Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Angiologia e Cirurgia Vascular
versão impressa ISSN 1646-706X
Angiol Cir Vasc vol.16 no.3 Lisboa set. 2020
ORIGINAL ARTICLE
Open heart surgery or carotid endarterectomy. Which procedure should be done first?
Endarterectomia carotídea ou cirurgia cardíaca. Que procedimento deverá ser realizado primeiro?
Pedro Pinto Sousa1, Gabriela Teixeira2, Pedro Sá Pinto2, Luís Vouga3, Rui Almeida2
1Centro Hospitalar Alto Ave
2Centro Hospitalar Universitário do Porto
3Centro Hospitalar Vila Nova de Gaia/Espinho
Endereço para correspondência | Dirección para correspondencia | Correspondence
ABSTRACT
Introduction: Ischemic stroke is a predictable complication of cardiac surgery specially in patients with previous diagnosed carotid stenosis. On the other side, patients undergoing carotid endarterectomy with concomitant significant valvular or coronary artery disease, may face worst peri-operative outcomes.
Objective: Analyzing outcomes from a pool of patients with both comorbidities wondering which procedure should be conducted first.
Material and Methods: Retrospective analysis of a group of patients submitted to carotid endarterectomy (Group I) between January 2011 and December 2017 that concomitantly presented coronary artery or valvular disease. Outcomes comparison with a group of patients submitted to cardiac surgery (Group II) that concomitantly presented carotid stenosis.
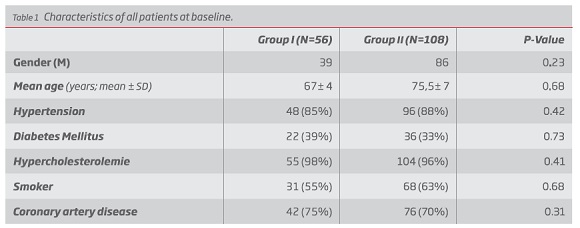
Results: There was no statistically significant difference in patient stroke risk-factors between groups.
Adverse events rate difference between groups did not reach statistical significance (stroke 1,7% vs 2,8% p=0,698; Acute myocardial infarct 1,7% vs 2,8% p=0,698, death 0% vs 4,6% p=0,073).
Discussion: Handling these specific pools of patients is still debatable. Both interventions demand a multidisciplinary approach so as an experienced surgery and anaesthesiology team to individually select which approach fits each patient better.
Keywords: Carotid endarterectomy; Open heart surgery; Carotid stenosis; Stroke; Combined surgery; Coronary event; transient ischemic attack
RESUMO
Introdução: O acidente vascular cerebral isquémico é um potencial evento adverso pós cirurgia cardíaca, principalmente em doentes que apresentem estenose carotídea. Contudo, também os eventos cardíacos são complicações peri-operatórias conhecidas aquando da realização de endarteriectomia carotídea e será tão mais frequente quando na presença de doentes com doença coronária ou valvular.
Objetivo: Analisar os resultados operatórios de um grupo específico de doentes que apresentasse concomitantemente ambas as patologias e tentar inferir sobre que procedimento deveria ser realizado primariamente.
Materiais e métodos: Análise retrospetiva de doentes submetidos a endarteriectomia carotídea (Grupo I) entre Janeiro de 2011 e Dezembro de 2016 com estenose carotídea assintomática mas que apresentassem doença coronária ou valvular concomitante. Comparação com um segundo grupo de doentes submetido a cirurgia cardíaca, entre Janeiro de 2015 e Dezembro de 2017 (Grupo II) e que apresentassem concomitantemente estenose carotídea.
Resultados: Não houve diferença estatística em termos de fatores de risco cardiovasculares entre os grupos analisados.
A taxa de eventos adversos registada não foi estatisticamente significativa (AVC 1,7% vs 2,8% p=0,698; Enfarte agudo do miocárdio 1,7% vs 2,8% p=0,698, Mortalidade 0% vs 4,6% p=0,073) entre os dois grupos.
Discussão: A melhor orientação deste grupo específico de doentes permanece questionável. A sua análise e decisão terapêutica deverá envolver uma experiente equipe cirúrgica e de anestesiologia para decisão individual de como proceder caso a caso.
Palavras-chave: Endarterectomia carotídea; Cirurgia cardíaca; estenose carotídea; Acidente vascular cerebral; Cirurgia combinada; Evento coronário; Acidente isquémico transitório
Introduction
Ischemic stroke, associated to a perioperative thromboembolic or hypoperfusion event is a well-recognized complication of cardiac surgery specially in patients with previous diagnosed carotid stenosis.
Regarding this subject, recent studies have analysed peri operative stroke during post-cardiac surgery with published rates of 1%-5%(1-3), with valvular surgery ringing the highest risk.
