidade. A importância e os desafios no que respeita a testes genéticos para determinar a suscetibilidade para a doença polianeurismática são discutidas nesta revisão.
Conclusão: A doença polianeurismática é rara e na maioria dos casos a sintomatologia é vaga. O diagnóstico precoce e intervenção cirúrgica são necessários para permitir a intervenção adequada e prevenir complicações. Além disso, devem ser estudadas múltiplas artérias quando há suspeita de um aneurisma, especialmente em doentes com fatores de risco e naqueles que apresentam aneurisma isolado nos membros inferiores.
Palavras-chave: Aneurismas Múltiplos, Arterial, Etiologia, Diagnóstico, Tratamento
Introduction
Arterial aneurysms occur throughout the body but are most prevalent in the infrarenal aorta, abdominal aortic aneurysm (AAA), followed by the lower extremity aneurys.(1) As aneurysms are more common in the advanced age, their prevalence has risen due to the increase of life expectancy.(2,3)
Previous studies have reported an association between abdominal aortic aneurysms and peripheral artery aneurysms of the lower limb.(1,4,5) However, there is scarse information concerning multiple aneurysmal disease.(6) It is known that it develops more frequently in men and in elderly patients(2) and has been hypothesized that clinical and pathological characteristics are different in patients with multiple aneurysms in comparison to those with a single aneurysm.(6)
Although causes may be diverse, arterial aneurysms share many of the same risk factors and pose similar threats to life, limb and vital organ function as occlusive arterial disease.(7) Risk factors include age, male sex, history of smoking, family history of aneurysms, cardiac disease, hypertension, presence of other arterial aneurysms and atherosclerotic disease.(1) Diabetes and dyslipidemia seem to have a smaller influence.(6) Aneurysms can also be associated with underlying conditions that predispose to generation of multiple aneurysmal disease as observed in some connective tissue disorders.(1)
Multiple aneurysms are more common in lower extremity, so excluding other arterial aneurysms must be a part of the examination plan in these patients.(2, 8)
Objectives
The main objective of this review the literature is to analyze recent approaches to multiple aneurysmal disease of the abdominal aorta and lower extremities arteries, focusing on its etiology, diagnosis and treatment. It aims to report new findings regarding possible causes, methods of diagnosis and therapeutics, and to raise the awareness for the importance of a multiple artery investigation when diagnosing an arterial aneurysm.
Methods
The review was performed using PubMed database. The search strategy aimed to include research articles and reviews articles which included MeSH keywords: multiple aneurysmal disease, arterial, etiology, treatment and g following PRISMA guidelines (Figure 1). The initial search gathered 1430 articles, written in English and Portuguese, within a time period from 1960 to 2019. The articles were, firstly, selected on the basis of title and abstract. Excluding criteria were non-English papers and single case reports, articles that focused on intra-organ or intracranial multiple aneurysms or that did not cover the main topics of this review. A definitive selection of 50 articles was based on full text evolution of the report. (Figure 1)
Etiology
Multiple aneurysms are common among the elderly population aged above 50 and atherosclerosis is the main etiology for degenerative aneurysms. In young patients, other causes can be responsible for the development of arterial aneurysms. Connective tissue disorders and arteritis have also been associated with peripheral aneurysms.(1, 9)
Due to the many factors that may influence the development of arterial aneurysms, the Society of Vascular Surgery (SVS) classifies them according to their etiology.(10) (Table I)
Arteriomegaly has been described as a nonaneurysmal enlargement of the arteries, associated with tortuosity and markedly slow arterial flow seen on arteriogram.(11) It reflects a systemic alteration of the elastic component of the arterial wall, which results in dilation and elongation of many arteries.(7, 12) It is closely related with multiple and contiguous aneurysms. Yamamoto et al(11) reported that multiple aneurysms were located at the site of arteriomegalic arteries, suggesting that a background of arteriomegaly might depict a subgroup of patients at risk for multianeurysmal disease.(11)
Isolated and multiple aneurysms represent different stages of the presentation of the degenerative deformation that results from elastin digestion in those segments. The concentration of ±-antitrypsin (major inhibitor of elastase) was found to be lower in the aneurysmal wall in patients with multiple aneurysms than in those with isolated ones.(11)
Matrix metalloproteinase (MMP-9) is involved in the remodeling process by degrading extracellular matrix, which is important for the maintenance of structural integrity and favorable mechanical properties of the artery vascular wall. Neutrophil gelatinase-associated lipocalin (NGAL) appears to enhance its activity.(13) MMP-9 may have a role in multiple arterial aneurysms development(14), while NGAL is involved, not only in its regulation, but also in AAA growth. According to de Franciscis et al(13) NGAL levels are higher in AAA patients.(13) Levels of MMP-9 are also significantly increased in patient with artery aneurysms, especially in cases of multiple aneurysms, compared with healthy controls.(14) However, it is still not clear whether the rise in MMP-9 and NGAL levels is a cause or a consequence of aneurysmal generation.(13)
