Case Report
A 61-year-old man diagnosed with a pancreatic tumor, was submitted to a Whipple procedure and hemicolectomy. In the post-operative period, he developed a pancreatic fistula treated with octreotide. Patient was admitted in the emergency room, 9 days after discharge, with hemodynamic instability, fever and a spontaneous hematic drainage through previous drain incision.
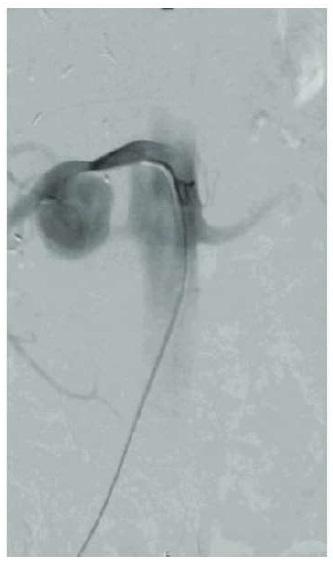
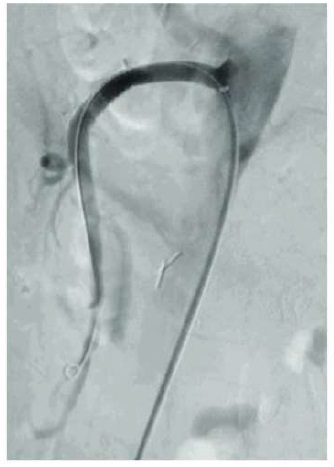
A surgical revision was performed, leaving an abdominal drainage, and meropenem was prescribed empirically. Four days after, he presented a spontaneous hematic drainage of 800 ml and persistent fever. Angio-CT scan revealed the rupture of a large pseudoaneurysm arising from the proximal portion of the superior mesenteric artery (SMA) (figure 1). The patient was immediately transferred to our center and forwarded to the angio suite. A selective SMA angiography confirmed the diagnosis. A 7×59mm stent graft (Advanta V12) was successfully deployed across the pseudoaneurysm, with immediate clinical and imagiological resolution (figure 2). On follow-up, patient maintained complete pseudoaneurysm exclusion and patency of the stent graft.
Discussion
Postoperative SMA pseudoaneurysm in the face of pancreatic surgery is a rare yet dangerous complication(1).
The formation of these pseudoaneurysms is attributed to the release of elastase, which leads to enzymatic autodigestion of adjacent arterial walls(2). Complications of pseudoaneurysms include rupture into the peritoneum, gastrointestinal tract, or rarely, the pancreatic duct. Intermittent gastrointestinal bleeding and crescendo-decrescendo abdominal pain may result. While early post-pancreatectomy hemorrhage occurs by definition within 24h from resection, delayed post-pancreatectomy hemorrhage can occur many days and even weeks later. In the described case, our patient presented with bleeding signs more than a week after surgery(3).
CT scan is currently the gold standard for diagnosis and in this case, the diagnosis was made in the emergency setting with a contrasted CT scan(4).
Delayed post-pancreatectomy hemorrhage represents to date a major cause of postoperative mortality(3); this complication is extremely difficult to manage because of the unstable clinical condition of the patients, wich deteriorates rapidly. In the past, surgical approach was considered the best treatment but it was associated with high rates of morbidity and mortality, besides the challenging postoperative adhesions and inflammation. These issues, have launched the endovascular approach as a less invasive, effective and safe technique with reduced morbi-mortality, when compared with open surgical care.
According to some reports, covered stent-grafts are associated with a diminished risk of recurrent hemorrhage when compared to selective embolization(5).Stent-graft deployment can lead to immediate exclusion of the pseudoaneurysm with a relatively short operative time. Moreover, stent graft implantation has been associated with a lower use of fluoroscopy during the procedure. Although it is a good treatment option, there are some associated complications, such as endoleaks and stent thromboses. Stent migration and consequent bleeding have also been described. Infection of the stent is another serious potential complication, which can happen when contact with gastrointestinal content or infected necrotic tissue occurs(6).
Vascular injuries after pancreatic surgery are associated with a significantly increased morbi-mortality. Early recognition and treatment are essential to optimize damage control and minimize complications. Whenever feasible, endovascular exclusion of a visceral artery pseudoaneurysm is a safe and effective technique with reduced morbi-mortality, when compared with open surgical care.