The literature debates how concomitant cerebrovascular atherosclerotic disease may increase the stroke risk for cardiac surgery patients, publishing that asymptomatic patients with 50-99% stenosis have a 3.8% stroke risk and patients with bilateral asymptomatic stenosis have a 6.5%, with ipsilateral stroke occurring in 2.0%(4).
Nevertheless, patients with need of open-heart surgery fulfil the criteria adopted in SAPPHIRE(5,6) that outline them as being high-risk for carotid endarterectomy (CEA).
Already established is that the most symptomatic atherosclerotic vascular bed should be treated first, but prospective trials are required when it concerns to asymptomatic disease. Current guidelines advocate multidisciplinary assessment of patients with significant carotid disease before cardiac surgery (Class I, Level C), carotid duplex screening for high risk patients (Class IIa, Level C) and, determines that in asymptomatic patients with bilateral high-grade stenosis, or with unilateral high-grade stenosis and contralateral occlusion, carotid revascularization ‘may be considered’ (Class IIa, Level C)(7).
Objective
The aim of the study was to retrospectively analyse and then compare the peri-operative results from two different surgical orientations of patients with both cardiac and carotid disease in tertiary centres.
Material and Methods
We retrospectively analysed the data from two different institutional patients, both from tertiary centers.
One group, thereafter named Group I, was submitted to carotid endarterectomy, between January 2011 and December 2016 due to severe (70-99%), asymptomatic carotid artery stenosis.
The specificity of this group was that they, concomitantly presented severe coronary artery (CAD), valvular disease or both with indication for open heart surgery. Severe coronary artery disease was defined as 2 or 3 vessel CAD or left main coronary artery disease.
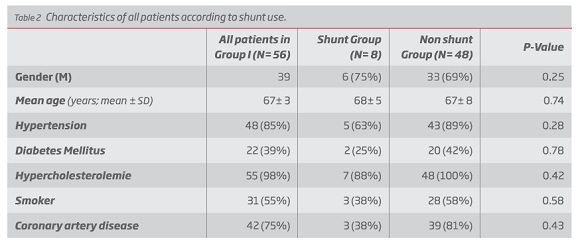
The Group I was subsequently divided into three groups: Ia with unilateral stenosis; Ib with bilateral stenosis and Ic with contralateral occlusion.
General or locoregional anaesthesia were both accepted for analyses. Nevertheless, despite the choice of anaesthesia was left to the surgical team’s discretion, every procedure registered in this study were under general anaesthesia.
The operative technique was traditional endarterectomy with routine patching.
Shunting was selective according to cerebral perfusion monitoring (<50mmHg on stump pressure or rSO2 > 20% on near-infrared spectroscopy).
Symptomatic carotid disease and patients submitted to CEA with eversion technique were excluded.
In the second group, Group II, we analysed the data from a pool of patients, between January 2015 and December 2017 that were submitted to non-urgent CABG or valve replacement.
The specificity of this group was that they, concomitantly presented, at least, unilaterally, severe carotid artery stenosis. Exclusion criteria were patients undergoing urgent cardiac surgical procedures performed within 24 hours of admission and those with symptomatic carotid artery stenosis.
Only patients submitted to cardiac surgery under off pump technique were accepted.
Primary outcomes of the study were development of adverse events in the peri-operative period (30 - day) such as transitory ischemic attack (TIA)/stroke, acute myocardial infarct or death. Perioperative stroke was defined as persistent neurologic deficit (>24 hours) that was due to cerebral ischemia occurring at a time between the surgical procedure until hospital discharge.
Patients submitted to carotid stenting previously or in combination with OHS and patients submitted to combined carotid endarterectomy and cardiac surgery were excluded. Re-stenosis were also an exclusion criterion.
Analysis of arch calcification was performed retrospectively reviewing computed tomography (CT) angiograms and when not available scrutinising r-ray evidence of calcification. Despite some authors describing electron beam computer tomography and multi-detector row CT as the gold standard for evaluating aortic arch calcification, with power to quantify its severity and disease progression(7), these exams are not routinely available.
The statistical analyses were accomplished with IBM SPSS Statistics Base 22.0®. Characteristics comparison between group 1 and group 2 was performed with Student’s t-test test. Eventually with Chi-square test or Fischer exact test for the other categorical variables. A probability value of < 0.05 was considered statistically significant.
Descriptive statistics is presented using relative and absolute frequencies for categoric variables. Continuous variables are described as mean ± SD.
Results
In Group I, we encompassed 56 patients, 39 males, with a mean age of 67 (min 63, max 81) years old.
Of those, 42 (75%) had concomitantly significant coronary artery disease, 11 (20%) had valve disease with indication for valve replacement and 3 (5%) had both pathologies presented.