Short relative telomere length (RTL) is related with vascular ageing, inflammation, and cardiovascular risk factors.(15) Previous studies have reported an association between AAA and short RTL in white cells from peripheral blood.(16) A recent study focused on patients with popliteal artery aneurysm (PAA), who often develop multiple aneurysms (including AAAs), hypothesized that if short RTL was associated with the development of aneurysmal disease, it should be shorter in patients with multiple aneurysms compared to those with an isolated aneurysm.(17, 18) The hypothesis was not verified as RTL was not shorter among patients with multiple aneurysms, compared to isolated ones.(17) A possible justification of the contradictory results is that the previously reported shorter RTL in patients with AAA(16) may be a consequence from the high prevalence of cardiovascular risk factors in this patient population, rather than by the aneurysm disease itself.(17)
Degenerative aneurysmal disease
The most common form of aneurysmal disease is the degenerative aneurysm, which is a consequence of the arterial wall degeneration due to several factors - genetic, inflammatory and/or environmental.(11)
The relationship between atherosclerosis and aneurysms is complex. However, aneurysms and atherosclerotic risk factors often coexist in the same patient cohort, with either the aneurysmal or the arterial obstructive disease clinics predominating.(1)
Cigarette smoking intensity is the most significant risk factors for the development of degenerative aneurysms and represents the most attractive target for risk reduction.(1) Diameter progression of aneurysms covers a wide range of variability, that depends on genetic and environmental factors - among which continued smoking and hypertension increases the risk for aneurysm growth.(19)
Enlarged peripheral arteries may be seen in patients with abdominal aortic aneurysm (AAA), and the incidence of AAA is increased in patients with popliteal artery aneurysm (PAA), suggesting a systemic dilation diathesis.(20)
Some specific factors associated with degenerative aneurysms include the presence of abnormal levels of metalloproteinases in the media of aneurysm specimens. Evidence has shown a deficit of antiproteolytic enzymes that inhibit metalloproteinases - specifically the tissue inhibitor of metalloproteinase-1 in these patients.(1) The remodeling of the vascular wall requires proteolytic activity to degrade components of the extracellular matrix, such as elastin and collagen.(7, 21) These can be generated by the matrix metalloproteinase (MMP) system alone or along with the fibrinolytic system. In atherosclerosis, active MMPs may contribute to plaque destabilization and may also promote aneurysm formation by proteolytic degradation of the elastic lamina.(21)
Inflammatory aneurysms
The infrarenal abdominal aorta is the artery most affected by inflammatory aneurysmatic disease.(1) Detailed studies of the cellular infiltrate and cytokine profiles documented in patients with inflammatory aneurysms may eventually lead to a better understanding of this challenging and enigmatic disease state.(1)
Takayasu arteritis is a rare large-vessel vasculitis characterized by stenosis, occlusion, and sometimes aneurysms of the aorta, its major branches and the pulmonary arteries. (22) These are most common in women under 40- years.(23)
Polyarteritis nodosa (PAN) is a primary systemic necrotizing vasculitis predominantly targeting medium-sized arteries such as the main visceral arteries and their branches. It classically presents with fusiform or saccular microaneurysms, often with adjacent stenotic lesions, primarily in the renal, hepatic and mesenteric vasculature.(24)
Kawasaki disease (KD) is one of the most common causes of vasculitis in children. KD can lead to severe cardiovascular complications such as acute vasculitis, coronary aneurysms, and myocarditis.(25) Although KD-related arterial aneurysms affecting the aorta, subclavian, brachiocephalic, axillary, intercostal, celiac, mesenteric, hepatic, renal and iliac arteries have been reported, they are rare.(26) Among patients with KD and systemic aneurysmal disease, the brachial and internal iliac arteries are most commonly affected. Most KD-aneurysms reported were multiple and were detected during the first 8 months of life.(27)
Behçet’s disease is a chronic multisystemic disease affecting the skin, mucous membranes, eyes, joints, central nervous system and blood vessels.(23, 28) Vascular complications described are true and false aneurysms and/or venous thrombosis. Multiple vessels in the same patient can be affected. Arterial manifestations of Behçet disease are uncommon, but are more frequent in the abdominal aorta, followed by aneurysms of the femoral arteries.(23, 28, 29)
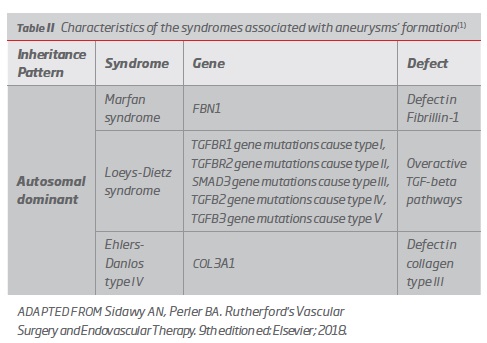
Connective tissue disorders
A connective tissue disorder is a genetic disease in which the primary target is either collagen or elastin protein assembly. Their disruption leads to an inherent predisposition to degeneration, loss of structural integrity, and consequent aneurysm formation. Connective tissue disorders are primary causes of familial aneurysmal disease and require careful genetic characterization and counselling (Table II).
As the technology to completely delineate a single individual’s genetic code becomes a clinical reality, this area of diagnosis and management will probably see significant changes in the near future.
