Introduction
Traumatic Thoracic Aortic Injury (TTAI) or Blunt Thoracic Aortic Injury results from rapid deceleration, usually from motor vehicle accidents or due to falls from a significant height(1). It happens in less than 1% of car accidents, but is responsible for 16% of deaths, owing to the majority of patients not arriving to the hospital in time (80-85% pre-hospital mortality)(2).
TTAI occurs at the aortic isthmus in over 60% of patients, just distal to the left subclavian artery, but other sites can be affected(3). Azizzadeh A, et al(4), described a classification system for TTAI in which four types are considered. Type I corresponds to intimal tear, type II to intramural hematoma, type III to pseudoaneurysm and type IV to rupture.
Several recommendations have been proposed concerning operative and non-operative management for each type of lesion. It has been established that rupture of the intimal and medial layers occurs first, and that progression to rupture of the adventitia is unpredictable - for many patients intimal injury may never progress to rupture, and for those in which it happens, the time interval may be from seconds to years(1).
Type I injuries have been suggested to be adequately managed by nonoperative measures, such as aggressive heart rate and blood pressure control along with serial imaging(2). In these patients, effective anti-impulse therapy reduces the risk of rupture from 12% to 1,5%(3). The desired systolic blood pressure is of 100mmHg, with a mean arterial pressure of no more than 80mmHg, and a heart rate lower than 100bpm.
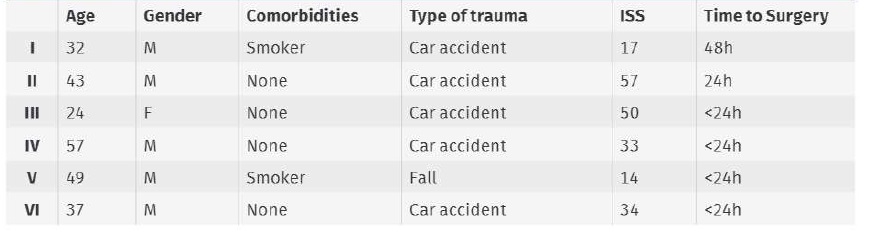
Table 1 Baseline characteristics of the six patients admitted for TTAI. Coding with I-VI is maintained in the following tables
This can be achieved by intravenous esmolol (rapidly acting beta blocker with a short half-life), that can be complemented with intravenous nitroglycerin or nitroprusside. If the patient has concurrent severe injuries that preclude aggressive blood pressure control, such as traumatic brain or spinal cord injuries, these may impede nonoperative management.
For type II-IV lesions, ESVS clinical practice guidelines(5) recommend urgent TEVAR, although some studies are now advocating expectant management of type II lesions or delayed repair for hemodynamically stable patients with type II or III lesions. A delayed repair is particularly beneficial for patients with severe coexisting injuries, in which stabilization and medical optimization prior to aortic surgery might actually reduce mortality(3).
The purpose of this study is to present our institutional experience with the surgical treatment of TTAI.
Material and methods
The authors declare that they have followed the protocols of their center on the publication of patient data and comply with the Helsinki declaration on research ethics. This study is a retrospective analysis of discharge data for patients admitted with TTAI between 2010 and 2019 was extracted from our institutional administrative database (level 1 trauma center). We extracted ICD-9 procedure code 39.73 - endovascular implantation of graft in the thoracic aorta and cross-checked with hospital registries to identify all TTAI cases. Follow-up was extracted from patient charts. A descriptive analysis of the data was performed.
The primary endpoints were primary technical and clinical success (successful deployment of the endovascular device at the intended location, survival in the first 24 hours, absence of type I or type III endoleaks as evidenced by procedural angiography and absence of graft obstruction) as defined by the reporting standards for thoracic endovascular aortic repair(6). Secondary endpoints were time to diagnosis and to surgical procedure relative to traumatic event, overall mortality, ongoing primary clinical success (freedom from the need for an unplanned additional surgical or endovascular procedure, freedom from death as a result of treatment or as a result of the original pathology that was treated, absence of type I or III endoleaks, absence of infection or aortic thrombosis, absence of aneurysm expansion or rupture, arrest of the original pathologic process without a new thoracic aortic pathology as a result of the intervention), and procedure specifications (upper limb revascularization, spinal drainage, systemic heparinization and endograft oversizing).
The aortic diameter was evaluated using the Horos® software and measurements were made at distal limit of the left carotid artery ostium or 2 cm above the lesion, in the antero-posterior axis and outer to outer fashion. Oversizing was calculated based in these determinations.
