Caso clínico
Vintage Technique in Vascular Surgery: Lumbar sympathectomy in critical limb ischemia.
Técnica Vintage em Cirurgia Vascular: Simpatectomia lombar na isquemia crítica de membro.
José Luis Durán Mariño1
Eva Lucía Martínez Gallego1
Eva Pérez Carballo1
Francisco Javier Rielo Arias1
Juan Pena Holguín1
Laura Velásquez Castañeda2
1 Department of Vascular Surgery; Lucus Augusti Universitary Hospital, Lugo, Spain
2 Department of Vascular Surgery; IMED Levante Hospital, Benidorm-Alicante, Spain
Abstract
Introduction:
Tromboangiitis Obliterans or Buerguer's disease is one of the expresions of the peripheral arterial disease; its main feauture is the absence of average distal outflow that precludes direct revascularization surgery; lumbar sympathectomy was carried out to treat this condition with acceptable results but nowadays this technique is described as obsolete; many young vascular surgeons have not even heard about it and most of them have never seen a lumbar sympathectomy for the treatment of patients with critical limb ischemia.
Case report:
A 39-year-old woman admitted with critical limb ischemia due to popliteal artery occlusion without average distal outflow, treated by a lumbar sympathectomy as a resource technique.
Discussion:
Today, endovascular treatment is the first option for the critical limb ischemia in most cases; althoug tromboangiitis obliterans is less frequent nowadays, exists, and this is one of the situations where endovascular treatment does not work; what's more, direct surgery is also not possible.
Conclusions:
Lumbar sympathectomy can work not only in this scenary of Buerguer's disease; it can be used as resource technique when the first approach with direct surgery has failed and there is not more options to limb salvage; thus, lumbar sympathectomy should be part of the therapeutic arsenal of any vascular surgeon.
Keywords: Critical limb ischemia; Buerguer's disease; Lumbar sympathectomy
Resumo
Introdução:
A tromboangeíte Obliterante ou doença de Buerguer é uma das expressões da doença arterial periférica; a sua principal característica é a oclusão dos principais eixos arteriais distais, o que impede a cirurgia de revascularização direta; A simpatectomia lombar foi já utilizada para tratar essa condição com resultados aceitáveis, mas hoje em dia esta técnica é considerada obsoleta; muitos jovens cirurgiões vasculares nem mesmo ouviram falar e a maioria deles nunca viu uma simpatectomia lombar para o tratamento de doentes com isquemia crítica de membro.
Caso-clínico:
Mulher de 39 anos admitida com isquemia crítica de membro consequente à oclusão da artéria poplítea sem eixos distais permeáveis, tratada com a realização de uma simpatectomia lombar como técnica de recurso.
Discussão:
O tratamento endovascular é a primeira opção para a isquemia crítica de membro de causa aterosclerótica; embora a tromboangeíte obliterante seja menos frequente, ainda se observa nos dias de hoje, e é uma das situações em que o tratamento endovascular é ineficaz; além disso, a revascularização por cirurgia clássica, na maioria das vezes, também não é possível.
Conclusão:
A simpatectomia lombar pode ser eficaz, não apenas neste cenário da doença de Buerguer; pode ser usada como técnica de recurso quando a primeira abordagem pela cirurgia de revascularização falha e não há mais opções de salvamento do membro; assim, a simpatectomia lombar deve fazer parte do arsenal terapêutico de qualquer cirurgião vascular.
Palavras-chave: Isquemia crítica de membro; Doença de Buerguer; Simpatectomia lombar
Introduction
Lumbar sympathectomy was introduced by the Argentinian professor Julio Díez almost a century ago, for the treatment of Tromboangiitis Obliterans in the lower extremities1.
This surgical technique was widely accepted and enjoyed diffusion among all surgical schools from the second third of the twentieth century, due to the absence of other alternative therapies for patients with peripheral artery diseases with risk of limb loss2-6; its practice was generalized for several decades, based on two fundamental premises: its undeniable hyperemiant action7 and the absence of other alternative therapies for patients with peripheral artery diseases, when amputation was considered the only surgical alternative to sympathectomy.
