Introduction
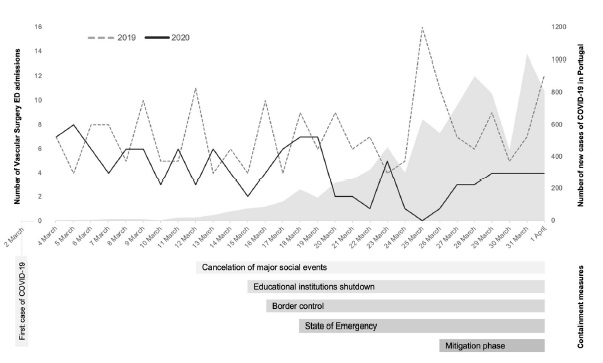
The coronavirus disease 2019 (COVID-19), caused by a new strand of coronavirus, (SARS-CoV-2) first appeared in China by the end of 2019. Since then, it spread globally at an alarming rate and was declared a pandemic by the World Health Organization on March 11th, 20201. In Portugal, the first positive COVID-19 diagnosis had just been confirmed nine days before, on March 2nd. The number of positive cases continued to rise and by the March 18th, 642 new infected people were announced; on that same day, in an unprecedent decision, the Portuguese government issued the first emergency state of its modern history - it lasted for 45 days and ceased on May 2nd with a total of 25190 confirmed cases and 1023 deaths2.
Along with the emergency state came the adoption of social confinement measures; among others, curfew was compulsory for the general population and non-essential services and activities were shutdown. This posed a challenge to the Portuguese National Health System: it had to ensure essential care to the growing number of infected patients and to other potential life-threatening diseases and, at the same time, it had to suspend non-essential activities - in March alone, 9000 elective surgeries were postponed and almost half a million appointments cancelled3.
Our hospital had to adapt, and so did the Vascular Surgery Department: a decision was made to only perform emergent/urgent surgeries based on practice guidelines issued for this specific purpose4; wards were reorganized and outpatient appointments were conducted by telephone.
As the critical phase of the pandemic mitigates, it is important to understand how the imposed measures impacted patient’s healthcare seeking behaviour and how it affected the prognosis of their diseases. Only a few studies have been published so far regarding the impact of COVID-19 pandemic in the ED of Portuguese hospitals; however, all of them confirm the drastic reduction on patients visits to the emergency services, reporting decreases greater than 40 to 50%5-7. This study aims to evaluate the impact of these measures on the Vascular Surgery ED admissions, by comparing clinical and demographic characteristics of patients visiting the ED during the pandemic and the homologous period of 2019.
Materials and methods
We conducted this retrospective observational study in Centro Hospitalar Universitário do Porto (CHUP), a tertiary hospital in northern Portugal, provider for the healthcare of approximately 6% of the national population. In this hospital, the Vascular Surgery ED runs 24 hours a day with at least one physician permanently present; no changes were implemented in the ED personnel during the COVID-19 pandemic8. Patients can be directly referred to this specialty through the Manchester Triage System (MTS), which is a resource implemented twenty years ago in Portuguese hospitals to manage patients’ clinical risk at the ED admission based on their chief complaint and objective severity criteria. It defines the level of priority and the recommend time to first clinical observation (Figure 2)9.
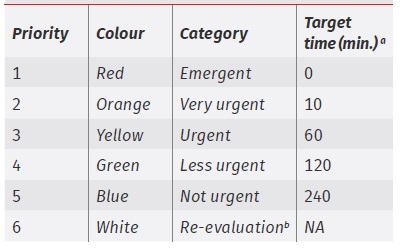
Figure 2 The Manchester Triage System levels of priority aRecommended target time from admission to first clinical evaluation. bWhite colour is assigned to patients refered to the ED for clinical re-evaluation or administrative reasons. NA: not applicable
Study population and variables
We included patients admitted to the Vascular Surgery ED between March 4th and April 1st, 2020 - two weeks before and two weeks after the governmental implementation of the state of emergency in our country due to the COVID-19 pandemic; we then compared these patients with those admitted to the same ED during the homologous period of 2019. Individual medical records were revised to obtain further information: patients demographics and characteristics, clinical severity under the MTS, final diagnosis, need for hospitalization or emergent/urgent surgery, in-hospital length of stay and mortality within 30 days of hospital discharge.
Statistical analysis
Patients personal information were anonymized prior to data analysis. Descriptive statistics were applied according to data type: categorical variables were presented as frequencies and continuous variables as mean and standard deviation or median and interquartile range according to their normal distribution. For statistical analysis, all observations were treated as independent. Despite the slight right-skewness in patients’ age, its mean was assumed to have a normal distribution under the central limit theorem; the homogeneity of variances assumption was also met by descriptive analysis and formal tests (equality of variances F-Test). Therefore, age comparison by year was performed using unpaired t-test. On the contrary, in-hospital length of stay showed no normal distribution and was compared using Mann-Whitney U test. Categorical variables were compared using χ2 tests. Statistical significance was set at 0.05 and analysis was performed using IBM® SPSS® Statistics 26 (National Opinion Research Center, USA).