Marfan syndrome is due to an autosomal dominant disease resulting from a defect in the FBN1 gene which leads to abnormal collagen cross-linking.(1, 30) The most common cardiovascular abnormalities include mitral and aortic valvular disease, ascending aortic aneurysm, and aortic dissection. Concomitant aortic dissection and multiple aneurysms have been reported(9) Other aneurysms such as those in the descending thoracic aorta, abdominal aorta, internal carotid artery, and pulmonary artery have been reported in association with Marfan's syndrome but are less common.(31)
Loeys-Dietz syndrome (LDS) is an exceedingly rare autosomal dominant syndrome resulting from a defect in the TGF-² pathway that causes abnormal pathway signaling, tissue friability, craniofacial abnormalities, and a characteristic panvasculopathy.(1) The vascular phenotype is characterized mainly by descending thoracic aortic and peripheral aneurysms, arterial tortuosity, and dissections.(1)
Heterozygous mutations in the genes encoding transforming growth factor ² receptors 1 and 2 (TGFBR1 e TGFBR2 respectively), may present, in less severe cases, similar to Marfan’s syndrome or familial thoracic aortic aneurysm and dissection(32), and in the most severe cases as Loeys-Dietz syndrome.(33) These mutations predict an aggressive and extensive vascular disease.(33)
A differential diagnosis is with vascular Ehlers-Danlos syndrome, caused by similar mutations. In both syndromes, dissection can occur without marked arterial dilation, but in Ehlers-Danlos it is not successfully resolved by surgical intervention, having frequent fatal outcomes(34) in contrast to the Loeys-Dietz syndrome.(33)
Ehlers-Danlos syndrome is a rare inherited disorder of the connective tissue that has been divided into 10 types according to the clinical course and inheritance. In type IV Ehlers-Danlos syndrome there’s an extreme fragility of the arteries is associated with multiple aneurysm formation, spontaneous rupture, and dissection.(1, 35)
Mycotic aneurysms
Mycotic aneurysms account for 1-3% of aneurysms. The majority are aortic although reports have been published about coexistent peripheral aneurysms.(36, 37)
Primary infection of the arterial wall is a rare cause of aneurysms. Mycotic or infectious aneurysms may arise secondarily to infection and are associated with a high morbidity and mortality due to enhanced risk of rupture, sepsis, and subsequent prosthetic graft infection.(7, 36) The exact mechanism for mycotic aneurysm formation is unknown, but some potential mechanisms have been advanced and include direct intimal colonization from hematogenous spread, metastatic implantation through the vasa-vasorum or local vascular extension from an adjacent infectious site.(37-39)
The most frequently organisms responsible for mycotic aneurysms are gram-positive bacteria such as Staphylococcus aureus and Streptococcus species.(37) A wide variety of organisms, including many strains of bacteria and fungi, tuberculosis, and syphilis have also been documented.(1)
Bacillus Calmette-Guerrin (BCG) is a live attenuated strain of Mycobacterium bovis that was initially developed as a vaccination against Mycobacterium tuberculosis infection, and in 1976 was introduced for primary treatment for superficial transition cell carcinoma (TCC) of the urinary bladder.(40) The incidence of BCG-induced mycotic aneurysms following intravesicular infusion is extremely rare. There has been a total of 32 reported cases of mycotic aneurysms as a complication from intravesicular BCG therapy.(40)
Genetic predisposition
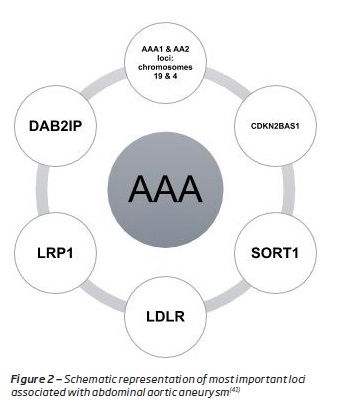
Even though environmental factors are implicated in the development of the pathology, there is a strong genetic diathesis, with family history being one of the strongest risk factors. Several studies suggest that the aneurysmal pathology is multifactorial, and several genetic loci may be implicated. This reflects the need for further investigation of epigenetics, most importantly methylation of DNA and histone modification in patients with aneurysm. Polygenic pathologies are also associated with the gender discrepancy in terms of prevalence, with a male to female ratio of 6:1.(41)
Abdominal aortic aneurysms (AAAs) have a strong genetic predisposition in their etiology, with 20-30% of close male relatives of patients with AAA having an aneurysm, after exclusion of genetic connective tissue disorders.(42)
The inheritance trait seems to be polygenic, but there could be a susceptibility locus for AAA on different chromosomes, which seems to be linked to defective mechanical properties of the abdominal aorta.(43) (Figure 2, Appendix)
The etiology of femoral and popliteal aneurysms probably involves the interaction of a genetic alteration that predisposes to the loss of arterial wall integrity and local forces, such as repeated flexion of the arteries at the hip and knee.(4)
The results of the genetic studies have also indirectly emphasized the importance of environmental factors on the disease process, such as smoking and obesity, that can directly affect DNA methylation processes. Also, controlling hypertension and CV risk factors, such as lipids, is as important as elucidating the genetic background of the pathology.(41)
Epidemiology
