Introduction
Endovascular repair of the thoracic aorta (TEVAR) is now widely practiced, however, anatomic constrains (pathology of the ascending and transverse aortic arch) are common and can preclude stent grafting in a large percentage of cases1. Hybrid interventions combining the durability of an open ascending/aortic arch replacement with the less invasive endovascular treatment of the descending thoracic aorta (DTA) have been associated with good outcomes (true lumen expansion, malperfusion prevention/resolution and favorable aortic remodeling)2,3. Despite the existence of specific devices (E-Vita Open and E-Vita Open Plus® (Jotec® GmbH, Hechingen, Germany) and the Thoraflex™ Hybrid Prosthesis (Vascutek®, Terumo®, Inchinnan, Scotland, UK), they may not be available in good time in emergent cases that may require inventive solutions, like the case we present.
Case report
A 53-year-old male hypertensive, active smoker patient was transferred from another Institution due to an acute non-A-non-B aortic dissection (zone 2, extending to the abdominal aorta and left common iliac artery), complicated with haemopericardium and a contained rupture at the aortic isthmus with an associated left haemothorax (figure 1). No history of trauma was present.
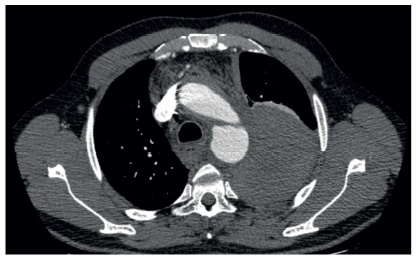
Figure 1 Admission angio CT demonstrating a contained rupture at the aortic isthmus with associated left haemothorax
Considering the absence of a secure proximal landing zone for a zone 2 deployment, the apparent involvement of the arch with hemopericardium description (risk of retrograde dissection), as well as the patient age and fitness, a decision was made for a hybrid procedure with a total aortic arch replacement and frozen stented elephant trunk using off-the-shelf devices. Procedure steps where as it follows. A 0.035 Terumo guidewire was introduced via right femoral artery (non-dissected iliac axis) within the true lumen, to the ascending aorta. Extra-corporeal circulation was established and cerebral perfusion secured through an 8 mm dacron graft anastomosed to the right axillary artery. Individual debranching of the innominate and left common carotid arteries was performed with 16×8 bifurcated dacron graft (distal anastomosis). Aortic arch replacement was then performed with a 28 mm woven polyester graft, under hypothermic circulatory arrest (approximate nasopharyngeal temperature of 24ºC): the distal anastomosis was first fashioned in zone 2 in a conventional elephant trunk fashion (with an excess of 6 cm of the dacron graft being gently pushed down to the DTA with an inflated Reliant balloon to guaranty adequate prosthetic overlap). The guidewire previously placed from the right femoral artery was recaptured in the aortic arch in a throught-and-throught fashion. Under direct vision and through the opened arch, a 30×30×157 mm endograft (Valiant Captivia, Medtronic Vascular, Santa Rosa, Calif) (10% oversize) was anterogradely advanced to the DTA over a stiff-wire with its proximal part parked at the level of the dacron anastomosis and fixated with interrupted, non-absorbable sutures to avoid future migrations (Figure 2).
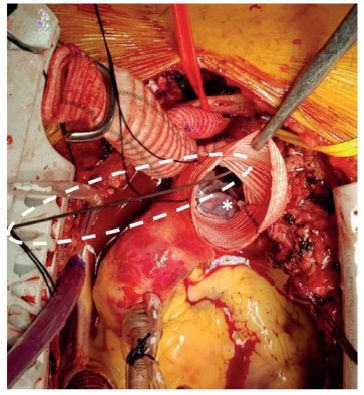
Figure 2 Intraoperative picture after TEVAR through the opened arch. The dotted line highlights the stiff guidewire through which the endoprosthesis (*) was anterogradely advanced to the DTA.
Proximal arch dacron anastomosis was completed at the level of the sinotubular junction. Proximal anastomosis of the bifurcated dacron graft and individual debranching of the left subclavian artery were performed. Figure 3 depicts the final intraoperative result.
