Introduction
Peripheral artery disease (PAD) has traditionally been identified as a male-dominant disease. However, PAD prevalence increases with age, and a larger percentage of the elderly patients are women. On the other hand, there has been a steeper decline in male smoking rates compared with female smoking. Nowadays, the incidence of PAD in men and women is similar(1).
Sex-specific data on outcomes after lower limb revascularization associate the female gender with worse surgical outcomes, particularly after open procedures. Women were found to be more likely to suffer from procedure complications, limb loss, and mortality than their male counterparts(1,2).
These differences may be related to an older age at presentation, smaller vessel size, poorer overall health status, or a more severe clinical and anatomical disease burden at presentation in female patients(2).
This study aims to identify differences in all major outcomes after lower limb revascularization between female and male patients (primary goals). It also aims to identify sex-associated dissimilarities in demographic characteristics and clinical presentation (secondary goals).
Methods
This is a retrospective, observational, single-center study. It includes all lower limbs without prior revascularization procedures in patients with diagnosed PAD, which underwent a revascularization procedure in a tertiary university hospital between January 2017 and December 2018. Exclusion criteria comprised lower limbs that had previously undergone a revascularization procedure and lower limbs that underwent a revascularization attempt without success in treating or bypassing the occlusive lesion.
Patient, procedure and outcome details were collected from medical records. It included analysis of admission and discharge documents, hospitalization and outpatient registries, and review of available follow-up exams (ultrasound, CTA or invasive angiography). Chronic limb-threatening ischemia (CLTI) was defined as objectively documented atherosclerotic PAD in association with ischemic rest pain or tissue loss (ulceration or gangrene). In the presence of CLTI, limbs and wounds were classified according to WIfI (wound, ischemia, foot infection) system, and PAD was staged according to the GLASS (Global Limb Anatomical Staging) system after arteriography evaluation.
Women's limbs Group (F) was compared against men's limbs Group (M).
The primary endpoint was major amputation, and secondary endpoints were diagnosed vascular procedure restenosis/occlusion, vascular reintervention and overall survival.
Diagnosed vascular procedure restenosis/occlusion was determined on follow-up exams, including ultrasound, CTA or invasive arteriography. In our department, patients undergo vascular surgeon observation and lower limb vascular ultrasound on an outpatient basis a month after discharge, six months after discharge, yearly after that, and every time symptoms recur or become more severe. If the patients have healing wounds, they are clinically followed closer, usually every two weeks.
A vascular reintervention was defined as a vascular revascularization procedure performed on the same limb. It included procedures performed: 1) after a diagnosis of vascular procedure restenosis/occlusion associated with life-limiting claudication or CLTI; 2) after a diagnosis of asymptomatic failing-graft; 3) after vascular procedures that did not relieve previous symptoms, despite having treated arterial anatomic lesions; 4) after symptoms recurrence due to atherosclerosis progression in another sector.
Subgroup analysis was undertaken considering open, endovascular or hybrid procedures. It was also performed for procedures addressing inflow, outflow, or simultaneous inflow and outflow disease.
Written consent was obtained from the patient for the planned procedure and anonymous data usage for scientific purposes.
Quantitative variables are expressed as mean ± standard deviations (SD) or median (interquartile range - IQR), as appropriate. Qualitative variables are expressed as absolute values and percentages. Shapiro-Wilk normative tests were used to access distribution patterns in quantitative variables. Student's t-test, A-nova one way, and respective non-parametric tests and χ2 and proper adjustments were used on univariate analysis. Correlations tests have been applied when relating quantitative variables. A p-value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS 24.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Group M included 324 male lower limbs. Group F included 96 female lower limbs.
Group F included older patients than group M (p<0,001). Group F had a mean age of 71,7±1,2 years, and Group M had a mean age of 67,5±0,6 years.
Baseline characteristics are depicted in table 1. There were no significant differences between groups, aside from a higher prevalence of smoking in Group M (70% vs. 21%; p<0.001) and hypertension in Group F (90% vs. 80%; p=0,031).