The association between iliac, aortic and peripheral aneurysms has been known for decades.(2, 3, 44) In a prospective survey from 1980, patients referred for suspected abdominal aortic aneurysms in the physical examination had a low incidence of associated lower extremities aneurysms, while patients referred for possible femoral or popliteal aneurysms frequently had multiple other peripheral arterial aneurysms.(8)
In the literature, multiple aneurysms are present in 50% to 90% of femoral aneurysms, approximately 30% to 50% of popliteal aneurysms, and as high as 70% for bilateral popliteal aneurysms.(1) Bilateralism is also common, occurring in approximately 25% to 50% of femoral aneurysms and 50% to 70% of popliteal aneurysms.(1, 2, 4)
The involvement of adjacent arterial segments is common in AAAs, with 5% to 15% extending to the juxta- or suprarenal aorta, and 10% to 25% involving the iliac arteries. Synchronous lesions of the thoracic aorta (12%), iliac arteries (10-25%) and femoral or popliteal arteries (14% among male patients) are also common.(1)
Multiple aneurysms also occur in the common iliac artery (CIA) (70%), typically in association with AAA or in bilateral iliac aneurysm (approximately 25%). Isolated aneurysms of the CIA are relatively infrequent (6.4% of patients). Isolated aneurysms of the internal iliac artery (IIAA) are also uncommon, occurring in association with AAAs in less than 2% of cases and are bilateral in 10.9% of cases.(1) A retrospective study showed that 86% of patients who were diagnosed with an IIAA had a corresponding AAA.(45)
Femoral artery aneurysms, though uncommon, they are a potentially limb-threatening disease. They are associated with a high incidence of aneurysmal multiplicity (50-85% with abdominal aortic aneurysms and 25-45% with popliteal aneurysms) and are frequently bilateral (50-70%).(11, 46) Aneurysms of superficial femoral artery (SFA), which are rare, are often associated with concomitant aneurysms (69%), mostly represented by AAAs (40%).(1, 47, 48) Profunda femoralis artery (PFA) aneurysms are extremely rare and, in most cases, are unilateral, although bilateral aneurysms have also been reported.(5)
Popliteal aneurysm is the most frequent peripheral aneurysm (1% of the population). And the one that is most often bilateral.(1) About 50% of patients have bilateral PAAs, and 30% to 50% of patients with PAA may have an associated AAA. On the other hand, less than 15% of all patients with AAAs have coexisting PAAs.(1, 4)
Clinical presentation
Abdominal aneurysms can present with a nonspecific abdominal or lower back pain, with or without hemodynamical instability, as a consequence of rupture, tissue ischemia or from direct pressure applied to the surrounding sensitive structures. It can be detected on physical examination, as a pulsatile mass, most commonly supraumbilical and in the midline.(1, 9, 40) Most AAAs are clinically silent and are discovered incidentally on routine examination. Younger patients are more likely to be symptomatic at the time of diagnosis.(7, 49)
Peripheral aneurysms may be more prone to diagnosis.
Pulsatile mass may call the patients attention or can manifest clinically as acute lower extremity ischemia consequence of thrombosis, distal embolization or local symptoms due to compression of adjacent structures.(18) A patient who has a peripheral aneurysm is likely to have another aneurysm, aortic or peripheral, requiring a careful physical examination.(2)
Associated symptomatic peripheral arterial disease (PAD) in patients with multiple aneurysms is higher than the incidence described in patients with AAA alone(3), but lower than the incidence reported in patients with isolated peripheral aneurysms.(44) The incidence of PAD was highest among patients with a popliteal aneurysm, which enhances the risk for complications.(2)
Most femoral aneurysms are asymptomatic are usually incidentally discovered at routine examination or in the investigation of other aneurysms. Claudication can precede the diagnosis of femoral aneurysm, though this is frequently due to coexisting atherosclerotic occlusion.(46) Other symptoms have been reported such as the presence of a pulsatile mass in the thigh, pain, deep venous thrombosis, lower limb edema, bruising, and claudication.(50, 51) The unusualness of SFA aneurysms has been related to the protection provided by the muscles that surround the artery as well as the lack of bending stress.(47)
Patients with mycotic aneurysms usually present with fever, nephrological symptoms, skin lesions,(23) weight loss, palpable abdominal mass and rarely signs of aneurysm rupture. These findings are unspecific, and the incidence is very low, which makes the diagnosis difficult.(39)
Diagnosis
Aortic aneurysms are an important cause of mortality, still many are diagnosed only incidentally during image methods performed by other reasons or at necropsy.(6) A greater awareness to screen a non-palpable aorto-iliac aneurysm in the presence of a peripheral aneurysm is mandatory, especially if risk factors are present.(2)
Also, when an aortic aneurysm is discovered, the patient should undergo an appropriate examination of the entire aorta and its branches to detect aneurysms in other locations.(7) Moreover, in patients with an AAA, it’s also mandatory to investigate the presence of a peripheral aneurysm.(8) Accordingly, when an aneurysm is suspected after physical examination, the physician should seek to confirm the diagnosis. Additional imaging, such as an ultrasound, may be indicated to evaluate for concomitant aneurysmal disease.(1)