The advent and developement of reconstructive arterial surgery made lumbar sympathectomy fall into disuse8,9; nowadays this technique is practically abandoned and even it's unknown for mostly of young vascular surgeons.
Case report
A female, thirty-nine year-old, was admitted at the emergency department of our hospital due to a five month clinical onset of gemelar claudication, coldness, tightness in the sole and paraesthesia in the toes of the left foot; the patient had been previously diagnosed as Morton's Neuroma and had been treated with corticoid infiltrations by the Ortopedic Department of her local hospital without improvement.
At the time of her admission into our service, she presented a necrotic lesion on the first toe, and an interdigital lesion between first and second toes of the left foot with lymphangitis (Figure 1a); she had not temperature, but referred rest pain.
Vascular examination showed a weak left popliteal pulse and absence of distal pulses in this extremity, while were present in the right lower extremity. There was also, no Doppler signal in the left foot, all it in the context of critical limb ischemia Rutherford 6.
Medical treatment was initiated with low molecular weight heparin at full dose and intravenous prostaglandin E1 (three week cycle), analgesia, suspension of hormone treatment and debridement on the foot wound.
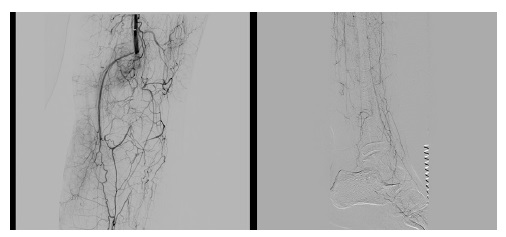
After ruling out other causes of ischemia (embolic and auto-immune), a selective angiography of the left femoropopliteal sector was carried out; an occlusion was identified at the level of the second portion of the popliteal artery, without average distal outflow, but with abundant colateral circulation in this leg (Figure 1b). Intra-arterial fibrinolytic therapy with urokinase was tried without any success.
The evolution of the ischemia lesions were unfavourable despite vasodilatory and debridement treatment, and due to the impossibilty of carrying out direct revascularization surgery, a left lumbar sympathectomy was done; the patient soon experienced a local improvement in the temperature of the foot, relief the rest pain and the foot wounds also slowly started to improve (Figure 2a). Now, at seven years of follow-up, the patient is asymptomatic, without claudication (Figure 2b).
Discussion
Since the discovery of the vasomotor nerves by Claude Bernard in 1851, the idea of sympathetic denervation in order to treat ischemia in extremities stimulating arterial vasodilatation was an objective pursued by all the angiologists of the time. The first to try it was René Leriche, who proposed a periarterial sympathectomy in 1913, but with bad results. The Argentinian Julio Díez carried out the first lumbar ganglionectomy with good clinical results in 1924, and he continued treating diverse patients with this technique, until 1931, when he published his results in the Journal de Chirurgie1.
It is estimated that the total length of all the microvessels of a man can reach 100.000 km and a total surface area of about 6.500 m ; around 20% of the total correponds to the lower extremities, based on Burton's studies10; for this reason, lumbar sympathectomy can be used as an alternative route to vascularize the ischemic tissues, especially in patients who aren't affected by medical diabetes, in whom the very metabolic neuropathy limits the vasodilatory response to sympathetic denervation11.
For several decades, Diez's sympathectomy was the only tool for management of limb ischemia until the advent of direct arterial surgery; Cid Dos Santos described thromboendarterectomy in 194612 and two years later Jean Kunlin advocated derivative surgery13, so hyperemiant surgery was forgotten until the point reached today, when it's an obsolete technique, unknown by mostly of young vascular surgeons and those in training.
One main weakness of lumbar sympathectomy is the absense of solid trials because it's decline coincided with the boom of Based Evidence Medicine14; with the advent of new compassive treatments to approach the critical ischemia like stemcell technique15 and the poor knowledge of lumbar sympathectomy, it's difficult that new evidence will be published in the future. However, lumbar sympathectomy can have a role in few patients where revascularization is not viable.