The severity of limb ischemia was not different between groups. 83% of procedures in Group F (N=80) and 79% of procedures in Group M (N=255) were performed due to chronic limb-threatening ischemia (CLTI). 17% (N=16) and 21% (N=69) of procedures were performed due to lifestyle-limiting claudication in Group F and Group M, respectively (p=0,321).
If CLTI, we found no statistically significant difference between groups regarding wound or infection grading (in WIfI system) and femoropopliteal or below-the-ankle (BTA) anatomic disease staging (in GLASS system) - Table 2. Group M was more likely to have common femoral artery (CFA) disease (p=0,001) and higher stages of aortoiliac disease (in GLASS system; p=0,014). Group F had more severe below-the-knee (BTK) disease (p=0,012).
The median follow-up was 22 months.
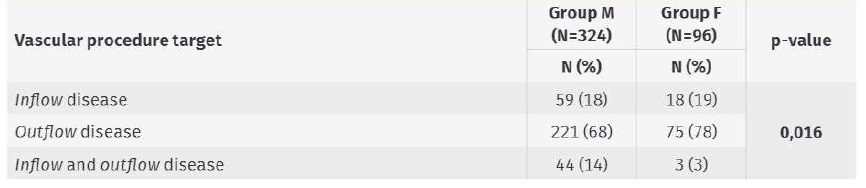
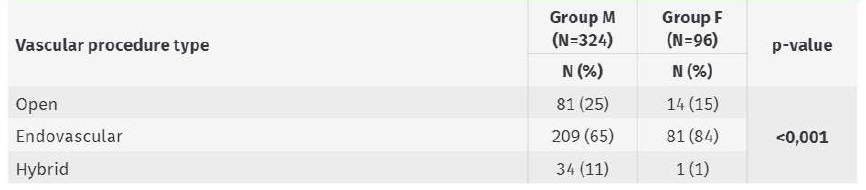
The vascular procedures to treat different levels affected by occlusive disease were associated with gender (Table 3; p=0,016). Group F underwent more outflow procedures (78% vs. 68% in Group M) and fewer simultaneous inflow and outflow procedures (3% vs. 14% in Group M).
We found an association between gender and the type of revascularization procedure performed (Table 4; p<0.001). Group F had a higher proportion of endovascular procedures (84% vs. 65% in Group M).
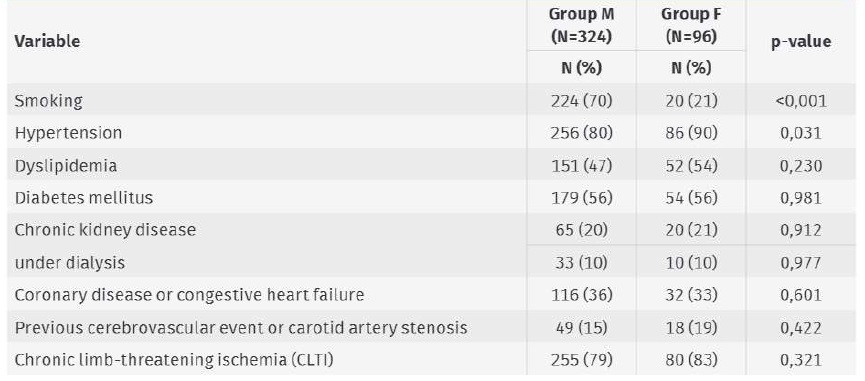
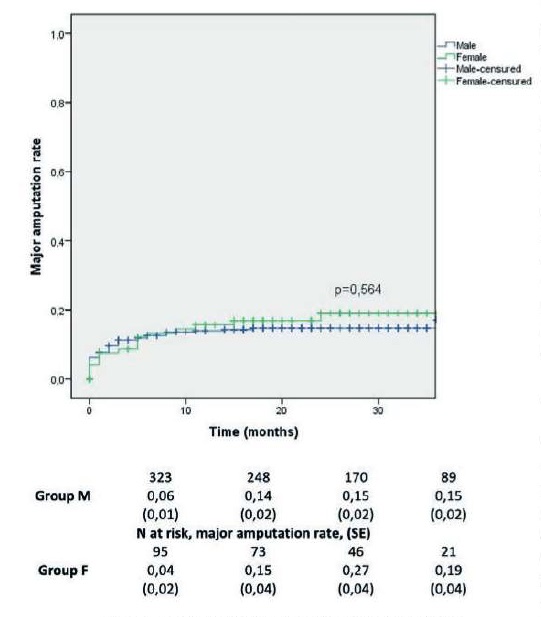
Major amputation rates in Group M and Group F were 8±2% and 8±3% at 1 month, 14±2% and 16±4% at 1 year, and 15±2% and 19±4% at 2 years, respectively (Image 1; p=0,564).