Every patient had, at least, a unilateral carotid artery stenosis greater than 70%. According to the contralateral carotid artery, 5 (9%) had contralateral internal carotid artery occlusion, 12 (21%) had contralateral severe (70-99%) carotid artery stenosis and the left side was always the chosen for the first intervention, 21 (38%) had a contralateral stenosis between 50-69% and the other 18 (32%) had no hemodynamic significantly carotid stenosis.
All patients were submitted to carotid endarterectomy and Dacron® Patch angioplasty under general anaesthesia. In the peri-operative period, 1 patient (1,7%) developed a non-disabling stroke, 1 (1,7%) a cardiac event that required transfer to a Cardiac Unit, but no mortality was registered.
The patient that developed non-disabling stroke was a male patient with contralateral carotid occlusion and a predominantly hypoechoic atherosclerotic plaque with signs of ulceration. The one that developed a cardiac event after the procedure was a male patient with coronary three-vessel disease and also a predominantly hypoechoic atherosclerotic plaque with signs of ulceration.
In Group II, we encompassed 108 patients, 86 males, with a medium age of 75,5 (min 45, max 84) years. 56 (51%) patients were submitted to bypass grafting, 32 (30%) to valve replacement and 20 (19%) to both.
Every patient had, at least, one side with severe (70-99%) carotid stenosis, 46 (43%) had contralateral moderate (50-69%) carotid stenosis, 27 (25%) had a severe contralateral carotid stenosis; 20 (19%) had contralateral occlusion.
As medical records, 5 (5%) patients had a previous history of neurologic event (TIA or non-disabling stroke). In the peri-operative period, 3 patients (2,8%) developed transient ischemic attack (TIA) or stroke, 3 (2,8%) a cardiac event and 6 (5,6%) patients died (3 due to a cardiac event and 2 due to a neurologic event). Two (67%) of the neurologic events occurred in the corresponding side of a severe hemodynamic carotid stenosis although both these patients had also significant aortic arch calcification and atrial fibrillation. None of the patients that developed post-operative TIA or stroke had previously a neurologic event, but had a significant contralateral carotid artery stenosis.
When proceeding with comparison, adverse events rate difference between groups did not reach statistical significance (stroke 1,7% vs 2,8% p=0,70; AMI 1,7% vs 2,8% p=0,70, mortality 0% vs 5,6% p=0,07).
There was no statistically significant difference in patient stroke risk-factors between groups.
Discussion
The optimal management of patients with concomitant severe carotid stenosis and significant coronary artery or valve disease remains controversial.
Bucerius et al(8) reported that CABG was associated with a 3.8% stroke risk, and CABG + valve surgery had a 7.4% stroke risk, though comparable to the ones we attended (overall 2,8%).
The 1.7% stroke rate that we attended for Group I is still below the accepted 3% described in the literature for asymptomatic carotid stenosis endarterectomy. No RCT has yet evaluated whether CEA under locoregional anaesthesia is equivalent to (or safer) than CAS in symptomatic patients with severe cardiac or pulmonary disease.(4)
When analyzing data in comparison between groups, cardiac surgery prior to carotid endarterectomy might be associated with higher adverse events rate even tough, the events rate reached is not prohibit, therefore very reasonable.
There is still limited evidence to guaranty the benefit of prophylactic carotid revascularization prior to OHS and the results attested that this last group of patients, may safely undergo OHS prior to carotid endarterectomy(4).
Aortic sclerosis is a known risk factor for peri-operative stroke, as cross clamping the aorta may lead to unpredictable atheroemboli which may have also contributed to the overall stroke rate in this cohort submitted to OHS, despite de bias with aortic arch calcification analyses.
We concomitantly analysed some other risk factors for stroke during CABG like aortic atherosclerosis, previous stroke or transient ischemic attack, age, hypertension, diabetes, smoking and peripheral arterial disease. None reached a significant statistical difference between groups nor even when analysed between those patients that faced an adverse outcome. Although there are still others, not here analysed like left ventricular dysfunction, left main coronary artery disease and increase cardiopulmonary bypass time that require further studying. According to the literature, during cardiac surgery, on-pump procedures with hypothermic circulatory arrest carried the highest early stroke risk, still this was not subject of analyse here(9-12).
Intracranial cerebral atherosclerosis should also play a role in this chapter and is still understudied with a study suggesting that intracranial atherosclerosis independently increases post-CABG stroke risk(13).
Castaldo et al described OHS in 230 patients with severe (>80%) carotid stenosis with an ischemic stroke rate of 0.9% which may led us to believe that once done in a very skilled and experience cardiac surgery department, those patients may safely undergone OHS before CAE(9).
Carotid artery stenting (CAS) might be an alternative to CEA. In an updated meta-analysis, the overall 30day death/stroke rate was 7.9% for patients who underwent staged or same day CAS-CABG, but when considered only asymptomatic patients the rate descended to 6.7%(15). Shishehbor also published that outcomes significantly favored staged CAS-CABG after the first year(16).