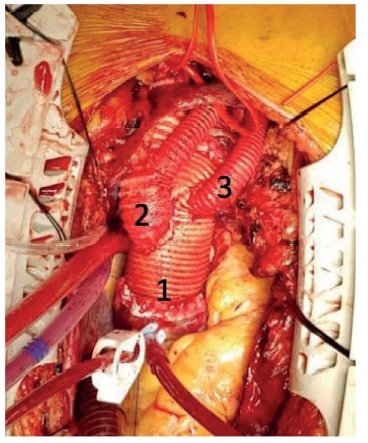
Figure 3 Final intraoperative result. 1: proximal zone 0 aortic anastomosis; 2: Individual debranching of the innominate and left common carotid arteries with 16x8 bifurcated dacron graft; 3: left subclavian artery debranching with an 8 mm dacron graft
Completion angiography demonstrated appropriately reconstructed aortic arch, successful exclusion of the entry tear and rupture site, as well as adequate renal and visceral branches perfusion. The patient had an uneventful postoperative course, being discharged on postoperative day 23. A control CTA prior to discharge demonstrated successful arch reconstruction, true lumen expansion, patent visceral branches and no signs of complications (Figure 4).
Discussion
The treatment of thoracic aortic pathology is in evolution. Anatomic constraints are common and preclude a TEVAR in a large percentage of patients.4 Hybrid approaches seeking to provide adequate proximal landing zones are now expanding the application of stent grafts and nowadays it is not a question of “open or endovascular” but “open and endovascular.”1 We report the case of a young and fit patient who presented with a complicated (rupture) acute non-A-non-B aortic dissection, without an adequate proximal landing zone, which we treated through an hybrid approach, in collaboration with cardiothoracic surgery. The “frozen elephant trunk” (FET) technique is a well-known operation and has been used to provide a secure proximal landing zone for a same-stage or second-stage DTA stent grafting5. This combination of techniques has been broadening the armamentarium of surgeons, allowing the treatment of complex arch/DTA pathology using of-the-shelf devices in a single-stage procedure like the one we describe. The conceptual strategy to obtain the most complete primary repair possible and to provide concomitant circumstances that facilitate any secondary future intervention is effective3.
In complicated aortic pathology, the primary focus of the treatment of this deadly disease is of course to promote immediate survival at the end of the surgical procedure. However, in young patients, to avoid reoperation on the remaining dissected proximal, descending thoracic, and thoracoabdominal aortas is also a concern5. The potential benefits of this intervention in acute aortic dissection are to (1) resect primary intimal tears beyond the ascending aorta, (2) resect or exclude re-entry tears in the distal aorta, (3) facilitate re-expansion of the distal true lumen and (4) promote false lumen obliteration. Ideally this approach would reduce early malperfusion, improve late aortic remodeling and decrease late mortality without increasing perioperative morbidity and mortality2. Favorable remodeling is particularly important in young patients with studies demonstrating that those submitted to stenting of the DTA had better remodeling and lower percentage of subsequent operations downstream of the thoracic aorta5. Spinal cord ischemia (SCI) is the Achilles heel of this procedure, and the incidence of new spinal cord injuries range from 1 to 21.7% in the literature with body core temperature greater than 28 °C in combination with a circulatory arrest time of more than 40 min and a distal landing zone lower than T10 being all associated with higher incidence of paraplegia3. In our case, we induced moderate hypothermia, cooling the patient to an approximate nasopharyngeal temperature of 24ºC. The total circulatory arrest time was of 27 minutes and the landing zone was above T7.
Some technical pearls are worth to discuss. Although we decided for an antegrade deployment, at the beginning of the operation a guidewire as introduced via right femoral artery. This had two main objectives: 1) secure that the stent graft was deployed within the true lumen; 2) to allow a controlled delivery of the stent graft with through-and-through wire access, avoiding any misdeployments or distal aortic perforations. The stent graft was sutured fixated to the dacron component to prevent future migration of the device. As we were dealing with a frail aorta, we aimed for an oversize of the stent graft of 10% to 15% larger than the long axis of the true lumen of the proximal descending thoracic aorta. Warm water was applied at the end of the stent deployment for full stent graft expansion because the deployment was performed during the hypothermic circulatory arrest period. The stent graft was then gently balloon-dilated to attain proper apposition against the aortic wall.
Conclusion
This hybrid approach with off-the-shelf devices was successful and avoided the cumulative morbidity of an additional left thoracotomy as well as the technical difficulty of a full open surgery in this setting. Open arch repair with an elephant trunk provided a proximal landing zone for a thoracic endograft. Further creative uses of these hybrid techniques will undoubtedly serve a larger role in the treatment of emergent thoracic aortic pathologies, providing an ever-widening option for the treatment aortic pathologies. The existence of an “aortic team” available to evaluate, decide and combine the expertise of cardiothoracic and vascular surgery was essential in this case.