Ultrasound is a first line of investigation for aneurysms.(7, 47) Generally, an AAA is considered to be present when the minimum anteroposterior diameter of the aorta reaches 3.0 cm.(7) Because of technical improvements, their relatively non-invasive nature and lower cost, CT and MR have emerged as the current gold standards in the pre-operative and post-operative evaluation of AAAs.(19) The decision to use either CTA or MRA is often locale-specific.(7, 19)
A popliteal mass should be studied by DUS to distinguish an aneurysm from other soft tissue lesions, such as synovial (Baker’s) cyst.(7) Regardless of the cause, a pulsatile thigh mass should be evaluated by DUS.(7) Early identification of femoral aneurysms may not produce the same clinical benefit, because several studies have shown that small asymptomatic femoral aneurysms may be followed conservatively with few adverse events.(4)
Considering mycotic aneurysms, the gold standard for definitive diagnosis is bacterial cultures within aneurysm tissue after aneurysm repair. However, the culture may be difficult, particularly following antibiotic therapy. The use of molecular diagnostic techniques on aneurysmatic tissue may play an important role in the future.(36) The imaging findings are also nonspecific, demonstrating saccular dilations of arteries not commonly involved by atherosclerosis.(40) Associated findings of perivascular inflammatory change and of atheromatous wall calcifications increases the specificity for mycotic aneurysms.(39)
There is growing interest in determining a potential genetic basis for multiple aneurysms, but linkage studies have been limited by the late onset of aneurysmal disease. Aneurysms of the aorta and peripheral aneurysms affect people mainly after the age of 50, and it is nearly impossible to establish the presence or absence of such a late onset disease in younger family members.(4)
Treatment
The coexistence of more than one aneurysm represents a challenge in the clinical and surgical fields, as after a surgery for aneurysm correction in patients with multiple lesions, the rupture of another one is a frequent cause of death.(6)
Controlling risk factors has been proven to be important in aneurysm development. Patients with aneurysms or a family history of aneurysms should be advised to stop smoking.(7, 52) Strategies targeted at a healthy lifestyle, including exercise and a healthy diet, should be considered.(49)
Life-threatening abdominal aneurysms should be dealt with before limb-threatening peripheral aneurysms, unless impeding rupture or thrombosis of the latter.(2)
Regardless of the etiology, the principles of surgical treatment for the aneurysms are the same. Emergency treatment is indicated in the presence of life-saving or limb-threatening complications such as embolization, thrombosis and rupture.(53)
Until recently, conventional surgery was the golden standard of treatment for all aneurysms. However, endovascular repair has also evolved and proved to be a viable treatment option.(54) Endovascular repair of AAAs provides an alternative to open surgical repair.(7) Endovascular AAA repair (EVAR) can avoid a major transabdominal procedure and can be performed under regional or local anesthesia.(7)
Surgical operation is indicated in all symptomatic and complicated aneurysms. Patients with local findings such as continuous increase in pain, and venous or neural complications, should be treated without delay.(54)
Multiple aneurysmal degeneration represents a more advanced stage of the atherosclerotic process.(2) The surgical principles are the same regardless of the location of the aneurysm: the aneurysms should be excluded and arterial circulation must be restored.(54)
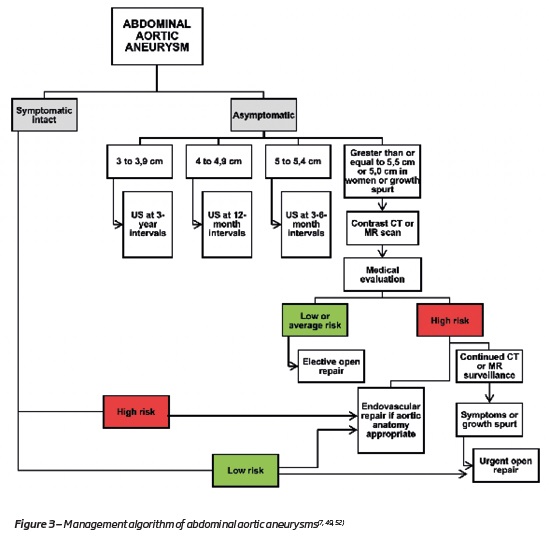
Elective aneurysm repair is recommended in appropriate surgical candidates when an AAA reached a size of at least 5.5cm or becomes symptomatic (if an abdominal or back pain in likely attributed to the aneurysm).(52) In women with acceptable surgical risk elective AAA repair may be considered above 5.0 cm diameter.(49)
For patients with an AAA who are likely to live more than 2 years and who are good risk surgical candidates, open or endovascular intervention is indicated. There is no long-term advantage to either technique of aneurysm repair.(55)
The algorithm overview of the management of AAA is shown in Figure 3, Appendix.
The coexistence of more than one aortic aneurysm represents a challenge in the clinical and surgical points-of-view: after surgery for aneurysm correction in patients with multiple lesions, the rupture of the other aneurysm is a cause of death.(6, 56)
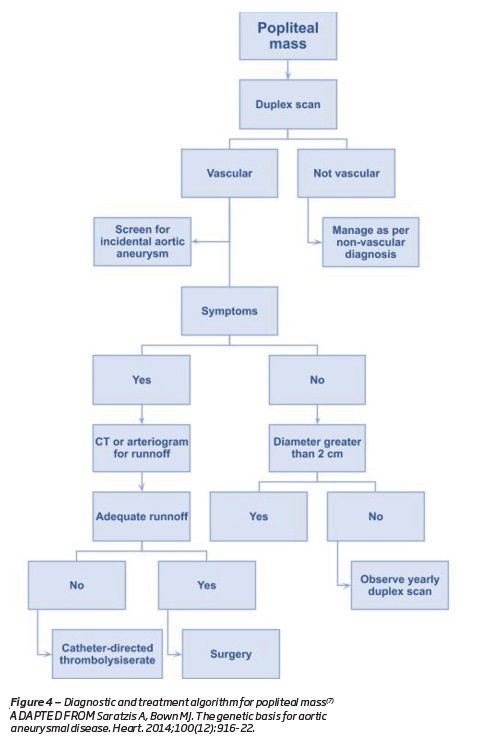
PAA requires surgical treatment if the diameter is greater than 2.0 cm. As stated before, patients with multiple aneurysms are common in patients with bilateral PAAs and survival is decreased compared to the general population.(18) In patients with PAA, the surgical treatment of multiple aneurysms is required to prevent eventual rupture, distal embolization, thrombosis and ultimately amputation.(18) The algorithm (Figure 4, Appendix) summarizes the management options for symptomatic and asymptomatic PAA.