Results
We identified six patients with TTAI who underwent TEVAR between 2010 and 2019 (Table 1). All were victims of high impact deceleration trauma, five car accidents and one fall. Ages varied from 24 to 57 years old (mean age 40 years old), two were smokers with no other know diseases. Additional major injuries were present in all patients as manifested by an Injury Severity Score of 14 to 57.
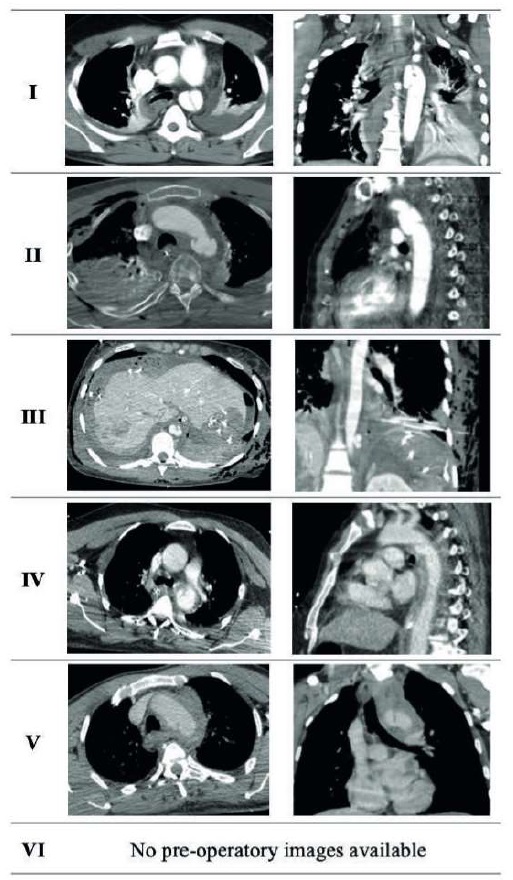
All patients were submitted to CTA at admission (Table 2) which allowed for early diagnosis of TTAI. According to the Classification of TTAI, grade III lesions were present in all six patients. Five patients had pseudoaneurysms at the aortic isthmus, and one patient had a pseudoaneurysm in the transition of the toraco-abdominal aorta. Five patients were submitted to urgent repair with TEVAR, with time from diagnosis to surgery being less than 24 hours. One patient was considered for delayed repair but submitted to surgery for worsening symptoms at 48 hours (progression to hemothorax).
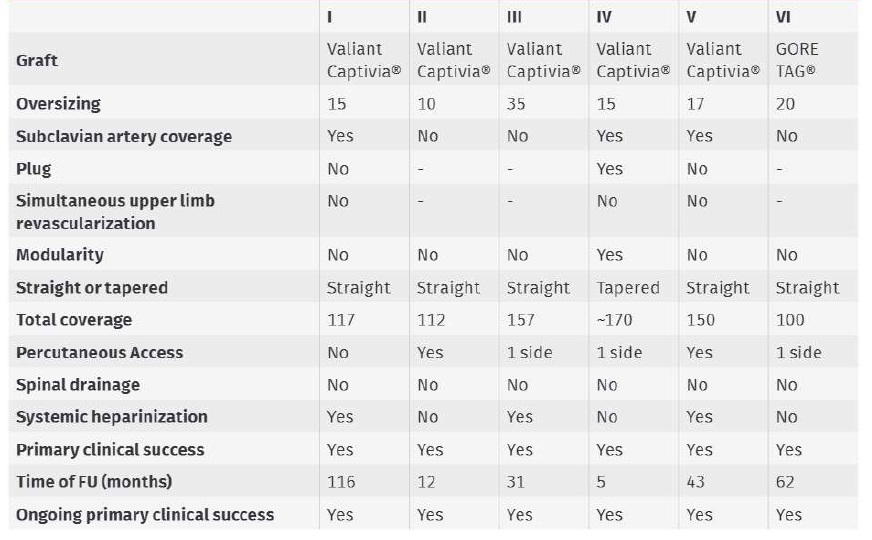
All patients underwent TEVAR with 100% technical and clinical success (Table 3). The median oversizing of the endograft was 16% (10-35%). Valiant Captivia® thoracic stent graft was used in five patients, and a GORE TAG® Thoracic Endoprosthesis was used in one. Length of coverage was between 100 and 170mm. Spinal drainage was not used in any case and there were no neurologic events. Half the patients were submitted to the procedure under systemic heparinization. One patient was operated on with an open femoral access, two with percutaneous femoral access and the remaining three with one side with open femoral access and the other with a percutaneous approach.