Conclusions
Lumbar sympathectomy is a feasible technique with low risk of complications; it can be done in specific scenaries of critical limb ischemia and can be resolutive in expertal hands as a resource technique, when standard techiques or other compassive procedures had been discarted. The knowledge of this technique can mean the difference between patient limb salvage or not, so lumbar sympathectomy should be on mind of any vascular surgeon.
References
1. Díez J. Le traitement de la thrombo-angéite oblitérante des membres infériours par la résection du sympathique lombaire (expérience basée sur 75 cas opérés et 6 années d'observations. Journal de Chirurgie, 1931; 37(2):161-231.
[ Links ]
2. Freeman N.E., Leeds F.H., Gardner R.E. Sympathectomy for obliterative arterial disease. Indications and contraindications. Annals of Surgery, 1947; 126(6):873-895.
[ Links ]
3. Imparato A.M. Lumbar sympathectomy. Role in the treatment of occlusive arterial disease in the lower extremities. Surgical Clinics of North America, 1979; 59(4):719-735.
[ Links ]
4. Erichsen HG. Lumbar sympathectomy in obliterative arteriosclerosis. Should it still be performed? Scand Cardiovasc J. 1979;13(3):333-337. doi: https://doi.org/10.3109/14017437909100574
[ Links ]
5. Dalessandri K.M., Carson S.N., Tillman P., Talken L., Wong H.N. Effect of lumbar sympathectomy in distal arterial obstruction. Arch. Surg. 1983; 118:1157-1160.
[ Links ]
6. van der Stricht JP. Effect of lumbar sympathectomy on the lower extremity. J Cardiovasc Surg (Torino). 1979;20(3):301-311.
[ Links ]
7. Sanni A. Is sympathectomy of benefit in critical leg ischaemia not amenable to revascularisation? Interact Cardiovasc Thorac Surg. 2005;4(5):478-483. doi: https://doi.org/10.1510/icvts.2005.115410
[ Links ]
8. Fulton RL, Blakeley WR. Lumbar sympathectomy: A procedure of questionable value in the treatment of arteriosclerosis obliterans of the legs. Am J Surg. 1968;116(5):735-744. doi: https://doi.org/10.1016/0002-9610(68)90359-0
[ Links ]
9. Gordon A, Zechmeister K, Collin J. The role of sympathectomy in current surgical practice. Eur J Vasc Surg. 1994;8(2):129-137. doi: https://doi.org/10.1016/S0950-821X(05)80447-5
[ Links ]
10. Pratesi Franco. Microcirculazione e microangiologia. Edizione Minerva Médica (Torino). 1990; 3-118.
[ Links ]
11 Friedman SA , Frieberg P, Colton J. Vasomotor tone in diabetic neuropathy. Ann. Intern Med197277353-355
[ Links ]
12. Cid Dos Santos J. The diagnosis and treatment of vascular obstruction. Gaz Med Port. 1948;1(3):631-643.
[ Links ]
13. Menzoian JO, Koshar AL, Rodrigues N. Alexis Carrel, Rene Leriche, Jean Kunlin, and the history of bypass surgery. J Vasc Surg. 2011;54(2):571-574. doi: https://doi.org/10.1016/j.jvs.2011.04.028
[ Links ]
14. Karanth VKL, Karanth TK, Karanth L. Lumbar sympathectomy techniques for critical lower limb ischaemia due to non-reconstructable peripheral arterial disease. Cochrane Database Syst Rev. 2016;2016(12). doi: https://doi.org/10.1002/14651858.CD011519.pub2
[ Links ]
15. Qadura M, Terenzi DC, Verma S, Al-Omran M, Hess DA. Concise Review: Cell Therapy for Critical Limb Ischemia: An Integrated Review of Preclinical and Clinical Studies. Stem Cells. 2018;36(2):161-171. doi: https://doi.org/10.1002/stem.2751
[ Links ]