Results
A total of 119 patients visited the Vascular Surgery ED of CHUP during the pandemic period, which represents a reduction of 43.3% compared to the previous year. From March 4th until March 20th, a mean of 5.2 patients were admitted per day; from the following day until April 1st, the average contracted to just 2.6 with even no patients entering the ED on the March 25th (Figure 1).
Table 1 summarizes the demographics and characteristics of all patients collected, split by year with their respective variation. Men comprised the majority of patients in both years. The proportion of women visiting the ED was significantly lower in 2020 compared to 2019 (P=0.015). Patient’s average age overlapped at around 64-65 years with no significant differences in means between both years.
The MTS attributed a significantly lower number of high-priority levels (yellow and orange) to patients visiting the ED in 2020 (P=0.048). In relative terms, 87.6% of all patients admitted in 2019 received a high-priority level, whilst in 2020 only three-quarters required this level of priority. No emergent (red) cases were recorded during both years.
The number of patients requiring hospitalization or emergent/urgent surgery were identical in both years; however, considering the absolute reduction of patients admitted to the ED in 2020, a significantly higher proportion of patients in the latter year required in-hospital treatment or emergent/urgent surgery (P<0.001 and P=0.002, respectively). In fact, 40% of all patients entering the ED in 2020 remained hospitalized and more than one-quarter underwent emergent/urgent surgery. Regarding in-hospital length of stay, no significant differences were noted as patients in 2020 only remained hospitalized a median of two more days before discharge compared to 2019. Early mortality remained similar during both periods.
The most prevalent diagnosis during the pandemic were chronic limb threatening ischemia (CLTI) - comprising almost half of the patients - deep vein thrombosis, and acute limb ischemia. Noticeably, in 2019, non-vascular limb pain and post-operative pain were commonly diagnosed (in fact, only topped by CLTI), but both saw a reduction of more than 80% when the pandemic occurred (Table 2).
Discussion
Data from the Organization for Economic Cooperation and Development (OECD) reveals that Portugal is one of the highest emergency services users per capita10. As the COVID-19 pandemic expanded, a reduction on ED admissions was to be expected, especially among the eldest population: moral conscience not to overload already on stress healthcare services, limitations on displacements and isolation imposed by government decree along with the fear and consequent avoidance of contamination may explain this hypothesis. Our study shows a significant reduction of 43.3% on the demand for the same services, compared to the previous year. In fact, a similar study conducted in a different Portuguese tertiary hospital reveals similar reductions on Vascular Surgery emergency visits11. As suggested, the eldest patients refrained the most from attending the ED during the pandemic, as noticed by the more than 60% reduction in the 80 or plus years old age group.
The pandemic might have also influenced patients bearing more severe diseases: these patients, who typically present with more serious and higher-priority complaints under the MTS saw a significantly reduction of admissions compared to 2019. Such phenomena was also observed in the ED of other surgery specialties12. Nonetheless, despite the overall decrease in patients attending the ED during this critical period, the proportion of those requiring hospitalization or urgent/emergent surgery was significantly higher. This finding are in conformity with the literature and may reflect both patients delay on seeking for healthcare services - thus presenting at the ED with more advanced and critical diseases - and the lack of proper follow-up at the outpatient and general practitioner clinics, which were severely affected by the sudden need of institutional reorganization5,11. Following hospitalization, in-hospital caregiving response may be assumed as adequate, as length of stay and early mortality did not significantly differ from that of 2019.
CLTI is a clinical syndrome defined by the presence of peripheral artery disease (PAD) in combination with rest pain, gangrene, or a lower limb ulceration >2 weeks duration and it represents less than 10% of all PAD patients13. According to a study conducted in 2008 by the Portuguese Society for Angiology and Vascular Surgery, the prevalence of PAD in Portugal is around 6%14, inevitably making CLTI a prevalent problem in a hospital setting. CLTI remained the top problem diagnosed at the ED even during the COVID-19 crisis - actually, this condition was diagnosed in a higher proportion of patients in 2020 than in 2019 (41.2% vs. 30%, respectively) - and may have played an important role in the increase of hospitalizations and urgent/emergent surgeries; this hypothesis is beyond the scope of this work, but further research to assess its real impact is essential to prepare the Vascular Surgery unit for future pandemic waves. The higher prevalence of CLTI among male patients may help explain the significant widder sex gap of patients between the studied years13.