Three patients had a lesion that extended above the subclavian artery and consequently required subclavian coverage, but no patient was submitted to upper limb revascularization and none had manifestations of upper limb ischemia. Of the patients requiring subclavian coverage, a plug was used in only one.
All patients had a follow-up CT scan in the first year with no complications (no new, expanding, or progressing lesions, no device migration, no stent fracture and no endoleak presence). There was no in-hospital mortality nor mortality during follow-up (median duration of 35,5 months with an IIQ of 84,5 months) and the ongoing primary clinical success is 100%.
Discussion
TEVAR is a straightforward modality of treatment for TTAI when compared with the open surgery alternative and has been proven to be safer and to significantly reduce mortality.
In a large study conducted about TTAI in the New York state between the years 2000 and 2007, 328 patients were submitted to either open or endovascular surgery and results were compared(7). There was a statistically significant reduction of in-hospital mortality, with 6% after TEVAR and 17% after open surgery. Pulmonary complications were significantly reduced as well, as was paraplegia (7% after open surgery, and less than 1% after TEVAR). In a meta-analysis conducted by the SVS(8) the mortality was also significantly lower for endovascular repair (9%) compared to open repair (19%) and nonoperative management (46%). The risk of spinal cord ischemia was 3% for endovascular repair and 9% for open repair, and the risk of end-stage renal disease was 5% for endovascular repair and 8% for open surgery.
However, some surgical limitations still exist, such as need for reintervention (endoleak is identified in 9% of patients(7)), need for revascularization of the left subclavian artery if upper limb ischemia ensues (due to anatomic proximity to the subclavian ostium, coverage is often necessary), risk of paraplegia and stroke. In our series TEVAR had excellent results in terms of primary clinical and technical success, and of ongoing primary clinical success.
Controversy exists about the need for systematic left subclavian artery revascularization and timing for said revascularization, use of systemic heparinization in the setting of multiple coexisting injuries, routine placement of spinal drainage, use of percutaneous access, oversizing of the endograft, type of anesthesia and follow-up strategy(7,9).
In our center, and according to current literature, upper limb revascularization is never done systematically in emergency cases, being reserved for patients that manifest with upper limb ischemia or neurological symptoms. Spinal drainage is not used routinely as well, especially in cases of TTAI, due to the perception that a relatively small coverage of the thoracic aorta is performed, and that an epidural puncture in a trauma patient may be more deleterious, being reserved for patients with post-operatory neurologic symptoms.
Systemic heparinization is considered based on the individual assessment of thrombophilic and hemorrhagic potential, or on contra-indications to anticoagulation. Preference for anticoagulation during the procedure is given, with reversion with protamine in the end of the procedure if necessary.
Percutaneous femoral access is faster to achieve and less prone to infectious complications but might be inadequate in an urgent setting in which acute access complications such as bleeding might significantly increase procedure time. As in all other matters the decision is individualized balancing the pros and cons of each approach.
Once TEVAR is a relatively recent surgical procedure there are still few data on long term follow-up and late complications. For TTAI in particular, patients are typically young, and present no concomitant aortic disease, so the conclusions withdrawn from thoracic aneurism repair may not apply. One concern regarding the use of endografts in healthy aortas is the potential remodeling induced by the prosthetic material, that may in the long term diminish aortic plasticity and hypothetically cause cardiac dysfunction. None of the patients in this study has any changes in the post-operatory cardiac function, but the mean follow-up is still short for evaluation of this variable.
There may be limitations inherent to retrospective data analysis, which is prone to information bias, given most information is withdrawn from existing medical records. Additionally, the ICD-9 code used to select patients, which as a procedure code, precluded all patients not submitted to surgery. We found that, once this is a rare diagnosis, most patients were not classified appropriately diagnosis-wise. This means that all patients treated conservatively are not included in the sample. Finally, the small number of patients does not allow for an adequate control group and outcome comparison.
Conclusions
Endovascular repair is a safe and effective therapy for TTAI even in patients with multiple trauma, and good mid-term results are expected. The procedure specifications such as the need for upper limb revascularization, use of spinal drainage, endograft oversizing, and systemic heparinization are still mostly center and surgeon dependent. The long-term consequences need to be clarified.