Aneurysms in the femoral arteries require treatment when its diameter exceeds 2,5 cm. (57) Most of the published series recommend elective repair of all symptomatic FAAs if their operative risk is low and if the patient has a reasonable life expectancy.(7, 48)
Treatment of mycotic aneurysms involves urgent surgical repair because of the high risk of rupture. The reconstruction depends principally on the localization and the number of aneurysms.(37)Also, it usually requires intravenous antibiotic therapy combined with staged surgical interventions.(37) The duration of post-operative antibiotic therapy remains contentious due to lack of good data.(36, 58)
Advances in understanding of the molecular pathophysiology of aneurysm formation, growth, and rupture will drive the next round of advances in diagnosis and therapy.(1)
Follow-up
Life expectancy of untreated patients with aneurysm, regardless of etiology and location, is limited with death occurring within 5 years from rupture or associated disease in more than 75% of the cases.(59)
In patients with multiple aneurysms is important to obtain a careful follow-up, since progression of the disease is common and it will allow an early elective surgical intervention prior to acute expansion or rupture.(2)
In childhood aneurysmal disease, life-long follow-up is important because of the cumulative risks of aneurysm recurrence that would require further treatment.(60)
Conclusions
The main message from this review is that multiple arteries should be surveyed when an aneurysm is suspected or detected at one site, especially in patients with cardiovascular risk factors, genetic, inflammatory or collagen diseases and in all who present with an isolated aneurysm in the lower extremities.
Careful clinical and molecular characterization to identify patients and families at risk for multiple aneurysms of genetic cause must be emphasized.
Future work may include simple serological tests (e.g. inflammatory markers or structural proteins of the aortic wall) as markers of growth, identifying patients at risk of complications. More attention needs to be given on epigenetics and gene expression analyses to improve screening and treatment.
BIBLIOGRAPHY
1. Sidawy AN, Perler BA. Rutherford's Vascular Surgery and Endovascular Therapy. 9th edition ed: Elsevier; 2018. [ Links ]
2 .Dent TL, Lindenauer SM, Ernst CB, Fry WJ. Multiple arteriosclerotic arterial aneurysms. Arch Surg. 1972;105(2):338-44. [ Links ]
3. Jackson BB. Surgery of acquired vascular disorders: Thomas; 1969. [ Links ]
4. Diwan A, Sarkar R, Stanley JC, Zelenock GB, Wakefield TW. Incidence of femoral and popliteal artery aneurysms in patients with abdominal aortic aneurysms. J Vasc Surg. 2000;31(5):863-9. [ Links ]
5. Harbuzariu C, Duncan AA, Bower TC, Kalra M, Gloviczki P. Profunda femoris artery aneurysms: association with aneurysmal disease and limb ischemia. J Vasc Surg. 2008;47(1):31-4; discussion 4-5. [ Links ]
6. Gutierrez PS, Leite TN, Mangione FM. Male gender and smoking are related to single, but not to multiple, human aortic aneurysms. Cardiovasc Pathol. 2015;24(5):290-3. [ Links ]
7. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006;113(11):e463-654. [ Links ]
8. Hirsch JH, Thiele BL, Carter SS, Colacurcio C. Aortic and lower extremity arterial aneurysms. J Clin Ultrasound. 1981;9(1):29-31. [ Links ]
9. Naha K, Vivek G, Shetty RK, Dias LS. Multiple idiopathic arterial aneurysms masquerading as aortic dissection. BMJ Case Rep. 2013;2013. [ Links ]
10. Johnston KW, Rutherford RB, Tilson MD, Shah DM, Hollier L, Stanley JC. Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. J Vasc Surg. 1991;13(3):452-8. [ Links ]
11. Yamamoto N, Unno N, Mitsuoka H, Uchiyama T, Saito T, Kaneko H, et al. Clinical relationship between femoral artery aneurysms and arteriomegaly. Surg Today. 2002;32(11):970-3. [ Links ]
12. D'Andrea V, Malinovsky L, Cavallotti C, Benedetti Valentini F, Malinovska V, Bartolo M, et al. Angiomegaly. J Cardiovasc Surg (Torino). 1997;38(5):447-55. [ Links ]
13. de Franciscis S, Mastroroberto P, Gallelli L, Buffone G, Montemurro R, Serra R. Increased plasma levels of metalloproteinase-9 and neutrophil gelatinase-associated lipocalin in a rare case of multiple artery aneurysm. Ann Vasc Surg. 2013;27(8):1185 e5-7. [ Links ]
14. van Laake LW, Vainas T, Dammers R, Kitslaar PJ, Hoeks AP, Schurink GW. Systemic dilation diathesis in patients with abdominal aortic aneurysms: a role for matrix metalloproteinase-9? Eur J Vasc Endovasc Surg. 2005;29(4):371-7. [ Links ]
15. De Meyer T, Rietzschel ER, De Buyzere ML, Langlois MR, De Bacquer D, Segers P, et al. Systemic telomere length and preclinical atherosclerosis: the Asklepios Study. Eur Heart J. 2009;30(24):3074-81. [ Links ]
16. Atturu G, Brouilette S, Samani NJ, London NJ, Sayers RD, Bown MJ. Short leukocyte telomere length is associated with abdominal aortic aneurysm (AAA). Eur J Vasc Endovasc Surg. 2010;39(5):559-64. [ Links ]