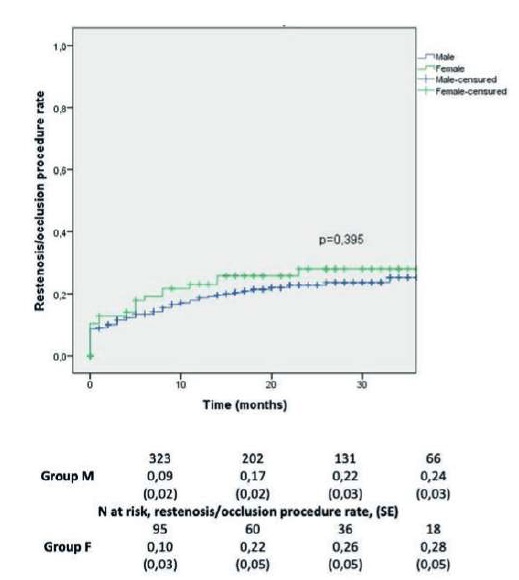
Diagnosed procedure restenosis/occlusion rates in Group M and Group F were 9±2% and 13±4% at 1 month, 19±2% and 23±5% at 1 year, and 23±3% and 28±5% at 2 years, respectively (Image 2; p=0,395).
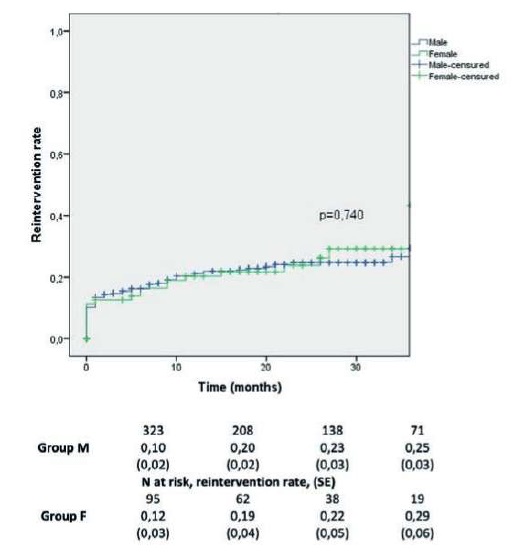
Vascular reintervention rates in Group M and Group F were 13±2% and 13±3% at 1 month, 21±2% and 20±4% at 1 year, and 25±3% and 24±5% at 2 years, respectively (Image 3; p=0,74).
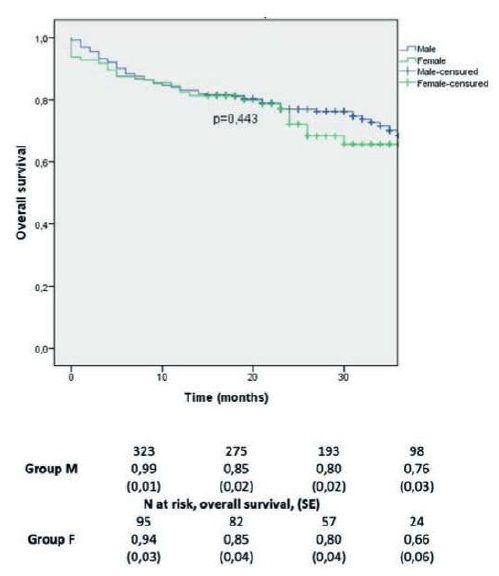
Overall survival in Group M and Group F was 97±1% and 93±3% at 1 month, 83±2% and 82±4% at 1 year, and 77±3% and 72±5% at 2 years, respectively (Image 4; p=0,443).
