Introduction
Lower limb bypass grafting is often required in patients with chronic limb threatening ischemia. Patients with distal occlusive disease pattern - often diabetic or with end-stage renal disease - have occlusion of the tibio-peroneal vessels with sparing of femoropopliteal segment, posing a particularly challenging scenario for surgical revascularization. Autologous veins have proven to be superior to prosthetic grafts with better long-term results, making the ipsilateral greater saphenous veins (GSV) the preferred bypass conduite1; however, almost half the patients have unsuitable or unavailable GSV, making the contralateral GSV and spliced arm veins usually the second best choice2. The lesser saphenous veins (LSV) traditionally receives less protagonism as a possible conduit with few clinical cases reporting its use either reversed or in situ. Recently, Nierlich P. et al conducted a retrospective analysis of patients who underwent infrainguinal bypass using total or partial LSV as conduit; more than two thirds of these cases were in situ LSV bypasses. LSV was reported as a valuable alternative vein graft in peripheral bypass surgery achieving excellent long-term results both in primary and redo procedures3. In situ technique offers the potential advantages of decreased surgical trauma to the vein and its vasa vasorum, better size-matching between vein and artery at the anastomoses, and improved hemodynamics. The posterior approach simplifies distal vessels revascularization with inflow in the popliteal artery, requires less skin incisions and may reduce wound complications and post-operative lympedema4; it achieves similar graft patency and limb salvage rates compared to standard procedures3,4.
In this paper, we present the clinical case of an unusual, yet successful in situ popliteal to posterior tibial LSV bypass through a posterior approach.
Clinical case
An 89 year-old male patient is followed at the vascular surgery outpatient clinic with a nonhealing ulcer of the first toe of the right foot with ~18 months of evolution. His medical history includes diabetes mellitus for 45 years, arterial hypertension, dyslipidemia and benign prostatic hyperplasia. He underwent plain balloon angioplasty of the superficial femoral artery with unsuccessful recanalization of the posterior tibial and peroneal arteries two months before. On physical examination he had good, palpable popliteal pulse, but absent distal pulses and an unhealing first toe ulcer. Transcutaneous oxygen at the base of the first toe measured 6 mmHg. Lower limb angiography revealed extensive anterior tibial and peroneal occlusion with foot run-off through a patent and mildly diseased distal segment of the posterior tibial artery (figure 1). Given these findings, a popliteal to posterior tibial artery bypass was planned. Pre-operative ultrasonographic vein mapping revealed both GSV to be varicose and inadequate for bypass; however, ipsilateral LSV had a linear, ~3mm diameter, path to the ankle. After general anesthesia induction, the patient was laid in prone position, allowing a “lazy-S” popliteal incision to be made with simultaneous approach to both the retrogeniculate popliteal artery and LSV (figure 2). After systemic heparinization, LSV was ligated at its junction and rotated to be end-to-side anastomosed to the artery with a standard running 5/0 polypropylene suture. The posterior tibial artery was isolated through a retro-malleolar standard skin incision; the distal portion of the LSV was accessed and ligated with silk suture through a parallel incision over the Achilles tendon (figure 3). Valvulotomy was performed with a 2.5 and 3.0mm LeMaitre® valvulotome. After satisfactory arterial pulse was obtained at the distal LSV, this segment was subcutaneously rotated and end-to-end anastomosed to the posterior tibial artery with a standard running 7/0 polypropylene suture. Intra-operative ultrasound identified arteriovenous shunts that required ligation with a 3/0 silk suture. Final control angiography through femoral 4-French access showed patent bypass and run-off to the foot. Seven days after surgery, the bypass occluded requiring reintervention. The distal anastomosis skin incision was reopened and the culprit patent arteriovenous shunt, pre-operatively identified with ultrasound near the distal anastomosis, was ligated with 3/0 silk suture. The LSV was incised to allow the passage of a number 3 Fogarty balloon for thrombectomy and, afterwards, sutured again with a 7/0 polypropylene suture. Control angiography revealed a significant stenosis proximal to the distal anastomosis that was treated with a 2.0 mm plain balloon angioplasty, with rehabilitation of posterior tibial pulse (figure 4). During this procedure, the patient also underwent first toe amputation for necrosis control. The remaining postoperative evolution was uneventful. He was discharged 8 days after reintervention and maintains follow-up at the outpatient clinic: the bypass remains patent and skin lesions healing without complications.