European society of vascular surgery guidelines suggest that when presented with bilateral severe carotid stenosis or significant carotid stenosis and occlusion on the contralateral side, since the outcomes achieved are acceptable, these group of patients may be better oriented staged or synchronous carotid intervention with coronary artery bypass(4).
Both interventions require a multidisciplinary approach and a very experienced and skilled team to decide which approach fits each patient better. The bias from this study are that it is retrospective, with a short period of follow up and reduced pool of patients analysed.
Nevertheless, the authors believe that if we have an experienced vascular and cardio-thoracic surgical team with attested CEA and OHS outcomes, CEA procedure might still be safe in cardiac surgery patients so as OHS with concomitant carotid artery stenosis and even beneficial when we have to consider the learning curve to achieve attested results for CAS-CABG.
REFERENCES
1. Newman MF, Ferguson TB, White JA, Ambrosio G, Koglin J, Nussmeier NA, et al. Effect of adenosine-regulating agent acadesine on morbidity and mortality associated with coronary artery bypass grafting: the RED-CABG randomized controlled trial. JAMA : the journal of the American Medical Association. 2012;308(2):157-64. [ Links ]
2. Farkouh ME, Domanski M, Sleeper LA, Siami FS, Dangas G, Mack M, et al. Strategies for multivessel revascularization in patients with diabetes. The New England journal of medicine. 2012;367(25):2375-84. [ Links ]
3. Houlind K, Kjeldsen BJ, Madsen SN, Rasmussen BS, Holme SJ, Nielsen PH, et al. On-pump versus off-pump coronary artery bypass surgery in elderly patients: results from the Danish on-pump versus off-pump randomization study. Circulation. 2012;125(20):2431-9 [ Links ]
4. A.R. Naylor et al; Management of atherosclerotic carotid and vertebral artery disease: 2017 clinical practice guidelines of the European society of vascular surgery; Eur J Vasc Endovasc Surg (2018) 55, 3-81
5. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 2004;351: 1493e501. [ Links ]
6. de Borst GJ, Moll FL. Regarding: ‘carotid angioplasty and stenting in anatomically high-risk patients: safe and durable except for radiation-induced stenosis.’. J Vasc Surg 2010;51:1077 [ Links ]
7. Taylor AJ, Bindeman J, Le TP, et al. Progression of calcified coronary atherosclerosis: relationship to coronary risk factors and carotid intima-media thickness. Atherosclerosis 2008;197:339-45 [ Links ]
8. Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Onnasch JF, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. The Annals of thoracic surgery. 2003;75(2):472-8 [ Links ]
9. John E Castaldo et al; Open Heart Surgery Does Not Increase the Incidence of Ipsilateral Ischemic Stroke in Patients With Asymptomatic Severe Carotid Stenosis; J Stroke Cerebrovasc Dis 2017 Oct;26(10):2154-2159
10. Ehtisham Mahumd et al; Carotid Revascularization Before Open Heart Surgery: The Data-Driven Treatment Strategy; J Coll Cardiol 2013 Nov 19;62(21):1957-1959 [ Links ]
11. Mehdi H Shishehbor et al; A Direct Comparison of Early and Late Outcomes With Three Approaches to Carotid Revascularization and Open Heart Surgery; J Am Coll Cardiol; 2013 Nov 19;62(21):1948-1956; [ Links ]
12. Jay Giri et al; How Should We Address Carotid Artery Stenosis Around the Time of Open-Heart Surgery?; JACC Cardiovasc Interv; 2017 Feb 13;10(3):299-301 [ Links ]
13. Lee EJ, Choi KH, Ryu JS, Jeon SB, Lee SW, Park SW, et al. Stroke risk after coronary artery bypass graft surgery and extent of cerebral artery atherosclerosis. Journal of the American College of Cardiology. 2011;57(18):1811-8 [ Links ]
14. Naylor AR, Bown MJ, et al. Stroke after cardiac surgery and its association with asymptomatic carotid disease: an updated systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2011 May; 41(5):607-24 [ Links ]
15. Paraskevas K, Batchelder A, Bown M, Naylor AR. An updated systematic review and meta-analysis of 30-day outcomes following staged carotid artery stenting and coronary bypass. Eur J Vasc Endovasc Surg 2017; 53:309-19 [ Links ]
16. Shishehbor MH, Venkatachalam S, Sun Z, Rajeswaran J, Kapadia SR, Bajzer C, et al. A direct comparison of early and late outcomes with three approaches to carotid revascularization and open heart surgery. JACC 2013;62:1948e56. [ Links ]
Endereço para correspondência | Dirección para correspondencia | Correspondence
Correio eletrónico: pedro_psousa@hotmail.com (P. Sousa).
Recebido a 15 de setembro de 2019. Aceite a 25 de junho de 2020.