17. Bjorck M, Ravn H, Nilsson TK, Wanhainen A, Nilsson PM. Blood cell telomere length among patients with an isolated popliteal artery aneurysm and those with multiple aneurysm disease. Atherosclerosis. 2011;219(2):946-50. [ Links ]
18. Ravn H, Bergqvist D, Bjorck M, Swedish Vascular R. Nationwide study of the outcome of popliteal artery aneurysms treated surgically. Br J Surg. 2007;94(8):970-7. [ Links ]
19. Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(41):2873-926. [ Links ]
20. Lun Y, Jiang H, Jing Y, Xin S, Zhang J. Saphenous vein graft aneurysm formation in a patient with idiopathic multiple aneurysms. J Vasc Surg Cases Innov Tech. 2018;4(3):197-200. [ Links ]
21. Lijnen HR. Metalloproteinases in development and progression of vascular disease. Pathophysiol Haemost Thromb. 2003;33(5-6):275-81. [ Links ]
22. Keser G, Aksu K, Direskeneli H. Takayasu arteritis: an update. Turk J Med Sci. 2018;48(4):681-97. [ Links ]
23. Mei F, Yu M, Li Y, Jin B, Ouyang C. Treatment of multiple aneurysms. Ann Vasc Surg. 2014;28(8):1937 e13-7. [ Links ]
24. Hernandez-Rodriguez J, Alba MA, Prieto-Gonzalez S, Cid MC. Diagnosis and classification of polyarteritis nodosa. J Autoimmun. 2014;48-49:84-9. [ Links ]
25. Ekici F, Varan B, Kocabas A, Erdogan I, Eminoglu S, Aktas D. Multiple giant aneurysms and stenoses of the coronary and systemic arteries in an infant with kawasaki disease at the early stage of convalescent period. Echocardiography. 2014;31(5):E147-50. [ Links ]
26. Roy S, Biswas MK. Multiple Systemic Aneurysms in a Case of Neglected Kawasaki Disease. J Paediatr Child Health. 2019;55(1):117. [ Links ]
27. Hoshino S, Tsuda E, Yamada O. Characteristics and Fate of Systemic Artery Aneurysm after Kawasaki Disease. J Pediatr. 2015;167(1):108-12 e1-2. [ Links ]
28. Bartlett ST, McCarthy WJ, 3rd, Palmer AS, Flinn WR, Bergan JJ, Yao JS. Multiple aneurysms in Behcet's disease. Arch Surg. 1988;123(8):1004-8.
29. Ali O, Nicholl P, Carruthers D, Geoghegan J, Tiwari A. Multiple Aneurysms and a Transplanted Kidney in Behcet Disease. Vasc Endovascular Surg. 2017;51(2):108-10. [ Links ]
30. Sonesson B, Hansen F, Lanne T. Abnormal mechanical properties of the aorta in Marfan's syndrome. Eur J Vasc Surg. 1994;8(5):595-601. [ Links ]
31. de Virgilio C, Cherry KJ, Jr., Schaff HV. Multiple aneurysms and aortic dissection: an unusual manifestation of Marfan's syndrome. Ann Vasc Surg. 1994;8(4):383-6.
32. Pannu H, Fadulu VT, Chang J, Lafont A, Hasham SN, Sparks E, et al. Mutations in transforming growth factor-beta receptor type II cause familial thoracic aortic aneurysms and dissections. Circulation. 2005;112(4):513-20. [ Links ]
33. Loeys BL, Schwarze U, Holm T, Callewaert BL, Thomas GH, Pannu H, et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med. 2006;355(8):788-98. [ Links ]
34. Oderich GS, Panneton JM, Bower TC, Lindor NM, Cherry KJ, Noel AA, et al. The spectrum, management and clinical outcome of Ehlers-Danlos syndrome type IV: a 30-year experience. J Vasc Surg. 2005;42(1):98-106. [ Links ]
35. Oka N, Aomi S, Tomioka H, Endo M, Koyanagi H. Surgical treatment of multiple aneurysms in a patient with Ehlers-Danlos syndrome. J Thorac Cardiovasc Surg. 2001;121(6):1210-1. [ Links ]
36. Dickinson KJ, Parry DJ, Sandoe JA, Gough MJ. Multiple peripheral pneumococcal mycotic aneurysms without aortic involvement: a unique case confirmed with the novel use of a molecular diagnostic technique. J Vasc Surg. 2007;45(6):1253-5. [ Links ]
37. Coutu M, Blair JF. Multiple mycotic aortic aneurysms due to Streptococcus pneumoniae. Ann Vasc Surg. 2003;17(5):554-7. [ Links ]
38. Harding GE, Lawlor DK. Ruptured mycotic abdominal aortic aneurysm secondary to Mycobacterium bovis after intravesical treatment with bacillus Calmette-Guerin. J Vasc Surg. 2007;46(1):131-4. [ Links ]
39. Coscas R, Arlet JB, Belhomme D, Fabiani JN, Pouchot J. Multiple mycotic aneurysms due to Mycobacterium bovis after intravesical bacillus Calmette-Guerin therapy. J Vasc Surg. 2009;50(5):1185-90. [ Links ]
40. Duvnjak P, Laguna M. Left Anterior Descending Coronary Artery and Multiple Peripheral Mycotic Aneurysms Due to Mycobacterium Bovis Following Intravesical Bacillus Calmette-Guerin Therapy: A Case Report. J Radiol Case Rep. 2016;10(8):12-27. [ Links ]
41. Saratzis A, Bown MJ. The genetic basis for aortic aneurysmal disease. Heart. 2014;100(12):916-22. [ Links ]
42. Bjorck M, Wanhainen A. Pathophysiology of AAA: heredity vs environment. Prog Cardiovasc Dis. 2013;56(1):2-6. [ Links ]
43. De Basso R, Sandgren T, Ahlgren AR, Lanne T. Increased cardiovascular risk without generalized arterial dilating diathesis in persons who do not have abdominal aortic aneurysm but who are first-degree relatives of abdominal aortic aneurysm patients. Clin Exp Pharmacol Physiol. 2015;42(6):576-81. [ Links ]
44. Crawford ES, Edwards WH, Debakey ME, Cooley DA, Morris GC, Jr. Peripheral arteriosclerotic aneurysm. J Am Geriatr Soc. 1961;9:1-15.