After group stratification according to the vascular procedure (open, endovascular or hybrid procedure) and according to the treated level affected by occlusive disease (inflow, outflow, or simultaneous inflow and outflow procedure), we found no significant difference between Groups M and F in the outcomes mentioned above (major amputation rate, diagnosed restenosis/occlusion procedure rate, reintervention rate, overall survival).
Discussion
Our study's main finding is that women and men have a similar prognosis after lower limb revascularization. Female patients who underwent lower limb revascularization tend to be older and have a more distal PAD distribution pattern. They undergo more frequent endovascular procedures and vascular procedures to treat outflow disease.
It has been suggested that, in women, there is a prolonged latent phase in the progression of PAD from asymptomatic to symptomatic. Notably, women tend to be older at the time of diagnosis than men, as in this study(1,3). Classic symptoms of PAD may be masked in this age group by increasing prevalence of osteoarthritis or a decrease in activity levels that occur with aging.
Other factors such as less physical activity and smaller calf muscle mass may also contribute to the delay in detecting PAD in women(1).
In Portugal, smoking is still more common in men(4). Increased smoking prevalence in Group M of this study may explain the increased burden of aortoiliac and CFA disease in male revascularized limbs, as smoking is associated with a proximal distribution of lower limb PAD(5).
The longer latent phase of PAD in women may lead to delayed diagnosis of PAD and greater risk of severe and complex anatomic disease burden(1-3). Below-knee arteries typically become increasingly involved as the overall severity of the disease worsens(5). Besides this, some authors state that women may be more prone to the development of FP disease(5). This can explain higher stages of BTK disease in Group F in this study. However, as PAD progresses, we should expect an increased prevalence of CLTI at presentation, and Groups F and M had similar CLTI prevalence.
Therefore, given the relative prevalence of asymptomatic PAD in women, early detection of asymptomatic PAD in this group can help control risk factors and inhibit disease progression(1).
In this study, women underwent endovascular and procedures to treat outflow disease more frequently than men. A possible explanation is the high experience of our vascular department on endovascular treatment of severe BTK disease. Other reasons may include the traditional belief that the female gender is associated with worse surgical outcomes, particularly after open procedures(1,2). These worse outcomes may be related to the above-mentioned older age of presentation, a smaller vessel size, a poorer overall health status, or a more severe clinical and anatomical disease burden at presentation in female patients(2).
On the other hand, some studies point out that endovascular intervention in females appears to be associated with better patency rates and better outcomes when compared with males(1,2).
After lower limb revascularization procedures, we found similar outcomes in males and females, even after stratifying by open, endovascular or hybrid procedures. Group F and M had no different rates of amputation, restenosis/occlusion and reintervention. There was also no difference in overall survival between groups. Ferranti et al. showed comparable results(3).
Despite similar outcomes in this study, Group F comprised only 23% of all revascularized lower limbs. In an analysis of 2.4 million PAD-related inpatient admissions, women were significantly less likely than men to receive a surgical revascularization procedure(6).
This study presents some limitations. It is dependent on appropriate medical records and patient clinical and imagiological follow-up. Department protocols do not include ankle-brachial index measurements, ankle pressure, or other parameters to evaluate ischemia grade in WIfI. Vascular procedure selection is dependent on surgeon experience. Power calculation was not produced to ascertain a sufficient sample size. Small sample size and lower prevalence of open, hybrid, inflow, and simultaneous inflow and outflow procedures on female limbs influence the statistical significance of outcomes differences. Gender-differences in baseline characteristics and in clinical grading and anatomic disease staging, if CLTI, may be confounding factors.
Conclusion
Overall, this study suggests no major difference in limb outcomes for women who undergo lower limb revascularization procedures. Women were more likely to be older, have more severe BTK disease, and undergo endovascular procedures. This absence of difference in outcomes may be explained by the high proportion of endovascular revascularization procedures due to CLTI in our population.
According to this study, we find no reason to expect worse limb outcomes in women.