Table 1 Demographics and characteristics of Vascular Surgery visits during the COVID-19 pandemic (March 4th to April 1st) compared to the homologous period in 2019
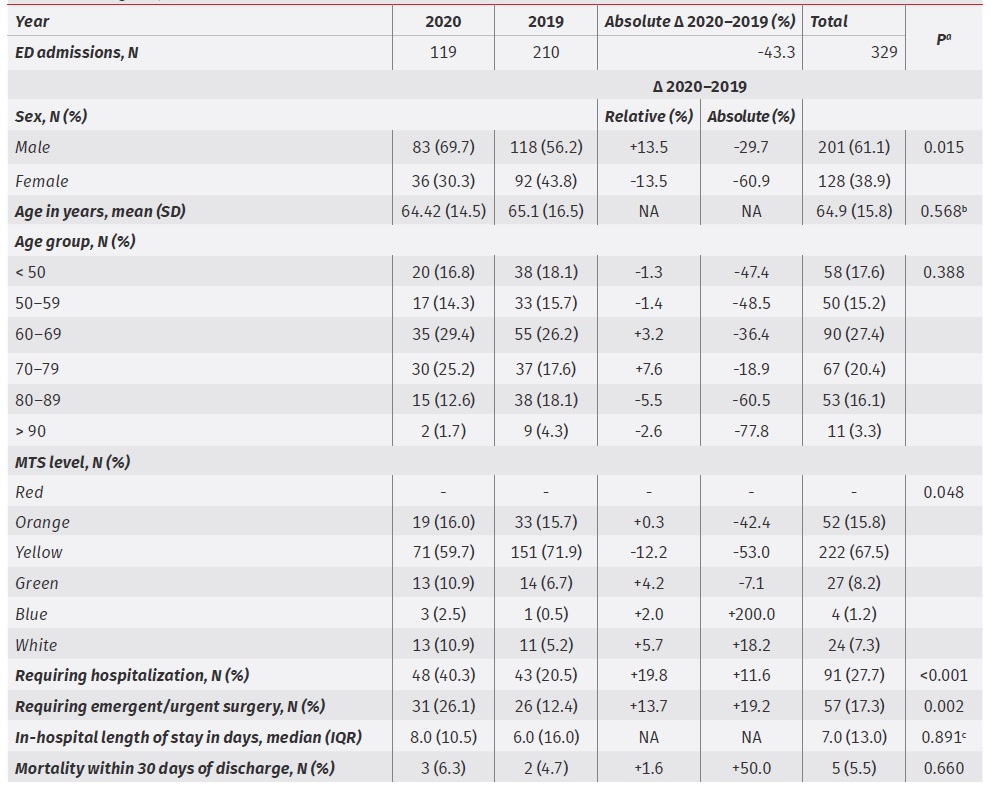
NA: not applicable; ED: emergency department; MTS: Manchester Triage system; SD: standard deviation; IQR: interquartile range.
a P is χ2 test (with Fisher’s exact test applied when appropriate) comparing each variable between 2020 and 2019.
b P is unpaired t-test comparing age between 2020 and 2019.
c P is Mann-Whitney U test comparing in-hospital length of stay between 2020 and 2019.
The absolute decrease in high-priority (yellow and orange) complaints may reflect a reality where patients with serious or potentially serious conditions did not seek healthcare during the critical months of the pandemic; this may trigger a ‘rebound’ effect leading to an increase in limb or life-threating events in the short-term, such as irreversible ischemia, uncontrolled pain or unmanageable ulcers in CLTI patients, with its associated risk of limb amputation and death. Once again, this phenomenon is not ascertained in our study but should be investigated thoroughly as it may have serious consequences for both the patients and the clinical practice in Vascular Surgery.
Non-vascular limb pain and post-operative pain were among the most frequent diagnosis established in 2019 with no cases requiring in-hospital treatment during both years. The pandemic impact on healthcare seeking behaviour and the cancelation of most surgical procedures help explain this abrupt reduction.
Limitations
This study is a retrospective analysis (with its inherent limitations and bias) of clinical records written by physicians during their activity in the emergency department of a large tertiary hospital - time and organization constraints as well as a lack of diagnosis coding may interfere with data quality. Also, the timeline of our study spans for only 29 days, not reflecting the entire nature nor consequences of the pandemic so one can only hypothesise about mid to long-term effects.
Conclusion
We found a 43.3% decrease in the number of visits to the Vascular Surgery emergency department in the first month after the inaugural diagnosis of COVID-19 in Portugal.
There was a significant reduction of patients with high-priority complaints, but those of presented to the ED had more severe and advanced disease, reflected by the increased proportion on hospitalization and emergent/urgent surgery requirements. Fear of infection and mobility limitations imposed by the quarantine may dissuade patients from attending the ED and delay proper healthcare. Mid to long-term impact of such behaviour on morbimortality should be determined to evaluate the quality of response of healthcare services to the pandemic.