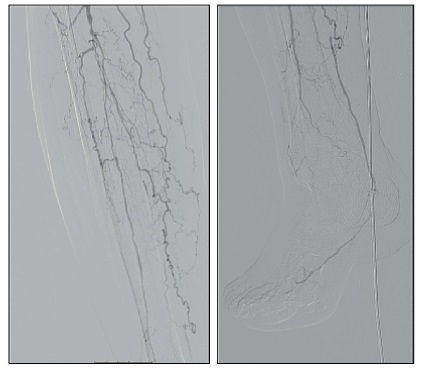
Figure 1 Right leg and foot angiogram revealing extensive occlusive disease with single run-off to the foot through a mildly diseased posterior tibial artery.
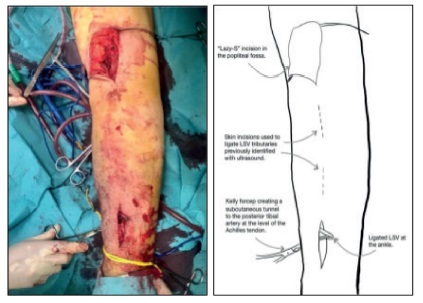
Figure 2 Proximal and distal exposures to control both the lesser saphenous vein (LSV) and the target arteries with the patient in prone position. In the right panel, the dashed lines represent the skin incisions used to ligate arteriovenous shunts identified with ultrasound after bypass anastomoses were completed.
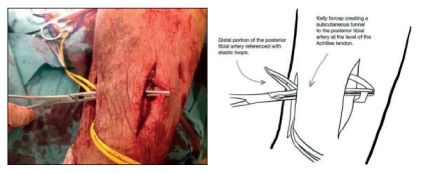
Figure 3 Zoomed-in distal exposure at the Achilles tendon level to control the distal portion of the LSV and the posterior tibial artery. A short subcutaneous tunnel was created to allow the distal anastomosis.
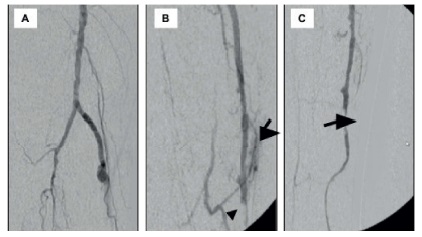
Figure 4 Angiography at the reintervention: A shows no stenosis at the proximal anastomosis; B shows the patent arteriovenous shunt (arrow) and distal vein thrombosis (arrowhead); C shows the vein stenosis proximal to the distal anastomosis (arrow) that was treated with 2.0mm plain balloon angioplasty
Discussion
Anatomic characteristics of LSV such as short length, small diameter and its posterior path in the leg usually discourage vascular surgeons to use it as an autologous conduit for lower limb bypasses. However, as many studies proved, when proper anatomy is present, it can be used as a viable option. Nierlich P. et al recently reported five year patency rates of 77% in infrainguinal bypasses using the LSV3. When GSV are not available, LSV may also offer better handling properties compared to arm veins; the latter are thin-walled with increased risk of lesions, need more incisions and often require splicing, resulting in worse outcomes4.
The posterior approach is a useful technique that simplifies distal vessels revascularization with inflow in the popliteal artery; it achieves similar graft patency and limb salvage rates compared to standard procedures5,6. Other potential benefits include less skin incisions to harvest the vein and fewer wound complications and lymphedema6. As shown in our clinical case, it allows adequate exposure of the popliteal and posterior tibial arteries; although not performed in this procedure, both peroneal and anterior tibial arteries can also be accessed through this approach.
In situ LSV bypass is a procedure performed less frequently, as it requires specific arterial and venous factors to its success. In fact, patients are required to have a disease-free femoropopliteal segment, at least one patent distal artery to the foot and a 2.5-3.0mm or more diameter LSV, lengthy enough to reach the target artery. Potential advantages of in situ technique are decreased trauma to the vein and its vasa vasorum, natural taper and better size-matching between vein and artery, which can ultimately lead to enhanced hemodynamics. On the other hand, complications that can lead to bypass thrombosis, include valve and intimal injury during valvulotomy as well as persistent arteriovenous shunts2; with intra-operative ultrasound both complications can be significantly reduced, reinforcing the role of ultrasound as an essential instrument to obtain better outcomes in vascular surgery.
Despite its potential benefits, there is still a lack of literature studying the outcomes of in situ LSV bypasses to distal arteries. Leather R. P. et al reported in situ techniques can achieve satisfactory patency rates: out of one thousand infrainguinal in situ bypasses with GSV and LSV, he reported 187 interventions to the distal tibial arteries with 1- and 5- year patency rates of 88% and 71%, respectively7. A different study reported 5-year primary and secondary patency rates of 52% and 89%, respectively, in distal bypasses using in situ LSV8.