45. Huang Y, Gloviczki P, Duncan AA, Kalra M, Hoskin TL, Oderich GS, et al. Common iliac artery aneurysm: expansion rate and results of open surgical and endovascular repair. J Vasc Surg. 2008;47(6):1203-10; discussion 10-1. [ Links ]
46. Lancashire MJ, Galland RB. Aneurysm of lateral circumflex femoral artery in association with multiple atherosclerotic aneurysms. Ann Vasc Surg. 1992;6(3):289-91. [ Links ]
47. Belhaj A, Chimanuka D, Rondelet B. Giant true aneurysm of superficial femoral artery in patient with multiple atherosclerotic aneurysms: A case report. Int J Surg Case Rep. 2017;35:94-7. [ Links ]
48. Leon LR, Jr., Taylor Z, Psalms SB, Mills JL, Sr. Degenerative aneurysms of the superficial femoral artery. Eur J Vasc Endovasc Surg. 2008;35(3):332-40.
49. Wanhainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T, et al. Editor's Choice - European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc Endovasc Surg. 2019;57(1):8-93. [ Links ]
50. Papadoulas S, Skroubis G, Marangos MN, Kakkos SK, Tsolakis JA. Ruptured aneurysms of superficial femoral artery. Eur J Vasc Endovasc Surg. 2000;19(4):430-2. [ Links ]
51. Honjo O, Yamada Y, Mima T, Kushida Y. Surgical treatment for an atherosclerotic aneurysm of the superficial femoral artery: report of a case. Surg Today. 2004;34(2):188-9. [ Links ]
52. Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67(1):2-77 e2. [ Links ]
53. Hama Y, Kaji T, Iwasaki Y, Kawauchi T, Yamamoto M, Kusano S. Endovascular management of multiple arterial aneurysms in Behcet's disease. Br J Radiol. 2004;77(919):615-9. [ Links ]
54. Goncu T, Sezen M, Vural H, Eris C, Yavuz S, Ozyazicioglu A. Sequential development of multiple atherosclerotic peripheral arterial aneurysms in a four-year period. Arch Med Sci. 2009;5(2):273-6. [ Links ]
55. Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, et al. 2011 ACCF/AHA focused update of the guideline for the management of patients with peripheral artery disease (updating the 2005 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society for Vascular Medicine, and Society for Vascular Surgery. Catheter Cardiovasc Interv. 2012;79(4):501-31. [ Links ]
56. Crawford ES, Cohen ES. Aortic aneurysm: a multifocal disease. Presidential address. Arch Surg. 1982;117(11):1393-400. [ Links ]
57. Mees B, Robinson D, Verhagen H, Chuen J. Non-aortic aneurysms - natural history and recommendations for referral and treatment. Aust Fam Physician. 2013;42(6):370-4. [ Links ]
58. Salzler GG, Long B, Avgerinos ED, Chaer RA, Leers S, Hager E, et al. Contemporary Results of Surgical Management of Peripheral Mycotic Aneurysms. Ann Vasc Surg. 2018;53:86-91. [ Links ]
59. Crawford ES, Coselli JS, Svensson LG, Safi HJ, Hess KR. Diffuse aneurysmal disease (chronic aortic dissection, Marfan, and mega aorta syndromes) and multiple aneurysm. Treatment by subtotal and total aortic replacement emphasizing the elephant trunk operation. Ann Surg. 1990;211(5):521-37. [ Links ]
60. Davis FM, Eliason JL, Ganesh SK, Blatt NB, Stanley JC, Coleman DM. Pediatric nonaortic arterial aneurysms. J Vasc Surg. 2016;63(2):466-76 e1. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: heitor.ivone@gmail.com (I. Silva).
Recebido a 06 de junho de 2019
Aceite a 08 de agosto de 2019